Epidemiology, Incidence and Global Burden of Stroke
Original Editor - Naomi O'Reilly
Top Contributors - Rachael Lowe, Lucinda hampton, Kim Jackson, Simisola Ajeyalemi, Rucha Gadgil and Amanda Ager
Introduction[edit | edit source]
Stroke is the second leading cause of death and a major cause of disability worldwide. Its incidence is increasing because the population ages.
In addition, more young people are affected by stroke in low- and middle-income countries. Ischemic stroke is more frequent but hemorrhagic stroke is responsible for more deaths and disability-adjusted life-years (DALY) lost. Incidence and mortality of stroke differ between countries, geographical regions, and ethnic groups. In high-income countries mainly, improvements in prevention, acute treatment, and neurorehabilitation have led to a substantial decrease in the burden of stroke over the past 30 years.
- The latest estimate from the Global Burden of Disease (GBD 2015) shows a further shift from communicable diseases, maternal and nutritional causes, towards noncommunicable diseases like stroke.
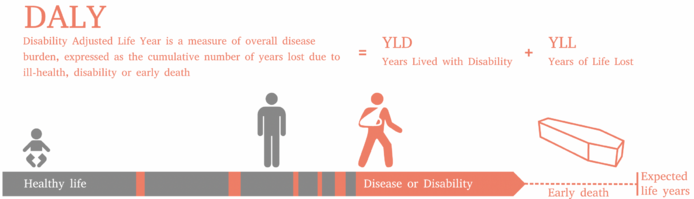
- According to the 2010 Global Burden of Disease Study, Stroke categorised under Cardiovascular and Circulatory Diseases, is the second leading cause of death globally and the third leading cause of premature death and disability as measured in Disability Adjusted Life Years (DALY). Cerebrovascular disease is the largest neurologic contributor and accounts for 4.1% of total global DALY.
Almost half of stroke-related mortality may be attributable to modifiable risk factors (i.e. hypertension, diabetes, dietary risks, impaired glucose intolerance, obesity, smoking, air pollution, alcohol use, hyperlipidemia, and physical inactivity). This is mainly due to the outcome of poor clinical management, limited access to health care, and late detection of underlying risk factors. This occurs often as a result of the societal barriers in lower socioeconomic groups, where the burden is the greatest. Social and economic policies to reduce inequalities in stroke care should become a health priority, particularly in less wealthy countries. The policies should focus on treating early predisposing factors and on educational programmes from childhood, which have long-lasting impacts on adulthood health. Similarly improving worldwide primary healthcare services may have an important impact on post-stroke outcomes. Improving stroke awareness among socioeconomically deprived individuals and societies and providing equitable post-stroke medical care is essential.[1]
Global Burden of Stroke[edit | edit source]
Global burden of disease (GBD) measures burden of disease using the DALY[2].
The global burden of Stroke is increasing globally[3][4].
In the last decades, a substantial decrease of stroke incidence, mortality, and DALYs has been achieved in high-income countries, most likely due to improvement in primary and secondary prevention as well as acute stroke treatment and neurorehabilitation. However
- Stroke remains an important cause of disability and death worldwide.
- Globally, the burden of stroke has increased substantially over the past few decades due to expanding population numbers and aging as well as the increased prevalence of modifiable stroke risk factors, especially in low- and middle-income countries.
- The number of patients who will need care by clinicians with expertise in neurological conditions will continue to grow in the coming decades.[5]
Individual burden of Ischaemic and Hemorrhagic Stroke[edit | edit source]
Hemorrhagic Stroke
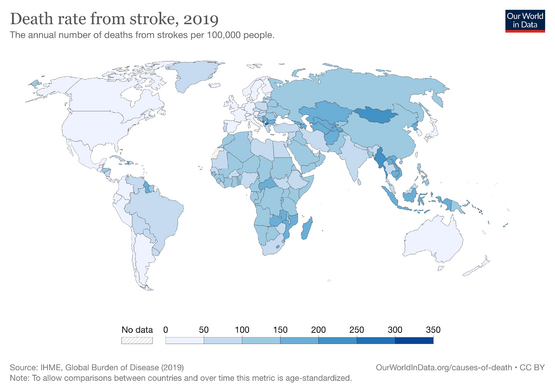
The worldwide burden of haemorrhagic stroke (HS) has increased over the last 2 decades[6] in terms of absolute numbers of HS incident events. The majority of the burden of HS is borne by LMIC. Rates for HS incidence, mortality, and DALY lost, as well as MIR decreased in the past 2 decades in HIC, but increased significantly in LMIC countries, particularly in those patients 75 years. HS affected people at a younger age in LMIC than in HIC. The lowest incidence and mortality rates in 2010 were in High Income North America, Australasia, and Western Europe, whereas the highest rates were in Central Asia, Southeast Asia, and sub-Saharan Africa[7].
Ischaemic Stroke
Although age-standardized ischaemic stroke (IS) mortality rates have declined over the last 2 decades, the absolute global burden of IS is increasing, with the bulk of DALY lost in LMIC. Tobacco consumption is an important modifiable risk factor for IS, and in both 1990 and 2010, the top ranked countries for IS deaths that could be attributed to tobacco consumption were China, Russia, and India. Tobacco control policies that target both smoking initiation and smoking cessation can play an important role in the prevention of IS. In China, Russia, and India, even modest reductions in the number of current smokers could see millions of lives saved due to prevention of IS alone[8].
Stroke Disparities[edit | edit source]
Stroke disparities are widespread and universal. Complex interwoven issues of inability to afford optimal medical infrastructure and personnel, unequal access to medical care (if available), low medical literacy, and problems with adherence and compliance all limit the effectiveness of primary and secondary prevention in stroke care. Factors such as geography, age, sex, ethnicity, and socioeconomic status (SES) interact and modify the incidence and prevalence of stroke.[5]
Risk Factors[edit | edit source]
Feigin et al[9]suggest that more than 90% of the stroke burden is attributable to modifiable risk factors, and achieving control of behavioural and metabolic risk factors could avert more than three-quarters of the global stroke burden. Air pollution has emerged as a significant contributor to global stroke burden, especially in low-income and middle-income countries, and therefore reducing exposure to air pollution should be one of the main priorities to reduce stroke burden in these countries. Identification and adequate management of risk factors are key to preventing any disease or injury.
The major risk factors for stroke include:
- Hypertension, Diabetes, Heart conditions eg coronary heart disease, cardiomyopathy, heart failure, and atrial fibrillation.
- Smoking
- Age and gender - your risk of stroke increases as you get older. At younger ages, men are more likely than women to have strokes. However, women are more likely to die from strokes. Women who take birth control pills also are at slightly higher risk of stroke.
- Race and ethnicity - strokes occur more often in African American, Alaska Native, and American Indian adults than in white, Hispanic, or Asian American adults.
- Personal or family history of stroke or TIA.
- Brain aneurysms or arteriovenous malformations (AVMs)
Other risk factors for stroke, many of which of you can control, include:
- Alcohol and illegal drug use, eg cocaine, amphetamines
- Certain medical conditions, eg sickle cell disease, vasculitis (inflammation of the blood vessels), and bleeding disorders
- Lack of physical activity
- Overweight and Obesity
- Stress and depression
- Unhealthy cholesterol levels, Unhealthy diet
- Use of nonsteroidal anti-inflammatory drugs (NSAIDs)
Many factors are relevant in prioritising strategies to reduce risks to health. These include the extent of the threat posed by different risk factors, the availability of cost-effective interventions, societal values, culture and preferences. Risk assessment and estimates of the burden of disease resulting from different risk factors may be altered by many different strategies.
Stroke Registers[edit | edit source]
In many countries and regions, Stroke Registers, are now being used to gain a greater understanding of the prevalence of Stroke and assist with research and service planning. These registers are databases of clinical information, with the primary aim being collection of key data items to provide information on the quality of care for individual patients with stroke and transient ischaemic attack (TIA) in order to provide high-quality information to identify areas where improvements in quality of care should be prioritised, reduce variations in care delivery and, ultimately, provide evidence of reduced deaths, disability, and recurrent stroke.
- Is there a Stroke Register in your Country?
- Do you keep a register within your practice of individuals with Stroke in order to plan for future service requirements?
References[edit | edit source]
- ↑ Avan, A., Digaleh, H., Di Napoli, M., Stranges, S., Behrouz, R., Shojaeianbabaei, G., Amiri, A., Tabrizi, R., Mokhber, N., Spence, J.D. and Azarpazhooh, M.R., 2019. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the Global Burden of Disease Study 2017. BMC medicine, 17(1), p.191. Available from: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1397-3 (last accessed 15.1.2020)
- ↑ Mathers C, Fat DM, Boerma JT. The global burden of disease: 2004 update. World Health Organization; 2008.
- ↑ Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T, O'Donnell M. Global and Regional Burden of Stroke during 1990–2010: Findings from the Global Burden of Disease Study 2010. The Lancet. 2014 Jan 24;383(9913):245-55.
- ↑ Feigin VL, Krishnamurthi RV, Parmar P, Norrving B, Mensah GA, Bennett DA, Barker-Collo S, Moran AE, Sacco RL, Truelsen T, Davis S. Update on the global burden of ischemic and hemorrhagic stroke in 1990-2013: the GBD 2013 study. Neuroepidemiology. 2015 Oct 28;45(3):161-76.
- ↑ 5.0 5.1 Katan M, Luft A. Global burden of stroke. InSeminars in neurology 2018 Apr (Vol. 38, No. 02, pp. 208-211). Thieme Medical Publishers Available:https://www.thieme-connect.de/products/ejournals/html/10.1055/s-0038-1649503 (accessed 18.8.2021)
- ↑ Feigin VL, Mensah GA, Norrving B, Murray CJ, Roth GA. Atlas of the Global Burden of Stroke (1990-2013): the GBD 2013 study. Neuroepidemiology. 2015 Oct 28;45(3):230-6
- ↑ Krishnamurthi RV, Moran AE, Forouzanfar MH, Bennett DA, Mensah GA, Lawes CM, Barker-Collo S, Connor M, Roth GA, Sacco R, Ezzati M. The global burden of hemorrhagic stroke: a summary of findings from the GBD 2010 study. Global heart. 2014 Mar 31;9(1):101-6.
- ↑ Krishnamurthi RV, Barker-Collo S, Forouzanfar MH, Naghavi M, Connor M, Lawes CM, Moran AE, Anderson LM, Roth GA, Mensah GA. The global burden of ischemic stroke: findings of the GBD 2010 study. Global heart. 2014 Mar 31;9(1):107-12.
- ↑ Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, Mensah GA, Norrving B, Shiue I, Ng M, Estep K. Global Burden of Stroke and Risk Factors in 188 Countries, during 1990–2013: A Systematic Analysis for the Global Burden of Disease Study 2013. The Lancet Neurology. 2016 Aug 31;15(9):913-24