Stroke
Original Editor - Wendy Walker Top Contributors - Admin, Wendy Walker, Kim Jackson, Rachael Lowe, Laura Ritchie, Vidya Acharya, Naomi O'Reilly, Lucinda hampton, Tony Lowe, Katherine McBeth, Scott Buxton, Sweta Christian, Evan Thomas, Magdalena Hytros, Priyanka Chugh, Simisola Ajeyalemi, 127.0.0.1, Rucha Gadgil, Amrita Patro and Karen Wilson
Introduction[edit | edit source]
According to the World Health Organisation, a Stroke is defined as an accident to the brain with "rapidly developing clinical signs of focal or global disturbance to cerebral function, with symptoms lasting 24 hours or longer, or leading to death, with no apparent cause other than of vascular origin and includes cerebral infarction, intracerebral hemorrhage, and subarachnoid hemorrhage".
Acute stroke is also commonly called a cerebrovascular accident which is not a term preferred by most stroke neurologists. Stroke is NOT an accident. The better and more meaningful term is "brain attack", similar in significance to "heart attack".[1]
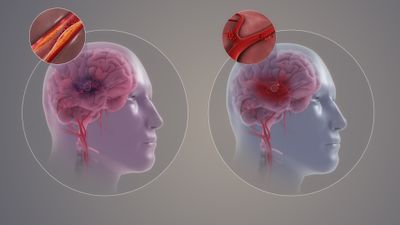
There are two main types of strokes[1].
- The commoner type is an ischemic stroke, caused by interruption of blood flow to a certain area of the brain. Ischemic stroke accounts for 85% of all acute strokes. According to the TOAST classification, there are four main types of ischemic strokes. These are large vessel atherosclerosis, small vessel diseases (lacunar infarcts), cardioembolic strokes and cryptogenic strokes (see left hand picture on image).
- 15% of acute strokes are hemorrhagic strokes which are caused by bursting of a blood vessel i.e. acute hemorrhage. There are two main types of hemorrhagic strokes, intracerebral hemorrhage (ICH) and subarachnoid hemorrhage which accounts for about 5% of all strokes (see R hand picture on image)
Regardless of the type of stroke, it is important to know that with each minute of large vessel ischemic stroke untreated, close to two million neurons die. This is the most important "time is brain" concept in understanding acute stroke and its treatment.
Epidemiology/ Etiology[edit | edit source]
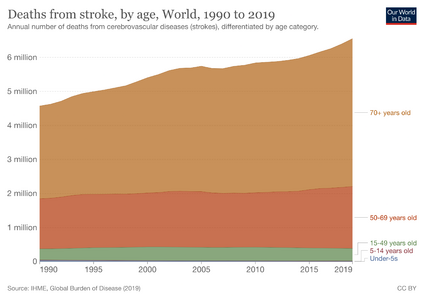
According to the World Health Organization (WHO), 15 million people suffer stroke worldwide each year. Of these, 5 million die and another 5 million are left permanently disabled.[2] The 2010 Global Burden of Disease Study suggested Stroke is the second leading cause of death globally and the third leading cause of premature death and disability as measured in Disability Adjusted Life Years (DALY). Cerebrovascular disease is the largest neurologic contributor and accounts for 4.1% of total global DALY.
In the United States, there are 800,000 new strokes every year. There is one new stroke every 40 seconds. Stroke is the 5th leading cause of death and the first leading cause of disability. [1]
Stroke kills more than 49,000 people each year in the UK, nearly 1 in 10. In 2010 stroke was the fourth-largest cause of death in the UK after cancer, heart disease, and respiratory disease.[3]
Many etiologies can lead to a stroke. Some of the most common risk factors include [1]
- Hypertension, diabetes mellitus, hypercholesterolemia, physical inactivity, obesity, genetics, and smoking.
- Cerebral emboli commonly originate from the heart, especially in patients with preexisting heart arrhythmias (atrial fibrillation), valvular disease, structural defects (atrial and ventricular septal defects) and chronic rheumatic heart disease.
- Emboli may lodge in areas of preexisting stenosis.
- Alcohol intake has a J-shaped relationship with ischemic stroke. Mild to moderate drinking carries a slightly lower risk of ischemic stroke yet heavier drinking increases the risk drastically. Alcohol intake increases the risk of hemorrhagic stroke in a near-linear relationship.
Read more about Epidemiology, Incidence and Global Burden of Stroke
Clinically Relevant Anatomy[edit | edit source]
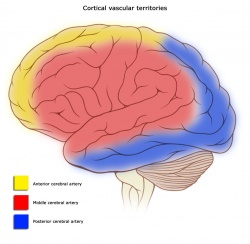
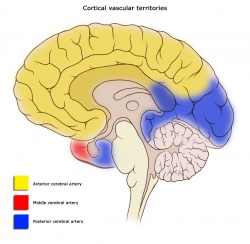
At the base of the brain, the carotid and vertebrobasilar arteries form a circle of communicating arteries known as the Circle of Willis (see image below). From this circle, other arteries—the anterior cerebral artery (ACA), the middle cerebral artery (MCA) and posterior cerebral artery (PCA)—arise and travel to all parts of the brain.
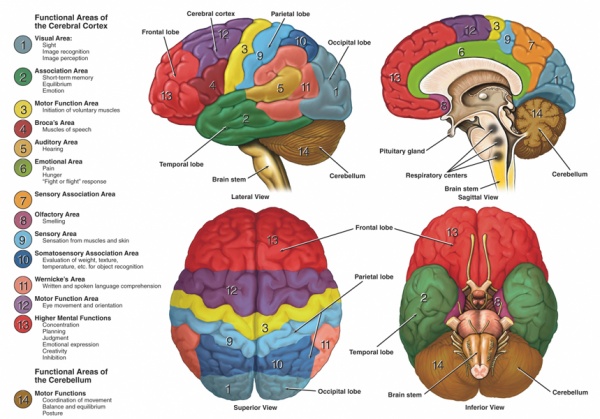
The image below clearly shows the function areas of the cerebral cortex that can be affected following insufficiency of the blood supply.
Mechanism of Injury / Pathological Process[edit | edit source]
| [4] |
A stroke occurs when there is an interruption of the blood supply to a particular area of the brain, ultimately leading to cell injury and cell death.
Strokes can be classified in two ways:
Ischaemic[edit | edit source]
Ischaemic strokes are the most common, accounting for up to 80% of strokes, and occur when there is an occlusion of a blood vessel impairing the flow of blood to the brain.
Ischaemic Strokes are divided into:
- Thrombotic - Where a blood clot forms in a main brain artery or within the small blood vessels deep inside the brain. The clot usually forms around atherosclerotic plaques.
- Embolic - A blood clot, air bubble or fat globule forms within a blood vessel elsewhere in the body and is carried to the brain.
- Systemic Hypoperfusion - A general decrease in blood supply, eg. 1. in shock 2.occurring in small vessels(lacunar infarcts) caused by chronic, uncontrolled hypertension resulting in the pathological entity of lipohyalinosis and arteriolosclerosis. These strokes occur in the basal ganglia, internal capsule, thalamus, and pons[1]. 3 Watershed strokes see link.
- Venous Thrombosis
According to the TOAST[5] classification, there are four main types of ischemic strokes.
- Large vessel atherosclerosis,
- Small vessel diseases (lacunar infarcts),
- Cardioembolic strokes
- Cryptogenic strokes
Haemorrhagic[edit | edit source]
- Haemorrhagic Strokes occur when a blood vessel in the brain ruptures and bleeds.
- Intracerebral Haemorrhagic Stroke — there is bleeding from a blood vessel within the brain. High blood pressure is the main cause of intracerebral haemorrhagic stroke.
- Subarachnoid Haemorrhagic Stroke — there is bleeding from a blood vessel between the surface of the brain and the arachnoid tissues that cover the brain.
Nb. Some experts do not classify Subarachnoid Haemorrhage as Stroke because subarachnoid haemorrhages present differently from Ischaemic Strokes and Intracerebral Haemorrhagic Strokes.
Clinical Presentation[edit | edit source]
Strokes can present in pre-determined syndromes due to the effect of decreased blood flow to particular areas of the brain that correlate to exam findings. This allows clinicians to be able to predict the area of the brain vasculature that can be affected.
Cortical Areas and their vascular supply:
Location of Infarct & Deficits Produced[edit | edit source]
Left MCA Superficial Division[edit | edit source]
Right face and arm upper-motor weakness due to damage to motor cortex, nonfluent (Broca’s) aphasia due to damage to Broca’s area. There may also be right face and arm cortical type sensory loss if the infarct involves the sensory cortex. Other deficits include a fluent (Wernicke’s) aphasia due to damage to Wernicke’s area. [Aphasia: a disturbance of the comprehension and expression of language]
Right MCA Superficial Division[edit | edit source]
Left face and arm upper-motor weakness due to damage to motor cortex. Left hemineglect (variable) due to damage to non-dominant association areas. There may also be left face and arm cortical type sensory loss if the infarct involves the sensory cortex.
Left MCA Lenticulostriate Branches[edit | edit source]
Right pure upper-motor hemiparesis due to damage to the basal ganglia (globus pallidus and striatum) and the genu of the internal capsule on the left side. Larger infarcts extending to the cortex may produce cortical deficits such as aphasia.
Right MCA Lenticulostriate Branches[edit | edit source]
Left pure upper-motor hemiparesis due to damage to the basal ganglia (globus pallidus and striatum) and the genu of the internal capsule on the right side. Larger infarcts extending to the cortex may produce cortical deficits such as aphasia.
Left PCA[edit | edit source]
Right homonymous hemianopia due to damage to left visual cortex in the occipital lobe. Extension to the corpus collusom interferes with communication between the two visual association areas so it can cause alexia without agraphia. Larger infarcts involving the internal capsule and thalamus may cause right hemi-sensory loss and right hemiparesis due to the disruption of the ascending and descending information passing through these structures. [Hemoanopia: visual loss in half of the visual field]
Right PCA[edit | edit source]
Left homonymous hemianopia due to damage to the right visual cortex in the occipital lobe. Larger infarcts involving the internal capsule and thalamus may cause left hemi-sensory loss and left hemiparesis due to the disruption of the ascending and descending information passing through these structures.
Left ACA[edit | edit source]
Right leg upper-motor neuron weakness due to damage to the motor cortex and right leg cortical sensory loss due to damage to the sensory cortex. Grasp reflex, frontal lobe behavioral abnormalities, and transcortical aphasia can also be seen if the prefrontal cortex and supplemental motor areas are involved.
Right ACA[edit | edit source]
Left leg upper-motor neuron weakness due to damage to the motor cortex and left leg cortical type sensory loss due to damage to the sensory cortex. Grasp reflex, frontal lobe behavioural abnormalities and left hemineglect can also be seen if the prefrontal cortex and non-dominant association cortex are involved.
| [6] | [7] | [8] |
Outcome Measures[edit | edit source]
Dynamic Gait Index, the 4-item Dynamic Gait Index, and the Functional Gait Assessment show sufficient validity, responsiveness, and reliability for the assessment of walking function in patients with stroke undergoing rehabilitation, but the Functional Gait Assessment is recommended for its psychometric properties[9].
Chedoke-McMaster Stroke Assessment
Chedoke Arm and Hand Activity Inventory
CRS-R Coma Recovery Scale Revised is used to assess patients with a disorder of consciousness, commonly coma.
Take a look at our Stroke Outcome Measures Overview for more information
Differential Diagnosis[edit | edit source]
The differential diagnosis is broad and can include stroke mimics such as TIA, metabolic derangement (in other words, hypoglycemia, hyponatremia), a hemiplegic migraine, infection, brain tumor, syncope, and conversion disorder.[1]
Management / Interventions[edit | edit source]
Early Management of Acute Stroke[edit | edit source]
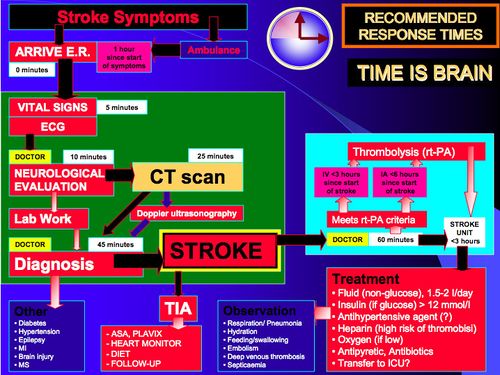
The goal for the acute management of patients with stroke is to stabilize the patient and to complete initial evaluation and assessment, including imaging and laboratory studies, within a short time frame. Critical decisions focus on the need for intubation, blood pressure control, and determination of risk/benefit for thrombolytic intervention.[10]
Patients presenting with Glasgow Coma Scale scores of 8 or less or rapidly decreasing Glasgow Coma Scale scores, require emergent airway control via intubation.
A recent study has shown gait improvement with high-intensity interval training and moderate-intensity continuous training in ambulatory chronic stroke patients. According to post-stroke guidelines, moderate-intensity, continuous aerobic training (MCT) improves aerobic capacity and mobility after stroke. High-intensity interval training (HIT) has been shown to be more effective than MCT among healthy adults and people with heart disease.
Physiotherapy[edit | edit source]
Physiotherapists should be involved early and should make their own assessment of how much they can work with a patient. Early mobilisation is associated with better outcomes - even after taking account of the potential confounding influence of disease severity. If rehabilitation is to take place on a different ward from acute care, the care received should be made as seamless as possible. The type and intensity of therapy should be determined by the patient's needs, not location.[11] Review by Harutoshi Sakakima et al. suggests that physical exercise acts as prototypical preconditioning stimuli that offer brain protection effects and are safe and workable treatment options for providing endogenous neuroprotection in patients with acute and chronic stroke[12].
A study by Carina U Persson et al. found that age, arm paresis, aphasia, and facial palsy at index stroke were predictors of increased muscle tone seven years post-ischaemic stroke[13]. A randomized study examining the effects of balance training with electromyogram-triggered functional electrical stimulation (EMG-triggered FES) to improve static balance, dynamic balance, and ankle muscle activation suggest positive results with stroke patients[14].
A single-blinded randomized controlled trial comparing the effectiveness of self-initiated sit-to-stand training with an assistive device with manual sit-to-stand training in a rehabilitation hospital of Hong Kong suggests positive outcomes with self-initiated sit-to-stand training on speeding up regaining the independence of sit-to-stand on sub-acute stroke survivors[15]. A Systematic Review suggests that only lifestyle interventions that include specific strategies targeting physical activity have a positive outcome on physical activity levels as compared to general lifestyle interventions[16].
Primary Goals of Rehabilitation[edit | edit source]
- Prevent complications
- Minimise impairments
- Maximise function
Optimising Post Stroke Rehabilitation[edit | edit source]
- Early assessment with standardized evaluations and validated assessment tools
- Early employment of evidence-based interventions relevant to individual patient needs
- Patient access to an experienced multidisciplinary rehabilitation team
- ongoing medical management of risk factors and co-morbidities
A randomized controlled trial suggests the CARE4STROKE program had a positive outcome on anxiety and depression of the patients[17].
Upper Limb[edit | edit source]
Upper Limb Impairments:
- Subluxation
- Changes in Sensation
- Contracture
- Swelling
- Coordination Problems
- Weakness
- Altered Muscle Power
- Changes in Muscle Tone
- Hand Dysfunction
Aims of Treatment:
- Prevent shoulder pain and if unable to do so, manage should pain effectively.
- Be selective when choosing compensatory versus remedial intervention methods to treat clients who are predicted to have a low return of motor function and poor functional use of their arm and hand.
- Provide remedially focused rehabilitation to clients who are predicted to change in arm and hand function.
- Use measures of known reliability and evidence of validity for treatment planning and outcome prediction.
In the upper extremity with severe impairment and/or poor prognosis for recovery (Chedoke McMaster Stroke Assessment (CMSA) of Arm and Hand < Stage 4) treatment should focus on maintaining a comfortable, pain-free, mobile arm and hand[18][19].
- Focus on proper positioning to provide support at rest and careful handling during functional activities
- Participate in classes supervised by professional rehabilitation clinicians in institutional or community settings that teach the client and caregiver to perform a self range of motion exercises.
- Avoid the use of overhead pulleys (risk of shoulder tissue injury)
- Use some means of external support for stage 1 or 2 upper limbs during transfers and mobility
- Place arm and hand in a variety of positions that include placement within the client’s visual field
- Use some means of external support to protect the upper limb during wheelchair use
In the upper extremity with moderate impairments who show high motivation and potential for functional motor gains (CMSA => stage 4)[18][19]
- Engage in repetitive and intense use of novel tasks that challenge the stroke survivor to acquire necessary motor skills to use the involved upper limb during functional tasks and activities
- Engage in motor-learning training including the use of imagery.
Treatment Techniques:
- Strength Training - There is evidence that strength training can improve upper-limb strength and function without increasing tone or pain in individuals with stroke[20][21]. A randomized study examining the effects of balance training with electromyogram-triggered functional electrical stimulation (EMG-triggered FES) to improve static balance, dynamic balance, and ankle muscle activation suggest positive results with stroke patients. A Randomized Controlled Trial showed improvement in strength and motor function in patients after subacute stroke with high-intensity and low-intensity arm resistance training[22].
- Modified Constraint-Induced Movement Therapy (mCIMT) and CIMT address learned non-use and decreased motor function in an upper extremity affected by post stroke[23] Some studies suggest that performing aerobic exercise prior to m-CIMT enhances the outcomes[24].
- Orthotics - therapy incorporating a dynamic wrist-hand orthosis may be no better than manual therapy[25]. Long-term use of static orthoses requires complementary appropriate treatment opportunities to prevent clenched fist, problems with ADL and hygiene maintenance.[26]
- Gaming - goal-orientated computer gaming has proven to significantly reduce upper limb impairment in stroke survivors[27][28]
- Virtual Reality - virtual reality training has been shown to be effective in restoring upper limb motor impairments and motor-related functional abilities[29][30]
- Mirror Therapy - Mirror therapy has been shown to have a beneficial effect on motor control and function compared with conventional therapy[31][32][33]
- Robot-Assisted Therapy - has been shown to have a beneficial effect on motor recovery and function[34][35][36]
Clinical Guidelines[edit | edit source]
Overall Management: National clinical guideline for stroke, The Royal College of Physicians, September 2012
- Canadian Best Practice Recommendations for Stroke Care. Heart and Stroke Foundation and the Canadian Stroke Network,Ottawa, Ontario Canada, 2013 (see also 2010 Canadian Best Practice Recommendations for Stroke Care).
- Stroke Management. National Stroke Foundation, Australia, 2010.
- Guidelines from the American Heart Association/American Stroke Association
Acute Care
- Stroke: Diagnosis and Initial Management of Acute Stroke and Transient Ischaemic Attack. NICE Guidelines, 2008.
Rehabilitation
- Stroke Rehabilitation: Long-term Rehabilitation after Stroke. NICE Guidelines, 2014.
- Clinical Guidelines for Stroke Management A Quick Guide for Physiotherapy. National Stroke Foundation, Australia, 2010.
- Clinical Practice Guideline for Physical Therapy in Patients with Stroke. Royal Dutch Society for Physical Therapy (KNGF), 2014.
- Canadian Best Practice Recommendations for Stroke Care: Stroke Rehabilitation. Heart and Stroke Foundation and the Canadian Stroke Network,Ottawa, Ontario, Canada, 2013.
Enhancing Healthcare Team Outcomes[edit | edit source]
- The prevention and management of stroke are best done with an interprofessional team approach.
- Education of the public and Emergency Medical Services(EMS) are extremely important in improving stroke outcomes.
- During the time-dependent early stroke phase and rehabilitation, stroke care involves an interprofessional team to manage the disease. Evidence reveals that hospitals with stroke teams with demonstrated knowledge in stroke and decreased door to needle times have decreased mortality and improved outcomes.
- Once the diagnosis of stroke is made and acutely treated, the patient may need extensive physical rehabilitation, speech therapy and/or a dietary consult.
- For those who recover function within 3 months, the prognosis is good, but for those with residual neurological deficits, the outcome is guarded.
- Nurses and physical therapists at this point played a crucial role in providing family and patient education as often activities of daily living may be a challenge.
- Secondary prevention after an acute stroke depends on the underlying stroke mechanism.
- Management of stroke is one of the single most difficult and challenging issues for health professionals. Only through an interprofessional approach will the best outcomes be achieved.[1]
Resources[edit | edit source]
- Stroke Scales & Clinical Assessment Tools
- The Evidence-Based Review of Stroke Rehabilitation (EBRSR) is a comprehensive and up-to-date review available examining therapy-based (and also pharmacological) interventions associated with stroke rehabilitation.
Presentations[edit | edit source]
 |
Stroke: PT Assessment and Management
This presentation, created by Dr. L. Surbala (MPT Neuro), discusses etiology, risk factors, stages of recovery, impairments and recovery from stroke. |
 |
Best Practices in Stroke Rehabilitation: The US Experience
This presentation, created by Dr. R.D. Zorowitz MD, discusses current practices in stroke rehabilitation. Best Practices in Stroke Rehabilitation: The US Experience/ View the presentation |
 |
Management of Upper Limb Post Stroke with Recent Advances
This presentation, created by Eusivia Pasi MPT, discusses current practices in stroke rehabilitation. |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Tadi P, Lui F. Acute Stroke (Cerebrovascular Accident). Available from: https://www.ncbi.nlm.nih.gov/books/NBK535369/ (last accessed 28.12.2019)
- ↑ Global Burden of Stroke. The Atlas of Heart Disease and Stroke. MacKay J, Mensah GA. World Health Organization.
- ↑ Townsend N, Wickramasinghe K, Bhatnagar P, Smolina K, Nichols M, Leal J, Luengo-Fernandez R, Rayner M (2012). Coronary heart disease statistics 2012 edition. British Heart Foundation: London. P21
- ↑ Cal Shipley, M.D. What Is A Stroke? - Narration and Animation by Cal Shipley, M.D. Available from: http://www.youtube.com/watch?v=uLJewzJcCZ0 [last accessed 10/10/14]
- ↑ Zafar F, Tariq W, Shoaib RF, Shah A, Siddique M, Zaki A, Assad S. Frequency of ischemic stroke subtypes based on toast classification at a tertiary care center in Pakistan. Asian journal of neurosurgery. 2018 Oct;13(4):984. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6208235/ (last accessed 28.12.2019)
- ↑ USMLEFastTrack. Effects of Strokes - Middle Cerebral Artery. Available from: http://www.youtube.com/watch?v=6sk7AXNw9Ns [last accessed 10/10/14]
- ↑ USMLEFastTrack. Effects of Strokes - Posterior Cerebral Artery. Available from: http://www.youtube.com/watch?v=OFlL9Dm8qCM [last accessed 10/10/14]
- ↑ USMLEFastTrack. Effects of Strokes - Anterior Cerebral & Lateral Striate Artery. Available from: http://www.youtube.com/watch?v=NSWnNnfDt70 [last accessed 10/10/14]
- ↑ Lin JH, Hsu MJ, Hsu HW, Wu HC, Hsieh CL. Psychometric Comparisons of 3 Functional Ambulation Measures for Patients With Stroke. Stroke. 2010 Jul 29; online article ahead of print
- ↑ Adams H, Adams R, Del Zoppo G, Goldstein LB. Guidelines for the early management of patients with ischemic stroke: 2005 guidelines update a scientific statement from the Stroke Council of the American Heart Association/American Stroke Association. Stroke. Apr 2005;36(4):916-23.
- ↑ Harwood R, Huwez F, Good D. Stroke Care: A practical manual. New York: Oxford, 2011.
- ↑ Matsuda F, Sakakima H, Yoshida Y. The effects of early exercise on brain damage and recovery after focal cerebral infarction in rats. Acta physiologica. 2010 Jul:no-.
- ↑ Wissel J, Verrier M, Simpson DM, Charles D, Guinto P, Papapetropoulos S, Sunnerhagen KS. Post-stroke spasticity: predictors of early development and considerations for therapeutic intervention. PM&R. 2015 Jan 1;7(1):60-7.
- ↑ Lee K. Balance Training with Electromyogram-Triggered Functional Electrical Stimulation in the Rehabilitation of Stroke Patients. Brain Sciences. 2020 Feb;10(2):80.
- ↑ Joey NC, Ho Marc WK. Does self-initiated sit-to-stand training with an assistive device regain the independence of sit-to-stand in stroke patient? A single-blinded randomized controlled trial. Journal of Rehabilitation and Assistive Technologies Engineering. 2020 Jan;7:2055668319866053.
- ↑ Hendrickx W, Vlietstra L, Valkenet K, Wondergem R, Veenhof C, English C, Pisters MF. General lifestyle interventions on their own seem insufficient to improve the level of physical activity after stroke or TIA: a systematic review. BMC neurology. 2020 Dec;20:1-3.
- ↑ Vloothuis JD, Mulder M, Nijland RH, Goedhart QS, Konijnenbelt M, Mulder H, Hertogh CM, Van Tulder M, Van Wegen EE, Kwakkel G. Caregiver-mediated exercises with e-health support for early supported discharge after stroke (CARE4STROKE): A randomized controlled trial. PloS one. 2019 Apr 8;14(4):e0214241.
- ↑ 18.0 18.1 Norine Foley, Swati Mehta, Jeffrey Jutai, Elizabeth Staines, Robert Teasell. Upper Extremity Interventions. EBRSR, 2013
- ↑ 19.0 19.1 Susan Barreca et al. Management of the Post Stroke Hemiplegic Arm and Hand: Treatment: Recommendations of the 2001 Consensus Panel. Heart and Stroke Foundation of Ontario, 2001.
- ↑ Carolynn Patten, Elizabeth G Condliffe, Christine A Dairaghi5 and Peter S Lum. Concurrent neuromechanical and functional gains following upper-extremity power training post-stroke. Journal of NeuroEngineering and Rehabilitation 2013, 10:1
- ↑ Harris JE, Eng JJ. Strength training improves upper-limb function in individuals with stroke: a meta-analysis. Stroke. 2010 Jan;41(1):136-40.
- ↑ Högg S, Holzgraefe M, Drüge C, Hauschild F, Herrmann C, Obermann M, Mehrholz J. High-intensity arm resistance training does not lead to better outcomes than low-intensity resistance training in patients after subacute stroke: A randomized controlled trial. Journal of rehabilitation medicine. 2020 May 5.
- ↑ Barzel A, Ketels G, Stark A, Tetzlaff B, Daubmann A, Wegscheider K, van den Bussche H, Scherer M. Home-based constraint-induced movement therapy for patients with upper limb dysfunction after stroke (HOMECIMT): a cluster-randomised, controlled trial. The Lancet Neurology. 2015 Sep 1;14(9):893-902.
- ↑ da Silva, E.S.M., Santos, G.L., Catai, A.M., Borstad, A., Furtado, N.P.D., Aniceto, I.A.V. and Russo, T.L., 2019. Effect of aerobic exercise prior to modified constraint-induced movement therapy outcomes in individuals with chronic hemiparesis: a study protocol for a randomized clinical trial. BMC neurology, 19(1), p.196.
- ↑ Barry JG1, Ross SA, Woehrle J. Therapy incorporating a dynamic wrist-hand orthosis versus manual assistance in chronic stroke: a pilot study. J Neurol Phys Ther. 2012 Mar;36(1):17-24.
- ↑ Aukje Andringa, Ingrid van de Port, and Jan-Willem Meijer. Long-Term Use of a Static Hand-Wrist Orthosis in Chronic Stroke Patients: A Pilot Study. Stroke Research and Treatment, 2013.
- ↑ Ann Reinthal, Kathy Szirony, Cindy Clark, Jeffrey Swiers, Michelle Kellicker and Susan Linder. ENGAGE: Guided Activity-Based Gaming in Neurorehabilitation after Stroke: A Pilot Study. troke Research and Treatment, Volume 2012 (2012), Article ID 784232, 10 pages
- ↑ Jordan, Kimberlee; Sampson, Michael; King, Marcus. ;atlitid=212008 Table-Top Exergaming Improves Arm Function in Chronic Stroke. Rehabilitation Engineering and Assistive Technology Society of North America, 2013
- ↑ Andrea Turolla1, Mauro Dam1, Laura Ventura, Paolo Tonin, Michela Agostini, Carla Zucconi, Pawe Kiper, Annachiara Cagnin and Lamberto Piron. Virtual reality for the rehabilitation of the upper limb motor function after stroke: a prospective controlled trial. Journal of NeuroEngineering and Rehabilitation 2013, 10:85
- ↑ S Bermúdez i Badia, E Lewis, S Bleakley. [http://www.researchgate.net/publication/236682630_Combining_virtual_reality_and_a_myo-electric_limb_orthosis_to_restore_active_movement_after_stroke_a_pilot_study Combining virtual reality and a myo-electric limb orthosis to restore active movement after stroke: a pilot study�]. Proc. 9th Intl Conf. Disability, Virtual Reality Associated Technologies Laval, France, 10–12 Sept. 2012
- ↑ Thieme H, Mehrholz J, Pohl M, Behrens J, Dohle C. Mirror therapy for improving motor function after stroke. Cochrane Review, 2012
- ↑ Ching-Yi Wu, Pai-Chuan Huang, Yu-Ting Chen, Keh-Chung Lin, Hsiu-Wen Yang. Effects of Mirror Therapy on Motor and Sensory Recovery in Chronic Stroke: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation, American Congress of Rehabilitation Medicine, 2013
- ↑ Lee, Myung Mo; Cho, Hwi-young; Song, Chang Ho. The Mirror Therapy Program Enhances Upper-Limb Motor Recovery and Motor Function in Acute Stroke Patients. American Journal of Physical Medicine and Rehabilitation: August 2012 - Volume 91 - Issue 8 - p 689–700
- ↑ Nahid Norouzi-Gheidari, Philippe S. Archambault, Joyce Fung. Effects of robot-assisted therapy on stroke rehabilitation in upper limbs: Systematic review and meta-analysis of the literature. JRRD, 2012, 49 (4), 479–496
- ↑ Patrizio Sale1, Marco Franceschini1, Stefano Mazzoleni, Enzo Palma1, Maurizio Agosti and Federico Posteraro. Effects of upper limb robot-assisted therapy on motor recovery in subacute stroke patients. Journal of NeuroEngineering and Rehabilitation 2014, 11:104
- ↑ Kwakkel G, Kollen BJ, Krebs HI. Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Neurorehabil Neural Repair. 2008 Mar-Apr;22(2):111-21. Epub 2007 Sep 17.