Immunoglobulins (Ig)
Original Editor - Lucinda hampton
Top Contributors - Kirsten Coutts, Lucinda hampton, Kim Jackson and Nupur Smit Shah
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (20/04/2023)
Introduction[edit | edit source]
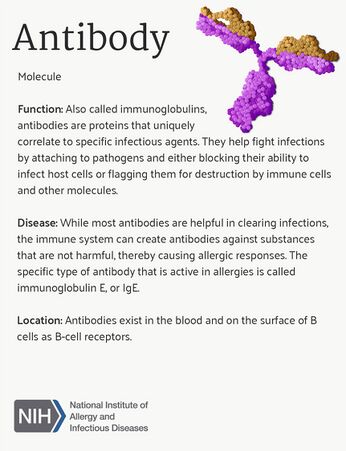
Immunoglobulins (Ig) or Antibodies are glycoproteins that your immune cells make to fight off bacteria, viruses, fungi, parasites, cellular antigens, chemicals, and synthetic substances[1]. Plasma cells (AKA plasma B cells) produce immunoglobulins. B cells are produced in stem cells in bone marrow and play an important role in the humoral immune response.[2]
- Immunoglobulins constitute about 20% of the protein in plasma[1]
- The antibody immune response is highly complex and exceedingly specific.
- The main functions are:
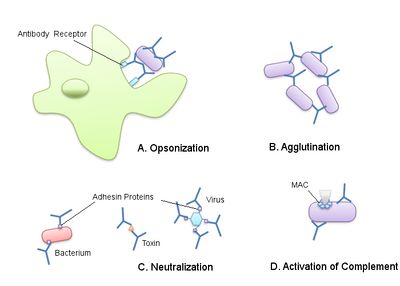
- Through their B cell receptor they recognise an antigen on the surface of a pathogen. Through direct binding they are able to neutralise the foreign material and prevent it from having an adverse effect on the body.[2]
- Through opsonisation they alter the antigen to make it more readily engulfed by phagocytes. [2]
- B cells secrete anti-inflammatory and pro-inflammatory cytokines. These influence the T cell response and assist in the development and suppression of auto-immunity.[2]
- Additionally they secrete a cascade of enzymes which play a significant role in the early antiviral immune response and in the regulation of autoimmunity.[2]
- Antibodies thus have a crucial role in mediating humoral immunity but also in their specific antibody functions.[2]
· See Image 1 and 3.
- Antibody tests are used to detect disease-specific antibodies in a blood sample.[3]
- WHO officially coined the term Immunoglobulins for antibodies in 1964. [4]
- A low level of any or all of the immunoglobulins is called hypogammaglobulinemia. This can be from a primary or a secondary origin. Primary being from genetic disorders or chromosome anomalies. Secondary being from other external causes such as infectious agents, mediators such as corticosteroids and immunosuppressants, chemotherapy, metabolic diseases such as nephrotic syndrome, nutritional disorders, and environmental conditions such as ionizing radiation.[5]
5 types of immunoglobulins in humans[edit | edit source]
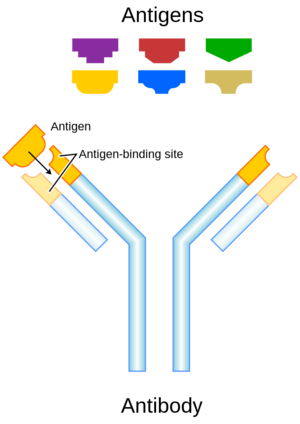
Though the general structure of all antibodies is very similar, the small region at the tip of the protein is extremely variable as can be seen in image 2. This allows millions of antibodies with different tip structures to exist. Each of these variants can bind to a different antigen. This enormous diversity of antibodies allows the immune system to recognise a wide variety of antigens[1].
There are five main types of immunoglobulins, each immunoglobulin can have a different binding site that matches a specific antigen.[1]
Immunoglobulin G (IgG)
- Accounts for around 75% of all antibodies in the human body.
- Depending on the antigen, IgG can either tag a pathogen so other immune cells and proteins will recognise it, or it can promote the release of toxins to directly destroy the microorganism.
- IgG can sometimes trigger an undesirable response in people with autoimmune disorders.[1]
Immunoglobulin A (IgA)
- Accounts for 15% of all antibodies in the human body
- Primarily found in mucosal tissues (eg mouth, vagina, and intestines) as well as in saliva, tears, and breast milk.
- Produced by B cells and secreted from the lamina propria (a thin layer within mucosal tissues).
- One of the body's first-line defences against infection - it binds to pathogens tagging them for destruction and preventing them from sticking to the epithelium (which lines the body's tissues).
- Associated with hypersensitive reactions in people with celiac disease and several other autoimmune disorders.[1]
Immunoglobulin M (IgM)
- Immunoglobulin M (IgM) is also one of the first antibodies recruited by the immune system to fight infection.
- IgM populations rise very quickly when the body is first confronted with an infectious organism, and then they plummet as IgG antibodies take over.
- IgM is also produced by B cells and, when bound to a pathogen, will spur other antibodies and immune cells into action.
- A subset of IgM helps B cells "remember" a pathogen after it has been destroyed. If you were to become re-exposed to the pathogen later, your immune system should respond more quickly due to your memory B cells.[1]
Immunoglobulin E (IgE)
- The antibody responsible for the allergic response that is mostly found in the lungs, skin, and mucosal membranes.
- Produced by B cells secreted by lymph nodes or other lymphoid tissues situated near the site of the allergen.
- When IgE binds to an allergen, it triggers a cascade of events. Basophils and mast cells (subtypes of WBCs,) degranulate and release histamine, an inflammatory compound, into the bloodstream.
- IgE also helps to protect the body from parasitic infections, including helminths (parasitic worms).[1]
Immunoglobulin D (IgD)
- Accounts for only around 0.25% of antibodies in the human body.
- Important in the early stages of the immune response.
- Unlike other antibodies, it does not actively circulate but binds to B cells to instigate the immune response.
- IgD helps incite the release of front-line IgM to fight disease and infection.
- The least understood antibody, with little known about how it might participate in other parts of the immune system[6].
Antibody Testing[edit | edit source]
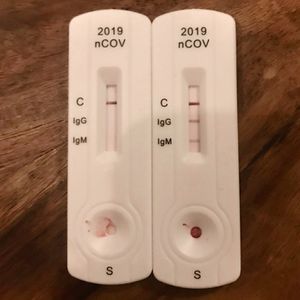
As immunoglobulins are matched to a specific pathogen, they are used to diagnose some diseases (as they detect disease-specific antibodies in a blood sample).
Antibody tests
- Do not detect the actual pathogens that cause an infection—they detect the antibodies that are produced in response to the infection. A positive result means "yes," the test has detected the antibody or antigen. A negative result means "no," while borderline results are considered inconclusive.
- Depending on the disease, it may take time for enough antibodies to be produced to reach detectable levels. If it's done too soon, during the early window period, the test may deliver a false negative result.
Antibody tests are available to help diagnose a wide variety of infectious and autoimmune diseases, including:
- Celiac disease (CD)
- COVID-19 Image 4: The rapid diagnostic test shows reactions of IgG and IgM antibodies.
- Cytomegalovirus (CMV)
- Epstein-Barr virus (EBV)
- HIV
- Lyme disease
- SLE (Lupus)
- Polio
- Tuberculosis[6]
Clinical use of immunoglobulins[edit | edit source]
Immunoglobulin therapy is used worldwide and can be used in the areas of Neurology, Haematology, Immunology and other fields of medicine.
- Polyvalent immunoglobulin, derived from pooled human plasma, can be administered via the intravenous, subcutaneous or intramuscular route. [7]
- It is prepared from a pool of blood donated at blood collection centres and processed through fractionation to separate the protein fraction from the cellular component.
- Immunoglobulin therapy is the mainstay of treatment for antibody-deficient disorders, as well as being an important supportive treatment for other forms of Primary Immune deficiencies. [8]
- Antibiotics and anti-fungal treatments are also used to help prevent the frequency and severity of infections
- Modern advances in fractition and filtration techniques since the late 1940s have led to safer and pure immunoglobulin preparations. [7]
- Treatment is expensive and can be a barrier to timely and regular therapy in many countries. Furthermore, the choice of product options is limited in many countries, such as South Africa where only 4 different products are available. [7] Image 5 shows one example of these products. Polygam® is one of the products available in South Africa.
- The purified immunoglobulin can be used in the treatment of many immunological disorders, including antibody deficiencies, severe combined immunodeficiency disorders (SCID), multiple sclerosis, myasthenia gravis, Kawasaki disease, systemic lupus erythematosus (SLE), organ transplants, and many others[1].
- There is high-quality evidence that supports its use in primary antibody failure, Guillain-Barre syndrome, chronic inflammatory demyelinating polyneuropathy, acute idiopathic thrombocytopenia, Kawasaki disease and immunobullous disease. Low quality evidence shows benefit in other uncommon autoimmune and immunodeficient conditions.[7]
Side effects of Intravenous Immunoglobulin therapy[edit | edit source]
- Immediate infusion-related reactions occur in about 1% of all immunoglobulin infusions, but are mostly mild and treated with simple analgesia. Some examples of these are fever, headache, myalgia, malaise, infusion site pain and tachycardia. [7]
- Moderate reactions can be treated with antihistamines and corticosteroids. Some examples of these are eczema and haemolytic anaemia. [7]
- Severe reactions include anaphylactic reactions and thrombosis. This is associated with high-dose immunoglobulin therapy. [7]
Deficiency Disorders[edit | edit source]
Primary Immunodeficiencies (PID) are genetic disorders that impair the normal functioning of the immune system. PID can occur in both children and adults, who are subject to serious, prolonged and sometimes life threatening infections and autoimmunity when not properly identified and treated. [8][9]
IgA deficiency is the most common PID, occurring in approximately 1 in 300 to 1 in 500 persons. It is characterised by recurrent infections that affect the respiratory, digestive, and genitourinary systems. Recurrent pneumonia, Giardia lamblia infestation, and urinary sepsis are prevalent. The majority of patients can be asymptomatic. They are at higher risks for autoimmune diseases, atopy, and anaphylaxis to IgA-containing products.[1]
The major categories of PIDs are classified according to the component of the immune system that is primarily disrupted: adaptive or innate immunity. These are the major categories of PIDs[8]:
Disorders of adaptive immunity
- T-cell (cellular) Immunodeficiency
- B-cell (antibody-mediated) deficiency
- Combined immunodeficiency (CID)
Disorders of innate immunity
- Phagocyte defects eg chronic granulomatous disease
- Complement defects
Disorders of immune dysregulation
- Hemophagoctic lymphohistiocytosis (HLH)
- Autoimmine lymphoproliferative syndrome (ALPS)
- Immunodysregulation polyendocrinopathy (IPEX)
- Autoimmune polyendocrinopathy candidiasis and ectodermal dystrophy (APECED)
Treatment of PIDs is complex and involves both supportive and definitive strategies. It is critically important that therapy is coordinated by an immunologist with experience in these disorders[8]. In many patients, the immunoglobulin replacement therapy will be lifelong.
Diagnosis of Primary Immunodeficiency[edit | edit source]
Early detection of PID is critical for preventing significant disease-associated morbidity, and even mortality. National surveys in the United States of America found that approximately 60% of patients with these disorders were not diagnosed until adulthood. The importance of prompt recognition and management of PID’s is further highlighted by the rate of hospitalisations pre-and post diagnosis. Although 70% reported being hospitalised prior to diagnosis, nearly half (48%) reported no hospitalisations since diagnosis[8].
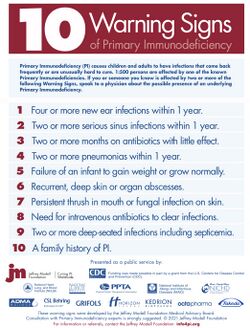
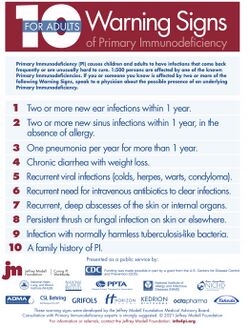
The Jefffrey Modell Foundation is an international, non-profit, organisation dedicated to helping individuals and family members affected by primary immunodeficiency disorders. The organisation formed a list of 10 Warning signs of Primary Immunodeficiency for both adults and children[9]. See Images 7 and 8. They also produced a summary on the 4 stages of testing which can be seen in image 9.
There are also secondary Immunodeficiencies which may result from other causes, such as viral or bacterial infections, malnutrition, Immunoglobulin loss, malignancy or treatment with drugs that induce immunosuppression[8].
Prognosis[edit | edit source]
The prognosis of PID varies depending on the etiology of the disorder. Advancements in medicine and the improved management of infections, as well as better access to antibiotics, bone marrow transplants and stem cell transplants has improved patient outcomes and mortality rates. The initiation of newborn screening programs, routine vaccinations and advancements in genomic technologies over the past few decades have allowed for better detection and understanding of PIDs.[8][9]
New research on the genes responsible for immunodeficiencies is ongoing and will continue to guide and advance treatment strategies.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Vaillant AA, Ramphul K. Immunoglobulin. InStatPearls [Internet] 2019 Nov 10. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK513460/ (last accessed 3.12.2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Upasani V, Rodenhuis-Zybert I, Cantaert T. Antibody-independent functions of B cells during viral infections. Plos Pathogens 2021;17:7
- ↑ Thermofischer scientific Immunoglobulins Available from:https://www.thermofisher.com/au/en/home/life-science/antibodies/antibodies-learning-center/antibodies-resource-library/antibody-methods/introduction-immunoglobulins.html (last accessed 3.12.2020)
- ↑ Easybiology antibodies Available from: https://www.easybiologyclass.com/difference-between-antibody-and-immunoglobulin/ (last accessed 3.12.2020)
- ↑ Pimenta FM, Palma SM, Constantino-Silva RN, Grumach AS. Hypogammaglobulinemia: a diagnosis that must not be overlooked. Brazilian Journal of Medical and Biological Research 2019;52:10
- ↑ 6.0 6.1 Very well health Antibodies Available from:https://www.verywellhealth.com/antibody-isotypes-3132614 (last accessed 3.12.2020)
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Peter JG, Heckmann JM. Recommendations for the use of immunoglobulin therapy for immunomodulation and antibody replacement. South African Medical Journal 2014;104:7306
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 McCusker C, Upton J, Warrington R. Primary Immunodeficiency. Allergy, Asthma & Clinical Immunology 2018;14:141-152
- ↑ 9.0 9.1 9.2 Quinn J, Modell V, Orange JS, Modell J. Growth in diagnosis and treatment of primary immunodeficiency within the global Jeffrey Modell Centers Network. 2022;18:19