Thrombosis
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton
Introduction[edit | edit source]
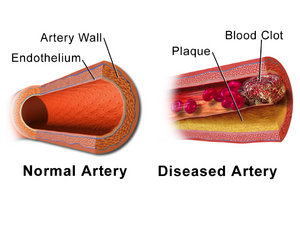
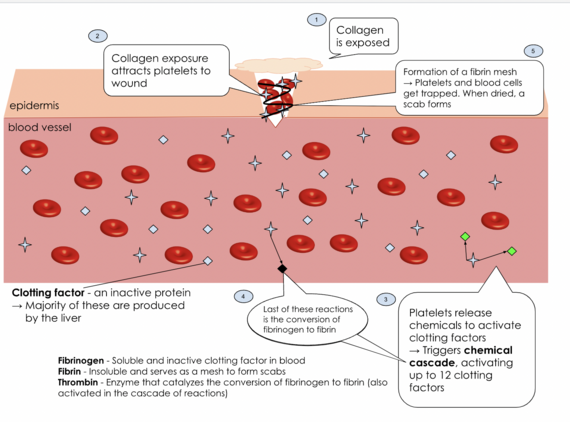
Thrombosis is when a blood clot (thrombus) forms within a blood vessel and prevents the correct flow of blood around the circulatory system. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cross-linked fibrin protein. A thrombus is a healthy response to injury aiming to stop and prevent further bleeding, however it can be harmful when a clot obstructs blood flow in the circulatory system.
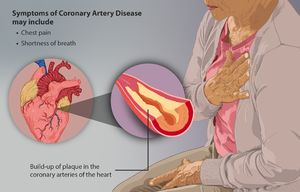
Acute venous and arterial thrombosis account for the most common causes of death in developed countries, the highest proportion of these deaths being from myocardial infarction and stroke. Nevertheless, thrombosis can be prevented and treated in time if it is identified[1][2].
Etiology[edit | edit source]
Thrombosis occurs when an imbalance occurs in the complex homeostasis that exists between blood cells (including platelets), plasma proteins, coagulation factors, inflammatory factors and cytokines, and the endothelial lining of the arteries and veins.
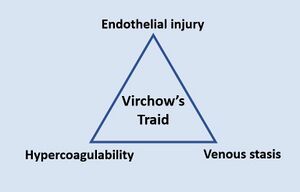
Virchow's Triad defines the types of conditions increase the risk to the a patient of an abnormal thrombus formation:
- Endothelial damage: increases the risk of thrombus formation through a myriad of mechanisms. eg when endothelium gets prised apart the tissue factor is exposed (which initiates the coagulation cascade). Conditions include atherosclerosis and bacterial sepsis.
- Abnormal blood flow: eg patients with prolonged immobilization, those with varicose veins or atrial fibrillation. In these situations blood is allowed to stagnate, increasing the chance that platelets and coagulation factors will meet up and start clot formation.
- Hypercoagulability: various disorders eg oral contraceptive use, obesity, pregnancy, smoking, and hereditary thrombotic disorders (eg factor V Leiden). The mechanisms underlying this category of risk are numerous and often not fully understood[3].
Hemostasis: Control of Bleeding, Coagulation and Thrombosis[edit | edit source]
Watch this 5 minute video to understand the homeostatic mechanism that control of bleeding, coagulation and Thrombosis formation. It also has information on bleeding disorders (eg Von Willebrand Disease, Haemophilia), unwanted blood clotting (eg as in stroke, MI) and preventative strategies for those at risk of thrombosis.
Types of Thrombi[edit | edit source]
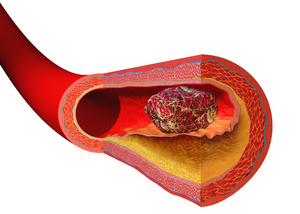
The composition and appearance of a thrombus differ according to their location:
- Arterial thrombus: typically composed of platelet aggregates (white thrombus). Clot formation is typically triggered by the rupture of an atherosclerotic plaque, with platelets quickly recruited to the site. The fibrin content of the clot gradually increases as the thrombus extends into the arterial lumen. Fibrin is an elastic, insoluble, whitish protein produced by the action of thrombin on fibrinogen and forms an interlacing fibrous network in the coagulation of blood[5]. An arterial thrombus is platelet-rich, fast growing, and unprotected from fast blood flow. Arterial thrombi can result in eg MI and unstable angina,ischaemic stroke, and acute limb ischaemia (in PAD)[6].
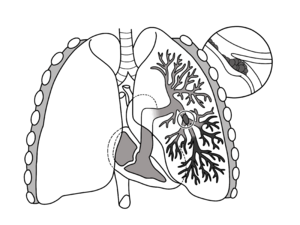
- Venous thrombus: largely consists of fibrin and red blood cells (red thrombus)[7]. Venous thrombi feature enmeshed erythrocytes that are prone to fragmentation, creating an embolus. Two common examples are DVT and PE.[8]
Thrombosis occurs throughout our arterial system, typically in people with predisposing cardiovascular risk factors.
In the heart, microthrombi may develop as a consequence of blood stasis in the ventricles or atria due to underlying valvular heart disease, cardiomyopathies, or arrhythmias, predisposing to ischemic emboli and CVA.
Arterial thrombosis (and microthrombi formation) often begin when the lipid plaques accumulate in the arterial wall, provoking chronic inflammatory cells and platelet activation. Platelets play alarge role in the development of arterial thrombosis compared to venous thrombosis, explaining why antiplatelet agents form a cornerstone of the prevention and treatment of arterial thrombosis.
The initial lipid plaques evolve into fibrous plaques which can rupture with the eroding surface leading to the release of additional pro-coagulating factors. This is the process of atherosclerosis formation. Atherosclerosis allows the activation of platelets, causing adhesion and aggregation, which leads to the formation of a clot. The blocked vessel caused by the atherosclerosis and thrombin formation prevent proper blood flow, affecting function as in eg stroke.[2]
Clinical Presentation[edit | edit source]
Thromboses present in a myriad of ways depending on the location. If symptoms present themselves, then they can depend on where the clot lies within the body. eg A blood clot in the leg can cause pain, swelling or tenderness in one leg, usually in the calf area; a pulmonary embolism may cause shortness of breath, rapid breathing, coughing, coughing up blood and chest pains; an MI may present with chest pain and dysponea.
Treatment[edit | edit source]
To treat an existing thrombosis, doctors normally proscribe an anticoagulant to attempt to safely dissolve the clot. Heparin and Warfarin are the most common drugs that are administered in the UK. Patients who are on anticoagulant drugs need to be monitored regularly to make sure that their blood does not completely lose its clotting ability[1].
The treament varies depending on type of thromosis. Venous thromboembolism management utilises various anticoagulant agents that target procoagulant factors, while arterial thrombosis management is predominantly with antiplatelet agents as monotherapy or dual-antiplatelet therapy.[2]
Physiotherapy Relevance[edit | edit source]
Physiotherapists (along with other health professionals) have a role in helping patients reduce their risk of thrombosis by providing valid information on prevention and treatment. Clients should be educated and encouraged patients to make healthy lifestyle choices. eg, chronic smokers should be encouraged to quit smoking, morbidly obese clients should be encouraged to change their diet and lifestyle accordingly, those with uncontrolled blood pressure should receive education on the importance of lifestyle modification and referred onwards.
Patients admitted to the hospital are also at higher risk of thrombosis, and physiotherapists have a role here in appropriate treatment. See appropriate sections in links eg DVT, Stroke, MI, PE.
References[edit | edit source]
- ↑ 1.0 1.1 Thrombosis charity What is a thrombosis Available: http://www.thrombosis-charity.org.uk/what-is-thrombosis/(accessed 15.7.2022)
- ↑ 2.0 2.1 2.2 Ashorobi D, Ameer MA, Fernandez R. Thrombosis. StatPearls [Internet]. 2022 May 15. Available:https://www.ncbi.nlm.nih.gov/books/NBK538430/ (accessed 15.7.2022)
- ↑ Pathology student Virchows triad Available:https://www.pathologystudent.com/virchows-triad/ (accessed 16.7.2022)
- ↑ Alila Media Hemostasis: Control of Bleeding, Coagulation and Thrombosis, Animation Available:https://www.youtube.com/watch?app=desktop&v=x8TLTTyyPfI (accessed 18.7.2022)
- ↑ Medical dictionary Fibrin Available:https://medical-dictionary.thefreedictionary.com/fibrin (accessed 17.7.2022)
- ↑ Vascular Advisor Arterial Thrombi Available:https://www.thrombosisadviser.com/en/professionals/knowledge-base/essentials/arterial-thrombosis (accessed 16.7.2022)
- ↑ Thrombosis advisor Thrombus formation Available:https://www.thrombosisadviser.com/en/professionals/knowledge-base/essentials/thrombus-formation (accessed 16.7.2022)
- ↑ Vascular Advisor Venous Thrombi Available:https://www.thrombosisadviser.com/en/professionals/knowledge-base/essentials/venous-thrombosis (accessed 16.7.2022)