Lyme Disease
Original Editors - Kevin Beale from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kevin Beale, Morgan Fife, Kim Jackson, Elaine Lonnemann, Admin, Wendy Walker, Lucinda hampton, Jack Nicholson, Erin Shinkle, Evan Thomas, Scott Buxton, Naomi O'Reilly and WikiSysop
Definition/Description[edit | edit source]

Lyme disease or Lyme borreliosis is the most commonly transmitted tick-borne infection in the United States and among the most frequently diagnosed tick-borne infections worldwide. Lyme disease is divided into three stages[1]:
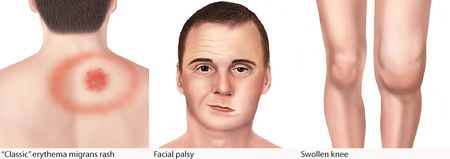
- Early localized - distinguished by the red ring-like expanding rash of Erythema migrans at the site of a recent tick bite. Other symptoms experienced at this stage may be flu-like symptoms, malaise, headache, fever, myalgia, and arthralgia.
- Early disseminated - About 20% of patients develop the early disseminated disease, with the most common symptoms being multiple erythema migrans lesions. Other symptoms of the disseminated stage are flu-like symptoms, lymphadenopathy, arthralgia, myalgia, palsies of the cranial nerves (especially CN-VII which results in Facial Palsy), ophthalmic conditions, and lymphocytic meningitis. Additionally, cardiac manifestations such as conduction abnormalities, myocarditis, or pericarditis may occur.
- Late - The most common manifestation of the late disease is arthritis that is usually pauciarticular and affects large joints, especially the knees
Lyme disease was initially identified in young children in Lyme, Connecticut in 1976. They first recognized the “bulls-eye” rash and an atypical type of arthritis in these children. In 1982 they recognized the relationship between the children with a history of tick bites and the infection when the Borrelia organism was found from an individual affected with Lyme disease. [2]
The Australian Government Department of health states[3] "the concept of chronic Lyme disease is disputed and not accepted by most conventional medical practitioners, not only in Australia but around the world". Australia recognises the existence of classical Lyme disease which is found in high rates in endemic areas (mainly the northeast of the USA, some areas of Europe including the UK and some parts of Asia). Australians can be infected in these endemic areas and bring the infection to Australia. Because there is no person-to-person transmission of classical Lyme disease, the risk to Australia and Australians is low.
Prevalence[edit | edit source]
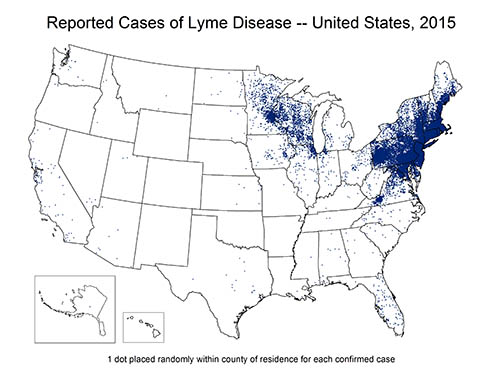
According to the CDC's collection of data from identified cases of Lyme disease counts by each county in the United States, there were 201,923 cases of Lyme disease reported from 2010 to 2015. The incidence of Lyme disease has fluctuated over the years, however still showing a steady increase from 30,158 confirmed cases in 2010 to 38,069 confirmed cases in 2015. Lyme disease is the most prevalent vector-bourne illness reported in the United States, according to date from the CDC.
Of those cases reported, 95% of confirmed Lyme disease cases were reported from 14 states: Connecticut, Delaware, Maine, Maryland, Massachusetts, Minnesota, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont, Virginia, and Wisconsin. Lyme disease is primarily found in the Upper Midwest and Northeastern states of the United States, where deer and black-legged ticks are most common. [2]
Most cases develop during the summer months of May through August when individuals are more likely to visit wooded areas for work or recreation and tick nymphs are most active. [4]Children 5 to 14 years of age have the highest rate of incidence with an average of 8.6 cases per 100,000 compared to 3.0 cases per 100,000 for people 20 to 24 and 7.8 cases per 100,000 for ages 55 to 59.[5] .
Characteristics/Clinical Presentation[edit | edit source]
Like syphilis, Lyme is classified into 3 stages: localized, disseminated and persistent. The first two stages are part of early infection and the third stage is part of persistent or chronic disease. Stage 3 usually occurs within 12 months of the infection.[1]
- Stage 1: Localized disease associated with erythema migrans and flu-like symptoms; Duration 1 to 30 days
- Stage 2: Early disseminated disease with malaise, pain, and flu-like symptoms; May affect the neurological, ocular, and musculoskeletal organs; Duration 3 to 10 weeks
- Stage 3: Late or chronic disease chiefly affects the joints, muscles, and nerves, May last months or years, Lyme arthritis is a hallmark of this stage.
- The occurrence of post-treatment Lyme syndrome is debatable.
Localized Lyme disease is characterized by erythema migrans occurring 1 to 2 weeks after tick exposure in an endemic area. The differential diagnosis for early Lyme disease with erythema migrans includes other skin conditions such as tinea and nummular eczema. If not treated in the localized stage, patients may go on to develop early disseminated or late disease manifestations. Early neurologic Lyme disease manifestations include Facial Nerve (CN-VII) palsy, lymphocytic meningitis, or radiculopathy. Cardiac involvement includes myopericarditis and typically presents with heart block. Lyme arthritis is mono- or pauciarticular, generally involving large joints, most commonly the knee, and occurring months removed from the initial tick bite.
Stage 1: Early localized disease that may present with erythema migrans and alow grade fever. This stage usually occurs within 1-28 days following the tick bite.
- A classic rash is seen in 70% of patients and may develop between 5-7 days following the tick bite. The uniform rash usually occurs at the site of the tick bite, may burn, itch or be asymptomatic. The rash tends to expand for a few days and concentric rings may be visible. If left untreated, the rash persists for 2-3 weeks.
- About 20% may have recurrent episodes of the rash and multiple lesions are not uncommon.
- Flu-like symptoms may be present. The fever is low grade and may be associated with myalgia, neck stiffness and headache.
- Visual problems include eye redness and tearing.
- About 30% of patients with the rash will have no further progression of symptoms.
Stage 2: Usually develops 3-12 weeks after the initial infection and may last 12-20 weeks, but recurrence is rare. Features may include
- General malaise,
- Fever
- Neurological features (dizziness, headache)
- Muscle pain
- Cardiac symptoms (chest pain, palpitations, and dyspnea)
- Cranial neuropathy may present as diplopia, eye pain and keratitis have also been reported.
- Knee, ankle and wrist joint are often involved. Often when a single joint is involved, it may be mistaken for septic arthritis
- About 20% of patients have CNS involvement including encephalopathy, meningitis and cranial nerve neuropathy. Facial palsy is seen in about 5% of patients. When meningeal symptoms are present, a lumbar puncture may rule out other causes.
- Encephalopathy presents with deficits in concentration, cognition, memory loss and changes in personality. Extreme irritability and depression are also common.
Borrelia lymphocytoma is a rare presentation of early Lyme disease that has been reported in Europe. It presents as a nodular red-bluish swelling that usually occurs on the ear lobe or areola of the nipple. The lesions can be painful to touch.
Stage 3: Late Lyme disease may occur many months or years after the initial infection. Features include
- Neurological and rheumatological involvement.
- Patients may not have a history of erythema migrans.
- May present with aseptic meningitis, Bell palsy, arthritis or dysesthesias.
- Cognitive deficits are common
- The key feature of late-stage Lyme is arthritis which tends to affect the knee and neurological and psychiatric symptoms mimic fibromyalgia.
- Radicular pain is common.
- Borrelia encephalomyelitis is rare and can present with ataxia, seizures, hemiparesis, autonomic dysfunction and hearing loss.
- Acrodermatitis chronica atrophicans is typically seen in older women and tends to occur on the dorsum of the hands and feet.
- Cardiac involvement may present with arrhythmias or transient heart block. Conduction abnormalities are not uncommon but most cases are isolated and rarely last more than a few days. Rarely does a patient require permanent pacing[1]
Associated Co-Morbidities[edit | edit source]
Babesia[edit | edit source]
Babesia microti is a parasite that enters the bloodstream along with Borrelia at the time of the tick bite and attacks and destroys the host’s red blood cells. It can be potentially life-threatening, especially in individuals who are elderly, immuno-compromised, do not have a spleen, or have other diseases involving the kidney or liver. If not treated, complications can include hemodynamic instability, anemia, thrombocytopenia, organ failure, or death.[6]
Chronic Fatigue Syndrome[edit | edit source]
Individuals who present with symptoms of significant fatigue and malaise consistent with a diagnosis of Chronic Fatigue Syndrome often test positive for Borrelia antibodies, suggesting a prior infection even in individuals with no previous clinical diagnosis of Lyme disease. In a double-blind study performed in Germany in 1999, researchers found that individuals who tested positive for Borrelia antibodies and had a history of tick bites were significantly more likely to report symptoms of fatigue and malaise than individuals who had a history of tick bites but tested negative for Borrelia antibodies.[7]
Fibromyalgia Syndrome[edit | edit source]
Similar studies have found temporal links between Borrelia infection and the development of clinically diagnosable Fibromyalgia, the etiology of which is generally multifactorial and can be triggered by environmental factors, trauma, stress, infection, and possibly vaccination.[8]
Cardiac Dysfunction[edit | edit source]
Cardiac problems arising as a result of Lyme disease may occur in 4 to 10% of affected individuals. Potential problems include <a href="http://www.nlm.nih.gov/medlineplus/ency/article/000149.htm">myocarditis</a>, heart conduction block, and arrhythmia. Symptoms of cardiac involvement include bradycardia, tachycardia, irregular heartbeat, dizziness, syncope, and shortness of air.[9]
Neurological Disorders[edit | edit source]
Neurological and mental health co-morbidities develop in approximately 5% of Lyme disease patients, especially if the disease is not successfully treated initially.[9] Neurological sequelae include radiculopathy and paresthesias in the extremities. Associated mental health changes include mild cognitive impairments, mood disorders, depression, and anxiety. [10]
Autism[edit | edit source]
Although controversy exists over whether or not autism is truly a co-morbidity of Lyme disease, recent research shows a correlation between the two. Chronic infectious diseases including the Borrelia organism that causes Lyme have been associated with other co-infections that may weaken the fetal or infant immune system, putting affected individuals at increased risk for developing autism spectrum disorders.[11]
Prevention[edit | edit source]
- Avoid tick-infested areas, especially during summer months
- Walk on cleared or paved surfaces when available, rather than tall grass
- Wear long pants, sleeved shirts, and close-toed shoes
- Light-colored clothing makes it easier to locate a tick
- Always check for ticks whenever coming from outdoors. The risk of Lyme disease is minimized when the tick is removed within 36 hours.
- Showering immediately after being outdoors reduces the risk of tick attachment
- Wash clothing that's been outdoors (dryer kills ticks)
- Remove the tick only by using tweezers to pull the tick directly off the skin (no twisting)
- After removal of the tick, wash site with soap and water and then swab the area with antiseptic [4]
Medications[edit | edit source]
Acute cases of Lyme disease are initially treated with a 14 to 21-day course of oral antibiotics such as doxycycline, amoxicillin, or cefuroxime which are all safe and highly effective for the early stages of Lyme disease. A single 200-mg dose of doxycycline reduces the risk of Lyme disease in individuals bitten by ticks; however, these are not to be taken routinely (There's a low risk of transmission from a tick bite even in areas where the disease is most prevalent) and is contraindicated for pregnant women and children younger than 8 years of age.[12] If an affected individual presents with neurological impairments or a third-degree heart block, IV antibiotics such as ceftriaxone are administered for 14 to 28 days. Lyme-related joint and muscle pain (Lyme arthritis) is also generally treated with oral antibiotics. If Lyme arthritis persists after the first course of antibiotics, an additional four-week course of oral antibiotics is recommended. . There is no evidence that patients treated for Lyme disease with persistent, nonspecific symptoms (e.g., arthralgia and fatigue) have persistent infection; the risks of prolonged treatment is substantial, and far outweighs the benefits if any. [12] Arthritic symptoms that persist beyond both courses of antibiotic treatment are generally treated with antirheumatic and nonsteroidal anti-inflammatory (NSAID) medications.[9] Immunology is not developed with the exposure to Lyme disease, meaning that patients can be re-infected after the previous infection. It is important to note that Lyme disease is rarely fatal, but can have an impact on the cardiovascular system that could potentially cause life-threatening cardiac arrhythmias. [2]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Lyme disease is diagnosed based on symptoms, physical findings (such as a characteristic rash called erythema migrans), and the possibility of exposure to infected ticks. Laboratory testing is helpful in the later stages of disease.
Diagnosis of any infectious disease requires a combination of clinical experience and assessment by the doctor and understanding of the lab tests and their limitations. Laboratory tests are rarely definitive and all tests have a proportion of results which are false-positive (test indicates disease in someone without the disease) and false negative (test indicates that there is no disease in someone with the disease). When tests are done in places where the disease is rare or absent (for example, Lyme disease in Australia), many positive tests will be falsely positive.
The tests to diagnose Lyme disease are technically complex and require specialist expertise. It is important for people who want to be tested to make sure the laboratory that performs the test is reliable.
Lyme disease is most commonly diagnosed by a screening test called ELISA and this is then confirmed using a western blot test. Both of these tests detect antibodies that are produced by the immune system of someone with Lyme disease.
Lyme disease can also be diagnosed by testing a sample of the skin lesion by nucleic acid testing (eg PCR) or culture.[13]
Causes[edit | edit source]
Lyme disease is caused by spirochete microorganisms in the family Borrelia (in the United States, the specific species involved is Borrelia burgdorferi) which are transmitted primarily by black-legged or deer ticks. Deer ticks generally feed on the blood of deer, small birds, and mice, but are opportunistic and will also feed on the blood of other hosts such as cats, dogs, horses, and humans. Infected deer ticks transmit the bacteria to their host during the process of feeding.
Risks for being bitten by a tick capable of transmitting Borrelia bacteria include spending time outdoors in wooded or grassy areas especially in the Northeast and Midwest (see Prevalence section above). Walking in wooded or grassy areas in shorts and/or short sleeves increases the risk because of the higher surface area of exposed skin. The risk of acquiring an infection also increases if a tick is allowed to remain attached to the body for more than 48 hours, allowing it to take in a full “blood meal.” If a tick is identified and removed prior to that time, the risk of infection is low.[14]
Systemic Involvement[edit | edit source]
Lyme disease, especially if left untreated, may involve multiple systems as detailed in the Characteristics/Clinical Presentation section above. If the infection is allowed to progress from a localized one at the site of the tick bite to a systemic one, it may affect the central nervous, cardiac, and musculoskeletal systems.
Medical Management[edit | edit source]
- Specific treatment is dependent upon the age of the patient and stage of the disease.
- For patients older than 8 years of age with early, localized disease, doxycycline is recommended for 10 days. Patients under the age of 8 should receive amoxicillin or cefuroxime for 14 days to avoid the potential for tooth staining caused by tetracycline use in young children.
- Longer courses and parenteral antibiotics may be required for more severe manifestations such as arthritis, atrioventricular heart block, carditis, meningitis or encephalitis, although European data and newer studies demonstrate that oral treatment regimens or transitioning to oral therapy at hospital discharge may be appropriate for some patients.
- Doxycycline is used in most patients except in children and pregnant women. In children, amoxicillin remains the drug of choice. Pregnant women show a good response to ceftriaxone.
- Patients with Lyme carditis should be admitted and monitored until the ECG features of a block subside. Lyme arthritis usually resolves in 6-8 weeks. CNS Lyme disease responds well to antibiotics. Clinicians should monitor patients for the Jarisch-Herxheimer reaction when starting therapy.
- The ocular feature of Lyme disease does respond to topical steroids and IV ceftriaxone or penicillin.
- Some patients may experience post-treatment Lyme disease syndrome with nonspecific symptoms. These symptoms do not respond to antibiotics.
Physical Therapy Management[edit | edit source]
Early-stage Lyme disease can only be treated with antibiotics and other adjunct medications such as analgesics. Some doctors will refer patients with chronic Lyme disease symptoms that do not respond to medication to physical therapy. The role that physical therapy plays in the treatment of Lyme disease is primarily to:
- Relieve pain,
- Prepare de-conditioned patients to begin a home-based exercise program
- Educate patients regarding proper exercise technique and frequency, duration, and resistance appropriate to achieve wellness benefits without exacerbating Lyme-related symptoms.[15]
Physical therapy interventions include:
- Massage,
- Range of motion,
- Myofascial release
- Modalities including ultrasound, moist heat, and paraffin.
- Generally, ice packs and electrical stimulation are contraindicated, though there is no research to support this.
- Exercise prescription is aimed at improving strength and gradually increasing the patient's conditioning level which may be severely impaired as a result of chronic Lyme infection. Whole-body workouts generally feature extensive stretching, light callisthenics, and light resistance training with low loads and high repetitions.[15]
In addition, many patients with specific neurological complications such as Facial Palsy may also be referred for physical therapy. Electrical stimulation of paralyzed or weak facial muscles following Lyme-related neurological insult is considered a fairly common practice, though the research does not fully support its use. There are few randomized controlled trials investigating its effectiveness and those that do exist indicate that it may be neither harmful nor beneficial with many therapists taking a conservative approach and waiting several months between symptom onset and initiation of an e-stim program to allow natural neurological recovery to occur. [16] Neuromuscular Facial Reeducation has been demonstrated to be beneficial in facial palsy[17], as has EMG biofeedback[18].
Physical Therapists should be aware of the signs of Lyme Arthritis which typically manifests approximately four months after Erythema Migrans. It is most common in the knee but can be found in multiple joints.[19] Below is a short video about Lyme Disease and physical therapy management:
Differential Diagnosis[edit | edit source]
In patients with erythema migrans, a careful history and physical examination are all that is required to establish the diagnosis of Lyme disease. However, many patients with Lyme disease present with erythema migrans or extracutaneous symptoms making the diagnosis a challenge. In those cases, erythema migrans may never have occurred, may not have been recognized, or may not have been correctly diagnosed by the clinician[1].
Other problems include the following:
- Acute memory disorders
- Ankylosing spondylitis and rheumatoid arthritis
- Atrioventricular nodal block
- Cellulitis
- Contact dermatitis
- Gout and pseudogout
- Granuloma annulare
- Prion-related diseases
Conclusion[edit | edit source]
The prognosis for patients who are treated for Lyme disease is excellent with no residual deficits.
- A few individuals may develop a recurrent infection if an infected tick bites them.
- Individuals who receive late treatment may develop neurological and musculoskeletal symptoms.
- Lyme arthritis is not uncommon.
- Some patients may develop Lyme carditis that results in a heart block and requires temporary pacing of the heart.
- Despite the large numbers of people affected, Lyme disease is not fatal. There continues to be a debate about the existence of post-treatment Lyme disease, but so far, this diagnosis has been promoted by the lay public and media as there is no good evidence that such a condition exists
Resources[edit | edit source]
- CDC Division of Vector-Borne Infectious Diseases
- Lyme Disease Foundation
- Canadian Lyme Disease Foundation
- Lyme Disease Map Project
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Skar GL, Simonsen KA. Lyme Disease. InStatPearls [Internet] 2018 Oct 27. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431066/ (last accessed 26.12.2019)
- ↑ 2.0 2.1 2.2 Lyme Disease. Centers for Disease Control and Prevention. http://www.cdc.gov/lyme. Published August 19, 2016. Accessed March 23, 2017.
- ↑ The Department of Health, Australia. Lyme Disease. Available from: https://www1.health.gov.au/internet/main/publishing.nsf/Content/ohp-lyme-disease.htm (last accessed 26.12.2019)
- ↑ 4.0 4.1 Goodman CC, Fuller K. Pathology: Implications for the Physical Therapist. 4th ed. St. Louis: Saunders Elsevier; 2014.
- ↑ CDC Division of Vector-borne Infectious Diseases website. Lyme Disease. Available at http://www.cdc.gov/ncidod/dvbid/Lyme. Accessed February 18, 2010.
- ↑ Babesia. CDC website. Available at http://www.cdc.gov/babesiosis. Accessed February 24, 2010.
- ↑ Treib J, Grauer M, Haass A, Langenbach J, Holzer G, Woessner R. Chronic fatigue syndrome in patients with lyme borreliosis. Eur Neurol [serial online]. 2000 Feb;43(2):107-109.
- ↑ Buskila D, Atzeni F, Sarzi-Puttini P. Etiology of fibromyalgia: The possible role of infection and vaccination. Autoimmunity Reviews [serial online]. 2008 Oct;8(1):41-43.
- ↑ 9.0 9.1 9.2 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis: Saunders Elsevier; 2009.
- ↑ Rudnik I, Konarzewska B, Zajkowska J, Juchnowicz D, Markowski T, Pancewicz S. [The organic disorders in the course of Lyme disease]. Polski Merkuriusz Lekarski: Organ Polskiego Towarzystwa Lekarskiego [serial online]. 2004 Apr;16(94):328-331.
- ↑ Bransfield R, Wulfman J, Harvey W, Usman A. The association between tick-borne infections, Lyme borreliosis and autism spectrum disorders. Medical Hypotheses [serial online]. 2008;70(5):967-974.
- ↑ 12.0 12.1 Lyme Disease. New England Journal of Medicine. 2014;371(7):683-684. doi:10.1056/nejmc1407264.
- ↑ NSW government Lyme disease factsheet Available from: https://www.health.nsw.gov.au/Infectious/factsheets/Pages/Lyme_disease.aspx (last accessed 26.12.2019)
- ↑ Mayo Clinic website. Lyme Disease. Available at http://www.mayoclinic.com/health/lyme-disease/DS00116. Accessed February 25, 2010.
- ↑ 15.0 15.1 Burrascano JJ. Advanced Topics in Lyme Disease: diagnostic hints and treatment guidelines for lyme and other tick borne illnesses. 15th ed. 2005. Available at http://www.lymediseaseassociation.org/drbguide200509.pdf
- ↑ Ohtake PJ, Zafron ML, Poranki LG, Fish DR. Evidence in Practice. Physical Therapy. 2006;86:1558-1564.
- ↑ Manikandan N. Effect of facial neuromuscular re-education on facial symmetry in patients with Bell's palsy: a randomized controlled trial. Clin Rehabil. 2007 Apr;21(4):338-43
- ↑ Bossi D, Buonocore M et al. Usefulness of BFB/EMG in facial palsy rehabilitation. Disabil Rehabil. 2005 Jul 22;27(14):809-15
- ↑ Arvikar S, Crowley J, Sulka k, et al. Autoimmune Arthritides, Rheumatoid Arthritis, Psoriatic Arthritis, or Peripheral Spondyloarthritis Following Lyme Disease: Arthritis; Rheumatology. Published online December 28, 2016. DOI: 10.1002/art.39866.
- ↑ Lyme Disease and Physical Therapy. Available from: https://youtu.be/QUIu1bvnC-8 [last accessed 28/12/19]