Neuropathies: Difference between revisions
mNo edit summary |
No edit summary |
||
| (16 intermediate revisions by 6 users not shown) | |||
| Line 2: | Line 2: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | |||
Neuropathies refer to a collection of disorders stemming from damage to the peripheral [[Neurone|nerves]], the vast communication network that sends signals between the [[Central Nervous System Pathways|central nervous system]](CNS) (the [[Brain Anatomy|brain]] and [[Spinal cord anatomy|spinal cord]]) and the rest of the body. Neuropathies can significantly impact patients' ability to perform daily activities, affecting functional independence and quality of life. | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
[[File:Neuron Part 1.png|right|frameless|500x500px]] | [[File:Neuron Part 1.png|right|frameless|500x500px]] | ||
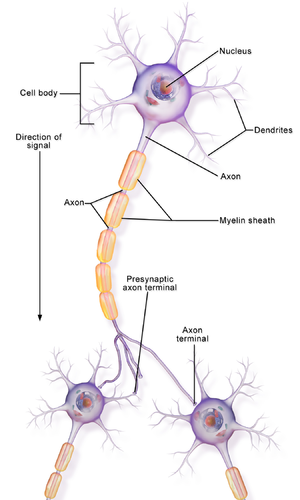
Peripheral | Peripheral nerves are intricate structures composed of nerve fibres ([[axons]]) and their covering, the myelin sheath. They transmit sensory information to the CNS, relay motor commands from the CNS to muscles, and manage autonomic functions like heart rate and digestion. Damage or dysfunction to these nerves manifests as neuropathies. | ||
To understand the extent and impact of such damage, neuropathies are commonly classified based on the number of nerves affected and their location: | |||
Peripheral | * Mononeuropathy: Involves damage to a single nerve. Examples include [[Carpal Tunnel Syndrome|carpal tunnel syndrome]] ([[Median Nerve|median nerve]]) or [[Common Peroneal Nerve|peroneal nerve]] palsy. | ||
* Polyneuropathy: Affects multiple peripheral nerves and often symmetrically. [[Diabetic Neuropathy|Diabetic neuropathy]] and [[HIV-related Neuropathy|HIV polyneuropathy]] is a common example.<ref>Said G. Diabetic neuropathy—a review. Nature clinical practice Neurology. 2007 Jun;3(6):331-40.</ref> | |||
* Mononeuritis Multiplex: Involves several nerves in random areas. This is typically due to multiple isolated nerve injuries and can be associated with conditions like vasculitis. | |||
* Autonomic Neuropathy: Targets the [[Autonomic Nervous System|autonomic nerves]], leading to issues with involuntary bodily functions such as [[Heart Rate|heart rate]], digestion, and bladder function. | |||
# Categorising them as mono-neuropathies, multifocal neuropathies, and poly-neuropathies. | |||
# Further sub-classifications can be made separating peripheral neuropathies as [[Axons|axonal]], [[Demyelinating Disorders|demyelinating]], or mixed, which is essential for treatment and management purposes. | |||
Peripheral neuropathy primarily presents with symptoms such as tingling sensations and numbness. Beyond these initial signs, affected individuals might also report pain, diminished muscle strength, and a lack of deep tendon [[reflexes]]. | |||
The progression and manifestation of these neuropathies can vary. Many develop gradually over the course of several years, while others might appear more abruptly, following a progressive course. Furthermore, the spectrum of clinical signs is broad due to the potential involvement of various nerve fibres, spanning motor, sensory, and autonomic functions.<ref name=":2">Hammi C, Yeung B. [https://www.ncbi.nlm.nih.gov/books/NBK542220/ Neuropathy.2019] Available from;https://www.ncbi.nlm.nih.gov/books/NBK542220/ (last accessed 5.9.2020)</ref> | |||
== Pathological Process == | == Pathological Process == | ||
The exact | When these peripheral nerves are damaged or diseased, their ability to transmit signals efficiently is compromised. The exact process can vary, but common features include axonal degeneration, demyelination, or both.<ref name=":2" /> | ||
== Aetiology == | |||
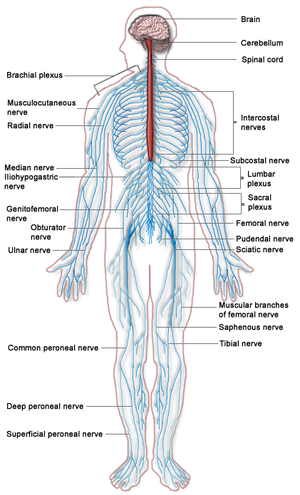
[[File:Nervous system diagram.png|495x495px|right|frameless]]Neuropathies, encompassing conditions marked by dysfunction or damage to the peripheral nerves, have a diverse range of causes. Understanding the origin is crucial not just for diagnosis but also to tailor the most effective treatment strategy. The causes can span from metabolic disruptions to genetic predispositions, from infections to physical traumas, and more. In some cases, a direct cause may not be apparent.<ref name=":2" /> | |||
* '''Metabolic/[[Endocrine Disorders|Endocrine]] Cause'''s: The most common being [[Diabetes|diabetes mellitus]], but nutritional deficiencies like B1, B6, [[Vitamin B12 Deficiency|B12]], and vitamin E also play a role. | |||
[[ | * '''Inflammatory Diseases''': Conditions such as [[Guillain-Barre Syndrome]], [https://medlineplus.gov/sjogrenssyndrome.html Sjogren's Syndrome], [[Systemic Lupus Erythematosus|Lupus]], [[Rheumatoid Arthritis|Rheumatoid Arthritis (RA)]], and vasculitis are prime examples. | ||
* '''Toxins and Drugs''': Some neuropathies occur secondary to the use of certain drugs or medications. This is caused by the toxic effect of these drugs which affects the axon or myelin sheath. There are various medications that are linked with neuropathies, with the most common being certain [[Antiretrovirals and HIV|antiretroviral]] drugs (especially NRTIs like zalcitabine and stavudine), [[Chemotherapy Side Effects and Syndromes|chemotherapy]] drugs (see [[Chemotherapy-Induced Peripheral Neuropathy (CIPN)|CIPN]]), antimicrobials (isoniazid, metronidazole), cardiovascular drugs (amiodarone), as well as certain illicit drugs.<ref>Jones MR, Urits I, Wolf J, Corrigan D, Colburn L, Peterson E, Williamson A, Viswanath O. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7365998/ Drug-induced peripheral neuropathy: a narrative review.] Current clinical pharmacology. 2020 Apr 1;15(1):38-48.</ref> | |||
* | * '''Hereditary Causes''': [[Charcot-Marie-Tooth Disease|Charcot-Marie-Tooth disease]] and familial [[amyloidosis]] are inherited conditions that lead to neuropathy. | ||
* '''Infections''': These can range from bacterial infections like [[Lyme Disease|Lyme disease]] (carried by ticks) to viral infections such as [[COVID-19|COVID 19]]<ref>Finsterer J, Scorza FA, Scorza CA, Fiorini AC. [https://pubmed.ncbi.nlm.nih.gov/34287509/ Peripheral neuropathy in COVID-19 is due to immune-mechanisms, pre-existing risk factors, anti-viral drugs, or bedding in the Intensive Care Unit.] Arquivos de neuro-psiquiatria. 2021 Jul 19;79:924-8.Available:https://pubmed.ncbi.nlm.nih.gov/34287509/ (accessed 18.8.2023)</ref>, chickenpox, Varicella zoster virus ([[Herpes Zoster|shingles]]), White Nile virus, [[Human Immunodeficiency Virus (HIV)|HIV]], [[Epstein-Barr Virus|Epstein-Barr virus]], and [[Hepatitis A, B, C|hepatitis C]]. | |||
* | * '''Trauma or pressure on the nerve''': Examples include [[Carpal Tunnel Syndrome|carpal tunnel syndrome]], physical injury like pressure from [[Disc Herniation|disc herniation]], pressure from a restrictive cast, direct trauma, and [[Arthritis|arthritic conditions]]. | ||
* '''Tumours''': Growths that either directly compress nerve fibres or are associated with [[Paraneoplastic Syndrome|paraneoplastic syndromes]]. Multiple myeloma, its treatments, and Monoclonal gammopathy of undetermined significance (MGUS) are related conditions that can cause neuropathic symptoms. | |||
* Trauma | |||
* [[ | |||
== Epidemiology == | == Epidemiology == | ||
[[File:Diabetic foot.jpg|right|frameless]]While neuropathies can affect people of all ages, certain types are more prevalent in specific groups. For instance, diabetic neuropathy predominantly impacts those with diabetes, and the risk increases with age and the duration of the disease. | |||
* Prevalence increases to 8.0% in older populations. | * Approx. 2.4% of the population is affected by peripheral nerve disorders. | ||
* [[Diabetic Neuropathy|Diabetic]] neuropathy occurs in approximately 50% of individuals with chronic type 1 and type 2 diabetes. | * Prevalence increases to 8.0% in older populations. | ||
* Globally, [[ | * [[Diabetic Neuropathy|Diabetic]] neuropathy occurs in approximately 50% of individuals with chronic type 1 and type 2 diabetes. | ||
* The most common genetic sensorimotor polyneuropathy is Charcot-Marie-Tooth disease, specifically, type 1a. | * Globally, [[leprosy]] remains a common cause of peripheral neuropathy, with the highest prevalence in South East Asia. | ||
* The most common genetic sensorimotor polyneuropathy is Charcot-Marie-Tooth disease, specifically, type 1a. | |||
* The most common mononeuropathy is [[Carpal Tunnel Syndrome|carpal tunnel syndrome]].<ref name=":2" /> | * The most common mononeuropathy is [[Carpal Tunnel Syndrome|carpal tunnel syndrome]].<ref name=":2" /> | ||
* HIV-related neuropathy affects up to 40% o HIV-infected individuals on ART.<ref>Winias S, Radithia D, Savitri Ernawati D. Neuropathy complication of antiretroviral therapy in HIV/AIDS patients. Oral Diseases. 2020 Sep;26:149-52.</ref> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Offene_Wunde_bei_einem_diabetischen_Fußsyndrom.jpg|thumb|An example of foot damage due to sensory loss]]Symptoms of neuropathies can range from numbness, tingling, and pain, to muscle weakness or paralysis. It is important to note that clinically, the symptoms of neuropathies can mimic those of other conditions like myelopathies, radiculopathies, autoimmune diseases, and muscle disorders. It's crucial for clinicians to differentiate neuropathies from these conditions for appropriate management. The precise manifestation will depend on the affected nerves: | |||
* Patients | |||
* '''Sensory Nerves''': Damage primarily leads to varied sensory symptoms. Patients often initially report disturbances in their digits, which can progress to their proximal limbs. This includes pain, tingling, numbness, heightened sensitivity, and changes in the ability to feel vibrations and touch. An individual might feel as though they're wearing gloves or stockings, an effect known as the "stocking-glove" pattern. The reduced ability to discern pain or temperature changes can result from damage to smaller sensory fibres, potentially impacting the patient's quality of life. Furthermore, there may be [[balance]] issues due to the loss of position sense. | |||
* '''[[Motor Neurone|Motor Nerves]]''': Symptoms related to motor nerve damage are predominantly muscular in nature. This includes muscle weakness, painful cramps, fasciculations (visible uncontrolled muscle twitching) and muscle atrophy. Advanced stages of neuropathy can exhibit reduced or even absent deep tendon reflexes, indicative of both sensory and motor nerve damage. | |||
* '''Autonomic Nerves''': Autonomic nerve symptoms arise due to the impairment of axons in small-fibre neuropathies. This can manifest as excessive sweating, heat intolerance, issues with blood vessel regulation affecting blood pressure, and a range of gastrointestinal symptoms.<ref name=":0">NIH [https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet Peripheral neuropathy fact sheet.] Available from: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet (last accessed 18 April 2019)</ref> | |||
* | |||
* | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
[[File:Blood testing.jpg|right|frameless]] | [[File:Blood testing.jpg|right|frameless]] | ||
The diagnosis of neuropathies is multifaceted, involving a combination of clinical examinations and advanced testing methods. By pinpointing the underlying cause and understanding the extent of nerve damage, clinicians can make informed decisions regarding the patient's care.<ref name=":1">Mayo clinic. [https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067 Peripheral neuropathy.] Available from: https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067 (last accessed 18 April 2019)</ref> | |||
* '''Physical Examination''': This involves testing reflexes, gauging [[Muscle Strength Testing|muscle strength]], and conducting sensory tests to assess the patient's neurological function. | |||
* '''[[Blood Tests]]''': These can be instrumental in uncovering conditions like diabetes that might be contributing to the neuropathy. | |||
* '''Nerve Function Tests''': Tools such as [[Electromyogram|Electromyography (EMG)]] and nerve conduction studies delve into the electrical activity and transmission capability of the nerves. | |||
* '''Imaging Tests''': [[MRI Scans|MRI]] or [[CT Scans|CT scans]] provide detailed views of bodily structures, helping to identify any physical causes of nerve distress. | |||
* '''Nerve Biopsy''': In select cases, examining a small segment of the nerve directly can offer invaluable insights. | |||
== Outcome Measures == | == Outcome Measures == | ||
Effective management of neuropathies requires consistent monitoring and evaluation. By using specific outcome measures, it is possible to monitor the progression of the condition and the impact of therapeutic interventions. Tests are usually related to [[muscle]] strength, [[Pain Behaviours|pain]], [[Quality of Life|QOL]], and activity limitations. They include: | |||
* The [[36-Item Short Form Survey (SF-36)|SF-36]] is a measure of health status and an abbreviated variant of it, the SF-6D, is commonly used in health economics as a variable in the quality-adjusted life year calculation to determine the cost-effectiveness of a health treatment.<ref>Wikipedia. SF-36 Available from: https://en.wikipedia.org/wiki/SF-36 (last accessed 19 April 2019)</ref> | * The [[36-Item Short Form Survey (SF-36)|SF-36]] is a measure of health status and an abbreviated variant of it, the SF-6D, is commonly used in health economics as a variable in the quality-adjusted life year calculation to determine the cost-effectiveness of a health treatment.<ref>Wikipedia. SF-36 Available from: https://en.wikipedia.org/wiki/SF-36 (last accessed 19 April 2019)</ref> | ||
* INCAT (inflammatory cause and treatment) score is a measure of activity limitation | * INCAT (inflammatory cause and treatment) score is a measure of activity limitation | ||
* [[Timed Up and Go Test (TUG)|TUG]]; [[10 Metre Walk Test|10 metre walk test]]; [[Grip Strength]]; [[Fatigue Severity Scale|Fatigue Severity Scale;]] [[Patient Specific Functional Scale]]; [[Muscle Strength Testing|Oxford Muscle Strength Scale]]; [[Romberg Test|Romberg Test]]. | * [[Timed Up and Go Test (TUG)|TUG]]; [[10 Metre Walk Test|10 metre walk test]]; [[Grip Strength]]; [[Fatigue Severity Scale|Fatigue Severity Scale;]] [[Patient Specific Functional Scale]]; [[Muscle Strength Testing|Oxford Muscle Strength Scale]]; [[Romberg Test|Romberg Test]]. | ||
* '''[[Neuropathic Pain|Neuropathic pain]]''' measures: [[PainDETECT]], [[DN4 questionnaire|DN4]], [[Leeds Assessment of Neuropathic Symptoms and Signs (LANSS)|LANSS]] | |||
== Treatment == | == Treatment == | ||
The cornerstone of neuropathy treatment revolves around addressing the root cause, alleviating symptoms, and restoring optimal function. A comprehensive treatment plan often combines pharmacological and therapeutic interventions. It is important to note not all neuropathies are reversible.<ref name=":2" /><ref name=":1" /> | |||
' | * Medication: This might include pain relievers, anti-seizure medications, or antidepressants tailored to the patient's specific symptoms. Chronic inflammatory demyelinating neuropathy is treated using [[Corticosteroid Medication|corticosteroids]] initially, but can also be treated using intravenous [[Immunoglobulins (Ig)|immunoglobulin]], plasma exchange, and some immunosuppressant drugs. | ||
* Therapies: Approaches such as physiotherapy or [[Transcranial Electrical Nerve Stimulation for Dementia|TENS]] offer non-invasive means to manage symptoms.<ref name=":2" /> | |||
* Surgical and Other Procedures: Certain neuropathies, particularly those arising from physical pressure, might necessitate surgical interventions. | |||
* Glucose control in diabetic neuropathy, alcohol cessation in [[Alcoholism|alcoholic]] neuropathy. | |||
* [[Nutrition|Nutritional]] deficiencies can have therapy with supplementation of the depleted vitamins or minerals. | |||
== Physiotherapy == | |||
[[ | |||
[[File:Exercise group.jpg|right|frameless]] | [[File:Exercise group.jpg|right|frameless]] | ||
The | [[Nerve Injury Rehabilitation|Physiotherapy]] is an important therapy intervention for people with neuropathies. Through individualised treatment plans and interventions, it aims to improve movement and relieve pain and discomfort. The scope of these interventions ranges from strengthening exercises designed to address muscle weakness, to balance exercises that address fall risks. Some common interventions include: | ||
* Restore, or maintain muscle strength, and prevent muscle shortening and deformity | * Restore, or maintain muscle strength, and prevent muscle shortening and deformity | ||
* [[Balance]], coordination and functional training. | * [[Balance]], coordination and functional training. | ||
| Line 100: | Line 87: | ||
* Education, re-managing conditions, preventing damage and emotional support. | * Education, re-managing conditions, preventing damage and emotional support. | ||
For a comprehensive guide see individual neuropathies below | For a comprehensive guide see individual neuropathies below | ||
* [[HIV/ | * [[HIV-related Neuropathy|HIV/AIDS]] | ||
* [[Anterior Interosseous Nerve Syndrome]] | * [[Anterior Interosseous Nerve Syndrome]] | ||
* [[Axillary Nerve Injury|Axillary Nerve Injury]] | * [[Axillary Nerve Injury|Axillary Nerve Injury]] | ||
| Line 116: | Line 103: | ||
* [[Nerve entrapment|Nerve Entrapment]] | * [[Nerve entrapment|Nerve Entrapment]] | ||
* [[Posterior Interosseous Nerve Syndrome|Posterior Interosseous Nerve Syndrome]] | * [[Posterior Interosseous Nerve Syndrome|Posterior Interosseous Nerve Syndrome]] | ||
* [[Saturday Night Palsy]] | |||
* [[Sciatic Nerve Injury|Sciatic Nerve Injury]] | * [[Sciatic Nerve Injury|Sciatic Nerve Injury]] | ||
* [[Thoracic Radiculopathy]] | * [[Thoracic Radiculopathy]] | ||
* [[Ulnar Nerve Entrapment]] | * [[Ulnar Nerve Entrapment]] | ||
== The Multidisciplinary Team approach to Rehabilitation == | |||
Managing neuropathies requires more than a singular approach; it calls for a holistic, cohesive strategy that draws on the strengths of various healthcare professionals. At the forefront of this multi-disciplinary team approach are occupational therapists, who play a pivotal role. With their in-depth expertise, they guide patients towards achieving a better quality of daily life. The scope of their contribution is vast, from modifying and adapting how patients engage in [[Activities of Daily Living|Activities of Daily Living (ADLs)]] to introducing sensory re-education techniques. These techniques are specially designed to refine and improve a patient's sensory perception, helping them navigate the challenges posed by neuropathies with greater ease and confidence. | |||
== Prognosis == | == Prognosis == | ||
In | Neuropathy outcomes are deeply influenced by the underlying cause. In conditions where peripheral nerves are damaged through Wallerian or axonal degeneration, recovery is challenging. For improvement, the nerve must regenerate its axon and reconnect with the affected muscles or organs. However, neuropathies resulting from segmental demyelination often have a more favourable prognosis due to the quicker process of remyelination, which facilitates the axon's functional return. | ||
Complications from neuropathies can vary, from pain and altered sensations to muscle atrophy and weakness. Diabetic peripheral neuropathy, for instance, can lead to severe complications like foot ulcers, which in some cases escalate to gangrenous conditions and amputations. | |||
Regardless of the type and complications, early intervention typically results in a better prognosis. While some patients find relief with treatments, others require long-term management.<ref name=":2" /> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Neurology]] | |||
[[Category:Neurological - Conditions]] | |||
[[Category:Neuropathy]] | |||
Latest revision as of 13:24, 13 December 2023
Top Contributors - Lucinda hampton, Kim Jackson, Candace Goh, Melissa Coetsee, Uchechukwu Chukwuemeka, Sehriban Ozmen, Manisha Shrestha, Merinda Rodseth and Ahmed M Diab
Introduction[edit | edit source]
Neuropathies refer to a collection of disorders stemming from damage to the peripheral nerves, the vast communication network that sends signals between the central nervous system(CNS) (the brain and spinal cord) and the rest of the body. Neuropathies can significantly impact patients' ability to perform daily activities, affecting functional independence and quality of life.
Clinically Relevant Anatomy[edit | edit source]
Peripheral nerves are intricate structures composed of nerve fibres (axons) and their covering, the myelin sheath. They transmit sensory information to the CNS, relay motor commands from the CNS to muscles, and manage autonomic functions like heart rate and digestion. Damage or dysfunction to these nerves manifests as neuropathies.
To understand the extent and impact of such damage, neuropathies are commonly classified based on the number of nerves affected and their location:
- Mononeuropathy: Involves damage to a single nerve. Examples include carpal tunnel syndrome (median nerve) or peroneal nerve palsy.
- Polyneuropathy: Affects multiple peripheral nerves and often symmetrically. Diabetic neuropathy and HIV polyneuropathy is a common example.[1]
- Mononeuritis Multiplex: Involves several nerves in random areas. This is typically due to multiple isolated nerve injuries and can be associated with conditions like vasculitis.
- Autonomic Neuropathy: Targets the autonomic nerves, leading to issues with involuntary bodily functions such as heart rate, digestion, and bladder function.
- Categorising them as mono-neuropathies, multifocal neuropathies, and poly-neuropathies.
- Further sub-classifications can be made separating peripheral neuropathies as axonal, demyelinating, or mixed, which is essential for treatment and management purposes.
Peripheral neuropathy primarily presents with symptoms such as tingling sensations and numbness. Beyond these initial signs, affected individuals might also report pain, diminished muscle strength, and a lack of deep tendon reflexes.
The progression and manifestation of these neuropathies can vary. Many develop gradually over the course of several years, while others might appear more abruptly, following a progressive course. Furthermore, the spectrum of clinical signs is broad due to the potential involvement of various nerve fibres, spanning motor, sensory, and autonomic functions.[2]
Pathological Process[edit | edit source]
When these peripheral nerves are damaged or diseased, their ability to transmit signals efficiently is compromised. The exact process can vary, but common features include axonal degeneration, demyelination, or both.[2]
Aetiology[edit | edit source]
Neuropathies, encompassing conditions marked by dysfunction or damage to the peripheral nerves, have a diverse range of causes. Understanding the origin is crucial not just for diagnosis but also to tailor the most effective treatment strategy. The causes can span from metabolic disruptions to genetic predispositions, from infections to physical traumas, and more. In some cases, a direct cause may not be apparent.[2]
- Metabolic/Endocrine Causes: The most common being diabetes mellitus, but nutritional deficiencies like B1, B6, B12, and vitamin E also play a role.
- Inflammatory Diseases: Conditions such as Guillain-Barre Syndrome, Sjogren's Syndrome, Lupus, Rheumatoid Arthritis (RA), and vasculitis are prime examples.
- Toxins and Drugs: Some neuropathies occur secondary to the use of certain drugs or medications. This is caused by the toxic effect of these drugs which affects the axon or myelin sheath. There are various medications that are linked with neuropathies, with the most common being certain antiretroviral drugs (especially NRTIs like zalcitabine and stavudine), chemotherapy drugs (see CIPN), antimicrobials (isoniazid, metronidazole), cardiovascular drugs (amiodarone), as well as certain illicit drugs.[3]
- Hereditary Causes: Charcot-Marie-Tooth disease and familial amyloidosis are inherited conditions that lead to neuropathy.
- Infections: These can range from bacterial infections like Lyme disease (carried by ticks) to viral infections such as COVID 19[4], chickenpox, Varicella zoster virus (shingles), White Nile virus, HIV, Epstein-Barr virus, and hepatitis C.
- Trauma or pressure on the nerve: Examples include carpal tunnel syndrome, physical injury like pressure from disc herniation, pressure from a restrictive cast, direct trauma, and arthritic conditions.
- Tumours: Growths that either directly compress nerve fibres or are associated with paraneoplastic syndromes. Multiple myeloma, its treatments, and Monoclonal gammopathy of undetermined significance (MGUS) are related conditions that can cause neuropathic symptoms.
Epidemiology[edit | edit source]
While neuropathies can affect people of all ages, certain types are more prevalent in specific groups. For instance, diabetic neuropathy predominantly impacts those with diabetes, and the risk increases with age and the duration of the disease.
- Approx. 2.4% of the population is affected by peripheral nerve disorders.
- Prevalence increases to 8.0% in older populations.
- Diabetic neuropathy occurs in approximately 50% of individuals with chronic type 1 and type 2 diabetes.
- Globally, leprosy remains a common cause of peripheral neuropathy, with the highest prevalence in South East Asia.
- The most common genetic sensorimotor polyneuropathy is Charcot-Marie-Tooth disease, specifically, type 1a.
- The most common mononeuropathy is carpal tunnel syndrome.[2]
- HIV-related neuropathy affects up to 40% o HIV-infected individuals on ART.[5]
Clinical Presentation[edit | edit source]
Symptoms of neuropathies can range from numbness, tingling, and pain, to muscle weakness or paralysis. It is important to note that clinically, the symptoms of neuropathies can mimic those of other conditions like myelopathies, radiculopathies, autoimmune diseases, and muscle disorders. It's crucial for clinicians to differentiate neuropathies from these conditions for appropriate management. The precise manifestation will depend on the affected nerves:
- Sensory Nerves: Damage primarily leads to varied sensory symptoms. Patients often initially report disturbances in their digits, which can progress to their proximal limbs. This includes pain, tingling, numbness, heightened sensitivity, and changes in the ability to feel vibrations and touch. An individual might feel as though they're wearing gloves or stockings, an effect known as the "stocking-glove" pattern. The reduced ability to discern pain or temperature changes can result from damage to smaller sensory fibres, potentially impacting the patient's quality of life. Furthermore, there may be balance issues due to the loss of position sense.
- Motor Nerves: Symptoms related to motor nerve damage are predominantly muscular in nature. This includes muscle weakness, painful cramps, fasciculations (visible uncontrolled muscle twitching) and muscle atrophy. Advanced stages of neuropathy can exhibit reduced or even absent deep tendon reflexes, indicative of both sensory and motor nerve damage.
- Autonomic Nerves: Autonomic nerve symptoms arise due to the impairment of axons in small-fibre neuropathies. This can manifest as excessive sweating, heat intolerance, issues with blood vessel regulation affecting blood pressure, and a range of gastrointestinal symptoms.[6]
Diagnostic Procedures[edit | edit source]
The diagnosis of neuropathies is multifaceted, involving a combination of clinical examinations and advanced testing methods. By pinpointing the underlying cause and understanding the extent of nerve damage, clinicians can make informed decisions regarding the patient's care.[7]
- Physical Examination: This involves testing reflexes, gauging muscle strength, and conducting sensory tests to assess the patient's neurological function.
- Blood Tests: These can be instrumental in uncovering conditions like diabetes that might be contributing to the neuropathy.
- Nerve Function Tests: Tools such as Electromyography (EMG) and nerve conduction studies delve into the electrical activity and transmission capability of the nerves.
- Imaging Tests: MRI or CT scans provide detailed views of bodily structures, helping to identify any physical causes of nerve distress.
- Nerve Biopsy: In select cases, examining a small segment of the nerve directly can offer invaluable insights.
Outcome Measures[edit | edit source]
Effective management of neuropathies requires consistent monitoring and evaluation. By using specific outcome measures, it is possible to monitor the progression of the condition and the impact of therapeutic interventions. Tests are usually related to muscle strength, pain, QOL, and activity limitations. They include:
- The SF-36 is a measure of health status and an abbreviated variant of it, the SF-6D, is commonly used in health economics as a variable in the quality-adjusted life year calculation to determine the cost-effectiveness of a health treatment.[8]
- INCAT (inflammatory cause and treatment) score is a measure of activity limitation
- TUG; 10 metre walk test; Grip Strength; Fatigue Severity Scale; Patient Specific Functional Scale; Oxford Muscle Strength Scale; Romberg Test.
- Neuropathic pain measures: PainDETECT, DN4, LANSS
Treatment[edit | edit source]
The cornerstone of neuropathy treatment revolves around addressing the root cause, alleviating symptoms, and restoring optimal function. A comprehensive treatment plan often combines pharmacological and therapeutic interventions. It is important to note not all neuropathies are reversible.[2][7]
- Medication: This might include pain relievers, anti-seizure medications, or antidepressants tailored to the patient's specific symptoms. Chronic inflammatory demyelinating neuropathy is treated using corticosteroids initially, but can also be treated using intravenous immunoglobulin, plasma exchange, and some immunosuppressant drugs.
- Therapies: Approaches such as physiotherapy or TENS offer non-invasive means to manage symptoms.[2]
- Surgical and Other Procedures: Certain neuropathies, particularly those arising from physical pressure, might necessitate surgical interventions.
- Glucose control in diabetic neuropathy, alcohol cessation in alcoholic neuropathy.
- Nutritional deficiencies can have therapy with supplementation of the depleted vitamins or minerals.
Physiotherapy[edit | edit source]
Physiotherapy is an important therapy intervention for people with neuropathies. Through individualised treatment plans and interventions, it aims to improve movement and relieve pain and discomfort. The scope of these interventions ranges from strengthening exercises designed to address muscle weakness, to balance exercises that address fall risks. Some common interventions include:
- Restore, or maintain muscle strength, and prevent muscle shortening and deformity
- Balance, coordination and functional training.
- Pain relief e.g. provision of TENS, massage
- Splints as needed, prevent deformity and contractures
- Education, re-managing conditions, preventing damage and emotional support.
For a comprehensive guide see individual neuropathies below
- HIV/AIDS
- Anterior Interosseous Nerve Syndrome
- Axillary Nerve Injury
- Brachial Plexus Injury
- Benediction Hand
- Carpal Tunnel Syndrome
- Charcot Marie Tooth Disease
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
- Cubital Tunnel Syndrome
- Cyclist's Palsy
- Diabetic Neuropathy
- Double Crush Syndrome
- Lumbar Radioculopathy
- Multifocal Motor Neuropathy
- Nerve Entrapment
- Posterior Interosseous Nerve Syndrome
- Saturday Night Palsy
- Sciatic Nerve Injury
- Thoracic Radiculopathy
- Ulnar Nerve Entrapment
The Multidisciplinary Team approach to Rehabilitation[edit | edit source]
Managing neuropathies requires more than a singular approach; it calls for a holistic, cohesive strategy that draws on the strengths of various healthcare professionals. At the forefront of this multi-disciplinary team approach are occupational therapists, who play a pivotal role. With their in-depth expertise, they guide patients towards achieving a better quality of daily life. The scope of their contribution is vast, from modifying and adapting how patients engage in Activities of Daily Living (ADLs) to introducing sensory re-education techniques. These techniques are specially designed to refine and improve a patient's sensory perception, helping them navigate the challenges posed by neuropathies with greater ease and confidence.
Prognosis[edit | edit source]
Neuropathy outcomes are deeply influenced by the underlying cause. In conditions where peripheral nerves are damaged through Wallerian or axonal degeneration, recovery is challenging. For improvement, the nerve must regenerate its axon and reconnect with the affected muscles or organs. However, neuropathies resulting from segmental demyelination often have a more favourable prognosis due to the quicker process of remyelination, which facilitates the axon's functional return.
Complications from neuropathies can vary, from pain and altered sensations to muscle atrophy and weakness. Diabetic peripheral neuropathy, for instance, can lead to severe complications like foot ulcers, which in some cases escalate to gangrenous conditions and amputations.
Regardless of the type and complications, early intervention typically results in a better prognosis. While some patients find relief with treatments, others require long-term management.[2]
References[edit | edit source]
- ↑ Said G. Diabetic neuropathy—a review. Nature clinical practice Neurology. 2007 Jun;3(6):331-40.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Hammi C, Yeung B. Neuropathy.2019 Available from;https://www.ncbi.nlm.nih.gov/books/NBK542220/ (last accessed 5.9.2020)
- ↑ Jones MR, Urits I, Wolf J, Corrigan D, Colburn L, Peterson E, Williamson A, Viswanath O. Drug-induced peripheral neuropathy: a narrative review. Current clinical pharmacology. 2020 Apr 1;15(1):38-48.
- ↑ Finsterer J, Scorza FA, Scorza CA, Fiorini AC. Peripheral neuropathy in COVID-19 is due to immune-mechanisms, pre-existing risk factors, anti-viral drugs, or bedding in the Intensive Care Unit. Arquivos de neuro-psiquiatria. 2021 Jul 19;79:924-8.Available:https://pubmed.ncbi.nlm.nih.gov/34287509/ (accessed 18.8.2023)
- ↑ Winias S, Radithia D, Savitri Ernawati D. Neuropathy complication of antiretroviral therapy in HIV/AIDS patients. Oral Diseases. 2020 Sep;26:149-52.
- ↑ NIH Peripheral neuropathy fact sheet. Available from: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet (last accessed 18 April 2019)
- ↑ 7.0 7.1 Mayo clinic. Peripheral neuropathy. Available from: https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067 (last accessed 18 April 2019)
- ↑ Wikipedia. SF-36 Available from: https://en.wikipedia.org/wiki/SF-36 (last accessed 19 April 2019)