Autoimmune Disorders
Introduction[edit | edit source]
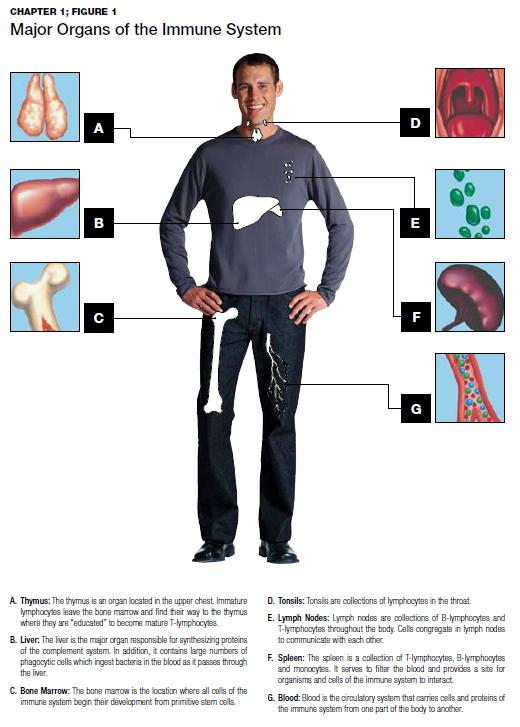
The immune system protects you from disease and infection. Sometimes, though, the immune system can produce autoantibodies that attack healthy cells, tissues, and organs. This can lead to autoimmune disease. Autoimmune diseases (AID) are a collection of many complex disorders of unknown etiology resulting in immune responses to self-antigens and are thought to result from interactions between genetic and environmental factors[1]. Autoimmunity contributes to more than 100 serious chronic illnesses that involve almost every organ system in the human body. Almost all autoimmune diseases affect women more often than men. Some of these diseases are cited in the top-10 leading causes of death in women aged 65 and younger, and together, they represent the fourth-largest cause of disability among women in America[2].
A Brief History[edit | edit source]
In the 1900s the idea of autoimmunity first surfaced. and by the 1940's it was recognised as a reasonable cause for a disease. In 1992, only 67 AIDs had been identified. Today, there are more than 100, and there are thought to be about 50 million Americans living with autoimmunity, 30 million of which are women. In the past decade the numbers have risen again[2]. Many of these diseases are increasing in frequency in industrialised countries. Treatment of autoimmune diseases improved greatly during the second half of the 20th century but has been hampered because the diseases often progress before a clinical diagnosis is possible. It does appear that a close interplay between environmental triggers and genetic factors is responsible for the loss of immunological tolerance and autoimmunities. Future directions are trying to unravel the connections between genetic predisposition and environmental triggers.
Some autoimmune diseases are life-threatening, and most are debilitating and require a lifetime of treatment. There are treatments available to reduce the symptoms and effects from many autoimmune diseases, but cures have yet to be discovered. Since most autoimmune diseases are rare, patients can often spend years seeking a proper diagnosis.
Unraveling Environmental and Lifestyle Risks[edit | edit source]
Physical Activity[edit | edit source]
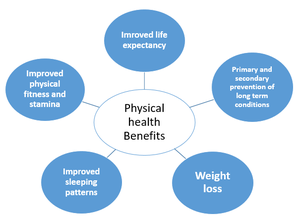
A 2018 report on the influence of [3] found it is a safe option in most of autoimmune diseases including systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), multiple sclerosis (MS), inflammatory bowel diseases (IBD), as well as others. Additionally, the incidence of RA, MS, IBD and psoriasis has been found to be higher in patients less engaged in physical activity. As a general trend, patients with autoimmune diseases tend to be less physically active as compared to the general population. Physically active RA patients were found to have a milder disease course, better cardiovascular disease (CVD) profile, and improved joint mobility. Physical activity decreases fatigue, enhances mood, cognitive abilities and mobility in patients with MS. In SLE patients, enhanced quality of life and better CVD profile were documented in more physically active patients. Physically active patients with type 1 diabetes mellitus have a decreased risk of autonomic neuropathy and CVD. Both fibromyalgia and systemic sclerosis patients report decreased disease severity, pain, as well as better quality of life with more physical activity[4]. A 2015 orthopaedic report stated that inactivity in patients with rheumatic diseases is very harmful both physically (reduced muscle strength, deconditioning, greater rigidity), and psychologically (fear of movement, depression, loss of self-confidence). Physical exercise can play a crucial role in the treatment of rheumatic diseases, optimizing both physical and mental health, enhancing energy, decreasing fatigue and improving sleep..[5]
Obesity[edit | edit source]
Obesity appears to be a major environmental factor contributing to the onset and progression of autoimmune diseases. Fat tissue has been found to produce a wide variety of "adipokines", involved in the regulation of numerous physiological functions, including the immune response. The strongest levels of evidence support an increased risk of RA , MS, psoriasis and psoriatic arthritis (PsA) in obese subjects. A higher risk of IBD, type-1 diabetes (T1D) and thyroid autoimmunity (TAI)is also suggested. Moreover, obesity worsens the course of RA, SLE, IBD, psoriasis and PsA, and impairs the treatment response of RA, IBD, psoriasis and PsA.[6]
Stress[edit | edit source]
The treatment for autoimmune disease should include stress management. Stress is probably a participating factor. Indeed, a high proportion of patients with auto-immune diseases report uncommon stress before disease onset or disease flare[7].
Smoking[edit | edit source]
Cigarette smoking has been causally linked to the development of multiple autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, Graves' hyperthyroidism, and primary biliary cirrhosis, among others.[8]
Toxins[edit | edit source]
A 2012 study into environmental exposures and human autoimmune diseases concluded that [1]
- Crystalline silica exposure can contribute to the development of several AIDs eg in glass, granite and stone cutting jobs exposing workers to silica dust.
- Solvent exposure can contribute to the development of systemic sclerosis;
- Smoking can contribute to the development of seropositive rheumatoid arthritis;
- An inverse association exists between ultraviolet radiation exposure and the risk of development of multiple sclerosis.
Drug Induced Autoimmune Syndromes[edit | edit source]
The number and complexity of drug-induced autoimmune syndromes has increased, and many are now associated with autoantibodies that have been classically defined as limited to idiopathic disease states.[9]
Diet[edit | edit source]
The influences of diet, nutrition, oral hygiene, exercise and BMI also play a role in the development AIDs
A 2019 study found a potential new link between pork consumption and autoimmunity in humans[10].
Oral manifestations of autoimmune disease are frequently the primary sign of autoimmune diseases. The dentists can therefore play a pivotal role in the detection and during the following multidisciplinary treatment[11]
Physiotherapy[edit | edit source]
As physiotherapists we are ideally placed to tackle many of the causative and current problems with clients. Drugs offer little in the way of this.
- Physical activity - planning, implementing and doing follow ups on exercise programs; encouraging correct options eg aim for 30 minutes walking 3 times weekly, working to this goal; educating re slow results but worth it.
- Diet - advise and educate about healthy food choices and quantities, refer when necessary.
- Toxin avoidance - smoking being an obvious one, and alert to second hand smoke risks.
- Stress - if able teach stress relieving techniques eg Yoga, CBT, Tai Chi, Breathing control, Meditation.
Conclusion[edit | edit source]
To better understand and treat specific autoimmune disease see here.
References[edit | edit source]
- ↑ 1.0 1.1 Miller FW, Alfredsson L, Costenbader KH, Kamen DL, Nelson LM, Norris JM, De Roos AJ. Epidemiology of environmental exposures and human autoimmune diseases: findings from a National Institute of Environmental Health Sciences Expert Panel Workshop. Journal of autoimmunity. 2012 Dec 1;39(4):259-71. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22739348 (last accessed 29.9.2019)
- ↑ 2.0 2.1 Amy Scanlin, MS. Autoimmune disease: The growing impact.BioSupply Trends Quarterly • April 2014 p47 Available from: http://www.bstquarterly.com/Assets/downloads/BSTQ/Articles/BSTQ_2014-04_AR_Autoimmune-Disease-The-Growing-Impact.pdf (last accessed 29.9.2019)
- ↑ Sharif K, Watad A, Bragazzi NL, Lichtbroun M, Amital H, Shoenfeld Y. Physical activity and autoimmune diseases: Get moving and manage the disease. Autoimmunity reviews. 2018 Jan 1;17(1):53-72.Available from: https://www.ncbi.nlm.nih.gov/pubmed/29108826 (last accessed 29.9.2019)
- ↑ Sharif K, Watad A, Bragazzi NL, Lichtbroun M, Amital H, Shoenfeld Y. Physical activity and autoimmune diseases: Get moving and manage the disease. Autoimmunity reviews. 2018 Jan 1;17(1):53-72.Available from: https://www.ncbi.nlm.nih.gov/pubmed/29108826 (last accessed 29.9.2019)
- ↑ Musumeci G. Effects of exercise on physical limitations and fatigue in rheumatic diseases. World journal of orthopedics. 2015 Nov 18;6(10):762. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4644863/ (last accessed 29.9.2019)
- ↑ Lago F, Dieguez C, Gómez-Reino J, Gualillo O. The emerging role of adipokines as mediators of inflammation and immune responses. Cytokine & growth factor reviews. 2007 Jun 1;18(3-4):313-25. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25092612 (last accessed 29.9.2019)
- ↑ Stojanovich L. Stress and autoimmunity. Autoimmunity reviews. 2010 Mar 1;9(5):A271-6. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23182292 (last accessed 29.9.2019)
- ↑ Costenbader KH, Karlson EW. Cigarette smoking and autoimmune disease: what can we learn from epidemiology?. Lupus. 2006 Nov;15(11):737-45. Available from: https://journals.sagepub.com/doi/10.1177/0961203306069344 (last accessed 29.9.2019)
- ↑ Olsen NJ. Drug-induced autoimmunity. Best Practice & Research Clinical Rheumatology. 2004 Oct 1;18(5):677-88. Available from:https://www.ncbi.nlm.nih.gov/pubmed/15454126 (last accessed 30.9.2019)
- ↑ Gershteyn IM, Ferreira LM. Immunodietica: A data-driven approach to investigate interactions between diet and autoimmune disorders. Journal of Translational Autoimmunity. 2019 Jun 6:100003. Available from: https://www.biorxiv.org/content/10.1101/619700v1 (last accessed 29.9.2019)
- ↑ Saccucci M, Di Carlo G, Bossù M, Giovarruscio F, Salucci A, Polimeni A. Autoimmune diseases and their manifestations on oral cavity: diagnosis and clinical management. Journal of immunology research. 2018;2018. Available from: https://www.hindawi.com/journals/jir/2018/6061825/ (last accessed 29.9.2019)