Multiple Sclerosis (MS)
Original Editor - Sarah Demarest Beth Niehbur Bram Van Laer
Top Contributors - Elizabeth Niebuhr, Vidya Acharya, Sarah Demarest, Laura Ritchie, Nikhil Benhur Abburi, Garima Gedamkar, Kim Jackson, Bram Van Laer, Lucinda hampton, Admin, Eta Frida, Rachael Lowe, Magdalena Hytros, WikiSysop, Naomi O'Reilly, Venus Pagare, Sheik Abdul Khadir, 127.0.0.1, Elaine Lonnemann, Wendy Walker, Evan Thomas, Memoona Awan, Elien Lebuf, Tarina van der Stockt, Rucha Gadgil, Jaroslaw Pospiech, Jess Bell and Rishika Babburu
Introduction[edit | edit source]
Multiple sclerosis (MS) is an autoimmune disease of the central nervous system (CNS) characterized by chronic inflammation, demyelination, gliosis, and neuronal loss. The course may be relapsing-remitting or progressive. Lesions in the CNS occur at different times and in different CNS locations. Because of this, multiple sclerosis lesions are sometimes said to be "disseminated in time and space." The clinical course of the disease is quite variable ranging from stable chronic disease to a rapidly evolving and debilitating illness. The most common form of the disease is relapsing-remitting multiple sclerosis; however, several other forms exist.[1]
Definition/Description[edit | edit source]
Multiple sclerosis (MS) involves an immune-mediated process in which an abnormal response of the body’s immune system is directed against the central nervous system (CNS). The CNS is made up of the brain, spinal cord and optic nerves.
Within the CNS, the immune system causes inflammation that damages myelin — the fatty substance that surrounds and insulates the nerve fibres — as well as the nerve fibres themselves, and the specialized cells that make myelin. Demyelination leads to decreased nerve conduction velocity and early fatigue of the nerve. Gliosis occurs when demyelinated areas become fibrotic, causing the proliferation of neuroglial tissue and scarring in the CNS. [2]
The course that MS can take will be different from one person to another as well as unpredictable. The disease can be divided into four clinical subtypes which describe how the disease will progress as well as the corresponding characteristics that become evident for each subtype:
- Relapsing-remitting MS (RRMS) is the most common subtype, affecting 85% of people with MS and is characterized by short attacks to the CNS followed by a complete or partial return to normal functioning[2].
- Secondary-progressive MS (SPMS) is a subgroup that begins as a relapsing-remitting course accompanied by a steady decline in function and is often developed by the patient.
- Primary-Progressive MS (PPMS) is a progression of the disease where a steady decline in function is experienced from the onset of the disease. Progressive-relapsing MS (PRMS) is similar to PPMS but has the additional characteristic of acute attacks.
Prevalence[edit | edit source]
It is estimated that in the United States, 400,000 people are being affected by MS and 2.1 million people globally[2]. Females are 2 to 3 times more likely to have MS than males, which may indicate hormones play a role in acquiring the; disease.[3] The prevalence of MS has increased within the last 5 decades with the increase primarily being due to females[2]. MS rarely occurs in children as well as adults over the age of 50 and will most commonly present between the ages of 20-40 years.[2] The risk of being diagnosed with MS is increased in a person, who has a sibling with MS by 3%, a fraternal twin by 5% and an identical twin by 25%.[2]
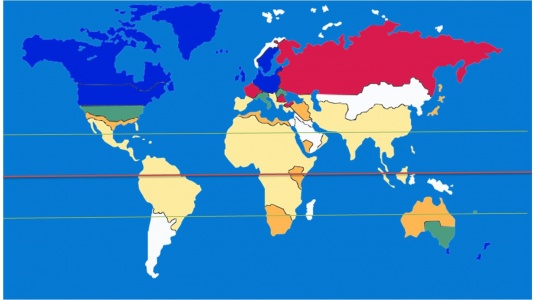
MS can occur in many ethnic groups, with the most common populations being Caucasians with ancestry from northern Europe, followed by African-Americans, Latinos/Hispanics and Asians[3]. It is rarely seen in ethnic populations such as Australian Aborigines, New Zealanders, Yakuts, Inuit, Hungarian Romani and Norwegian Lapps[3]. There have been studies that show the prevalence of MS is higher in some geographical locations than in others, such as the northern United States, northern Europe, southern Canada, New Zealand, Southern Australia and Scandinavian countries. Regions with a lower prevalence of MS tend to be closer to the equator, such as Asia, Africa, and South America[2]. In the image below Blue is high risk. Red is probably high risk. Orange is low risk. Sand is probably low-risk. Green North-South gradient risk. White other risks
Aetiology/Causes[edit | edit source]
The specific cause of multiple sclerosis is unknown. The most widely accepted theory is that multiple sclerosis is an autoimmune disease that preferentially destroys the CNS while the peripheral nervous system is spared. Demyelination causes symptoms of multiple sclerosis. Damage to myelin leads to symptomatic flares in multiple sclerosis. These damaged areas often do not fully recover leading to areas of scarring, damage, and ongoing symptoms. Over time, these cumulative areas of damage can lead to disability. Of note, patients can also develop subclinical areas of damage that are detectable early in the disease course only by radiographic studies[1].
The below factors all appear to have a role in MS development
Immunologic factor. The body's own immune cells attack the CNS and ultimately destroy nerve conduction[3]. Researchers have been able to identify what immune cells are attacking the CNS, the cause for their attack and some of the receptors on the attacking cells that make them attracted to myelin[3]. The T cells (one type of white blood cell in the immune system) somehow become sensitized to proteins in the CNS. When T cells become activated, they enter the CNS through blood vessels and produce damaging inflammation. Once in the CNS, these T cells not only injure myelin but also secrete chemicals that damage nerve fibres (axons) and recruit more damaging immune cells to the site of inflammation. It is not known what causes T cells in persons with MS to become activated but it is postulated that both genetic and environmental factors are important.[4]
Environmental factor. MS appears to be more prevalent in areas farther from the equator in a colder climate. There is some evidence that shows Vitamin D may play an important role in that people who live in a warmer climate are exposed to the sun more and therefore their body naturally produces more Vitamin D. It is thought that larger amounts of naturally produced Vitamin D may increase immune function and protect the body against autoimmune diseases[3].
Genetic factor. The risk of MS increases in a person who has a first-degree family member with the disease, however, MS is not considered to be hereditary. Studies have shown that in populations with higher rates of MS as well as in families where several members have MS there are similar genetic factors. The common genetic factors are continuing to be studied in the role they play in developing MS.[3]
Infectious factor. There is a possibility that viruses and other infectious agents may trigger the onset of MS. Many viral and bacterial infections are being investigated. A study [5] suggests the possibility of virus or virus-triggered immunopathology in MS, suggesting virus reactivating after years of latency. The argument of viral cause is supported by the presence of oligoclonal bands in the brain and cerebrospinal fluid, which persists throughout the lifetime. The presence of oligoclonal bands is found exclusively in infectious CNS disorders. The contribution of the Epstein-Barr virus to the cause of MS is not yet established, but a relationship is present.[6][7]
Gut microbiome factor. It is hypothesized that gastrointestinal microbiota might play an important role in the pathogenesis of MS. Recent evidence suggests that gut microbiota is one of the key environmental factors.[8] According to the “hygiene hypothesis”, reduced exposure to infections in childhood may increase the risk of allergic and autoimmune diseases. Supporting this argument, western societies report an increased incidence of diseases with an autoimmune/allergic component, including MS. Increased constipation, faecal incontinence, increased gut permeability and increased occurrence of inflammatory bowel diseases in MS patients and their families, suggesting an important gut–CNS connection. Interestingly, gut bacteria can also influence the blood-brain barrier integrity. However, research says, it is difficult to say with certainty whether changes in gut microbiota are a cause or consequence of MS because MS patients have immunological and microbial changes months to years before the clinical onset of the disease. So further research is needed to determine the role of gut microbiota and their metabolites in the susceptibility to and protection from MS.[9]
| Mechanisms of Multiple Sclerosis[10] | |
| Feature | Disease Mechanism |
| Autoimmunity | MS is a cell-mediated autoimmune disease directed against CNS myelin antigens that involve both CD4+ and CD8+ cells. Autoantibodies may play a secondary or enhancing role. Autoreactive T cells against myelin components exist in normal individuals and, in these individuals, do not cause disease and may even have brain-protecting properties. MS is induced when pathogenic Th17- and Th1-type and CD8 myelin autoreactive T cells are induced. |
| Infection | Infectious agents play a crucial role in inducing myelin-reactive pathogenic T cells. Potential mechanisms include cross-reactivity with CNS myelin antigens, triggering an already expanded autoreactive immune repertoire or a self-limited infection of the brain that releases myelin antigens. MS is not caused by a persistent viral infection of the brain or a transmissible agent. |
| Genetics | Both MHC and non-MHC genes are risk factors for the development of MS. MHC genes determine immune repertoire whereas non-MHC genes determine regulatory and tolerance mechanisms in MS, both of which are defective. |
| Environment | Environmental factors can increase the risk for both the development of MS and the disease course and include lowered vitamin D, lowered UV radiation exposure, cigarette smoking, obesity, and EBV exposure. |
| B cells | B cells play a central role in MS. Like T cells, there are pro- and anti-inflammatory B cell subsets. In relapsing MS, B cells serve as primary antigen-presenting cells that drive pathogenic T cells. In progressive MS, B cells enhance the compartmentalized CNS responses through lymphoid follicles and secreted factors. |
| Microbiome | The microbiome regulates T cell function throughout the body and contains both pathogenic microbial components, which play an important role in MS by establishing immune set points and by secreting metabolites. |
| Relapsing MS | Relapsing MS is driven by immune cells that migrate into the CNS. Multiple treatments have been shown to effectively treat relapsing MS (decrease relapses and new MRI lesions) and act on the following common pathways: decrease the number and/or function of effector cells, increase the number and/or function of regulatory cells, and prevent trafficking of cells to the CNS. |
| Progressive MS | Progressive MS mechanisms include those that are immune-dependent and immune-independent. In immune-dependent forms, an innate immune response is established in the brain that involves microglia, macrophages, B cells, and lymphoid follicles. There may also be chronic activation of peripheral T cells and innate cells. In immune-independent forms, mitochondrial injury, oxidative stress, and ion imbalance occur. Current therapy does not effectively target these two processes. |
| Autoantigen | The inciting autoantigen in MS is unknown. However, when MS is diagnosed, there would be no single autoantigen to target as there is spreading of reactivity to other organ-specific antigens as occurs in type 1 diabetes. Thus, antigen-specific therapy would have to employ bystander suppression or be given as a preventative strategy in at-risk subjects. |
| Therapy | MS is a heterogeneous disease. There will be responders and non-responders to each “effective” therapy. The earlier in the disease course that treatment is initiated, the more likely it is to be effective. Effective treatment will require pulse or continuous therapy and, ultimately, combination therapy. The identification of immune and MRI biomarkers will be the cornerstone of immunotherapy of MS and the achievement of no evidence of disease activity (NEDA). |
Characteristics/Clinical Presentation[edit | edit source]
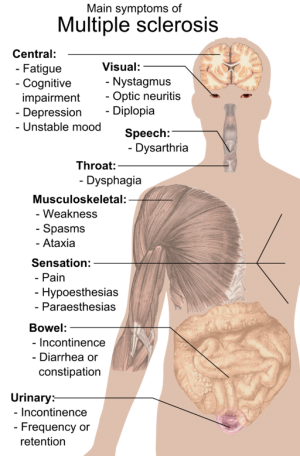
Multiple Sclerosis will present with varying symptoms depending upon the location of the nerves being affected[2]. Symptoms usually appear suddenly and rapidly over minutes or hours, but in more rare cases the symptoms may be insidious and take several weeks to months to develop[2].
Early symptoms:-[edit | edit source]
- Numbness and weakness in one or several limbs progressing from paresthesias,
- Visual disturbances such as double vision, atrophy of one optic nerve
- impaired ocular movement
- Fatigue is typically the early symptoms that will present with MS[2].
Other common symptoms:-[edit | edit source]
- Pain: Headache, chronic neuropathic pain, paroxysmal limb pain.
- Cognitive symptoms: Short-term memory deficits, diminished executive function, diminished attention/concentration.
- Affective Symptoms: Depression, anxiety.
- Motor symptoms: spasticity, spasms, ataxia, impaired balance and gait.
- Speech and swallowing: dysarthria, dysphonia, dysphagia.
- Bladder/Bowel symptoms: spastic or flaccid bladder, constipation, diarrhoea and incontinence.
- Sexual Symptoms: impotence, decreased libido, decreased ability to achieve orgasm[2].
The pattern of symptoms will be different from person to person. The initial symptoms are typically acute and followed by a period of remission with complete or partial recovery[11]. An increase in symptoms can occur with an increase in body temperature because many MS patients have a sensitivity to heat[11]. Multiple sclerosis can also cause lumbar radiculopathy.
The disease is the most common cause of neurological disability affecting people in their productive years, between 15 and 55 years of age. [12] It afflicts women more often than men (ratio of approximately 2:1).[13] Overall course and prognosis in multiple sclerosis are most likely to be related to age and the occurrence of the progressive phase of the disease, rather than to relapses or other clinical parameters. Individual prognosis remains hazardous.[14]
Associated Co-morbidities[edit | edit source]
Co-morbidities are common among the ageing population especially with added risk factors of a poor diet and obesity. They often lead to a decrease in functional status and quality of life. Knowing the prevalence and common types that exist in MS can help with disease management, to maximise an individual’s overall physical well-being. Common co-morbidities seen in patients with MS include [15]:
Autoimmune - Inflammatory bowel disease, Thyroid disease, Uveitis, Arthritis. Systemic lupus erythematosus
Physical - Hypertension, Hyperlipidemia, Heart disease, Chronic lung disease, Osteopenia/Osteoporosis
Behavioural - Anxiety. Depression. Sleep disorders. Alcohol use. Obesity
Less common co-morbid conditions - kidney disease, asthma, cancer, Sjogren’s syndrome, and liver disease.
Systemic Involvement[edit | edit source]
1. Nervous System - MS greatly impacts the CNS system when the body's immune cells attack the myelin, which exposes the nerve and creates a disconnect between the brain and the rest of the body. The disruption between the brain and the body creates a decrease in function throughout the body[16]. MS impacts the brain with symptoms such as memory loss, confusion, dizziness, vertigo, personality changes, depression and less commonly, seizures[16]
2. Visual System - Vision disturbances are a common first symptom with MS that comes on suddenly in one or both eyes[16]. Symptoms may present as blurred or double vision, pain, and trouble seeing the contrast in one or both eyes[16]. Vision impairments are due to inflammation and fatigue in the eye muscles and are temporary in most cases. Hearing loss is another effect of MS but less common to occur[16]. Problems with hearing usually occur due to damage to the brainstem and most commonly resolve on their own[16].
3. Respiratory System - The Decreased function of the respiratory muscles due to nerve damage can create speech as well as breathing difficulties. This complication usually occurs early on in the disease process and worsens as MS progresses[16].
4. Musculoskeletal System - Muscle weakness, numbness and tingling are common symptoms to occur because of demyelination in MS. This complication can lead to problems such as decreased hand-eye coordination, balance, gait, and fine motor skills because the brain has difficulty sending information to the nerves and muscles[16]. As the disease progresses these symptoms may worsen and make assistive devices necessary for gait and mobility. MS can also increase the risk of bone fractures and osteoporosis because of steroid use and inactivity, which decrease bone density[16]. Swallowing difficulties can also arise because of the muscles responsible for swallowing become weak due to nerve damage. Problems with swallowing can lead to food or liquid getting into the lungs and cause an infection[16].
5. Autonomic System - MS can affect the bladder when damage to the nerves that control bladder and sphincter function occurs[3]. The bladder can become “spastic” in which it is unable to empty urine properly or a “flaccid” bladder in which it is unable to hold urine[3]. Bowel problems are another complication that can occur in MS patients and will present as a loss of bowel control as well as constipation. Sexual impairments are a common occurrence in people with MS, which occurs when the nerves sending information to the sexual organs are damaged[3]. This damage can lead to problems in arousal and orgasm. Sexual impairments can also be caused by other MS symptoms, such as fatigue, spasticity and mood[3].
6. Integumentary System - MS patients are at a much greater risk of skin breakdown due to sensation loss, heat sensitivity, muscle weakness/paralysis and immobility[2].
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Multiple Sclerosis is diagnosed by a neurologist by performing a detailed medical history, and neurological exam as well as ordering supportive laboratory tests. The laboratory tests are used to diagnose as well as rule out other possible conditions that may present similarly[11].
- Magnetic Resonance Imaging
An MRI is very sensitive in detecting MS plaques that are found in the white matter of the brain and spinal cord[2]. The plaques that appear on the MRI may also be seen with conditions, such as Lupus, diabetes as well as migraines and therefore cannot be used to give definitive reasoning to rule in MS[11].
- Spinal Tap (Lumbar Puncture)
A spinal tap is a procedure in which a needle is inserted into the lumbar spine to remove a small amount of cerebral spinal fluid, which is then brought to a lab for analysis[11]. The cerebral spinal fluid is tested for an abnormal amount of white blood cells, proteins and other abnormalities that are secondary to MS.[11]
- Evoked Potential Test
The evoked potential test measures electrical signals in the nerves sent from the brain in response to a stimulus.[11] The stimulus may be visual or electrical in origin[11]. This test helps detect whether there is a lesion to a nerve in the optic nerve, brainstem and spinal cord even though a person may not be presenting with any neurological signs of nerve damage[11].
A blood test is beneficial to perform to rule out other conditions that may present similar to MS, such as infectious or inflammatory diseases[11].
Differential Diagnosis[edit | edit source]
Diagnosis of MS can be a complicated task. An easy mnemonic to aid in differential diagnosis used by the National Multiple Sclerosis Society is VITAMINS:[3]
- Vascular: Multiple lacunar infarcts; CADASIL; spinal arteriovenous malformation
- Infectious: Lyme disease; syphilis; HIV myelopathy; PML; HTLV-1 myelopathy
- Traumatic: Spondylitis myelopathy
- Autoimmune: NMO; acute disseminated encephalomyelitis; CNS vasculitis; Behcet syndrome, sarcoidosis; SLE
- Metabolic/Toxic: Central pontine myelinolysis; vitamin B12 deficiency; vitamin B6 deficiency; radiation; hypoxia
- Idiopathic/Genetic: Spinocerebellar degeneration; Friedreich ataxia; Arnold-Chiari malformation; adrenoleukodystrophy; metachromatic dystrophy
- Neoplastic: CNS lymphoma; glioma; paraneoplastic encephalomyelitis; metastatic cord compression
- pSychiatric: Conversion disorder.
Physical Therapy Management[edit | edit source]
Physical therapy - plays an essential role in keeping a patient with MS active and functional within the community
Aims of Physiotherapy
- To re-educate and maintain all available voluntary control
- Re-educate & maintain postural mechanisms
- Incorporate treatment techniques into ways of life by relating to ADLs
Inhibit abnormal tone
- Prevent abnormal movement
- To stimulate all sensory and perceptual experience
The PT assessment - focuses on posture, movement, and function, realise the patient's performance may be limited by fatigue, pain or other factors. An individualized program can then be set up. This program must easily be performed at home, and provide written instructions. Education is important to assist patients in managing their programs as independently as possible. Multidisciplinary treatment for MS patients leads to positive effects.
Expanded disability scale to evaluate degree of disability.
Multiple Sclerosis Functional Composite to assess 3 functional domains; ambulatory, hand and cognitive function.
Physiotherapy treatment[edit | edit source]
- Exercise is essential. A narrative [17]review highlights that exercises are safe and effective in symptom management and disease modification. The authors encourage neurologists, as they are critical in the treatment process along with the multidisciplinary healthcare team to prescribe and promote exercises at the diagnosis and across all stages of the disease trajectory using prescriptive clinical exercise guidelines as part of comprehensive MS care. Clinical education to dispel historical myths related to exercise in MS and behaviour change theory help overcome patients' barriers to exercise[17]. Exercise is beneficial at multiple levels and has an important role in delaying negative symptoms of the disease. Choose exercises appropriate to the client's strengths and weaknesses [18]. State the best ’dose’ (intensity, frequency and duration) of treatment in terms of activities and participation. Exercise is considered as a safe effective means of rehabilitation[19]. Exercise also has benefits on mood and quality of life. The use of therapeutic corticosteroids and inactivity due to fatigue and weakness may lead to osteoporosis and pathological fractures. Weight-bearing exercises are hence beneficial.
- Strength and aerobic training:
- The resistance training program is recommended for maintaining bone and muscle mass.
- Other techniques e.g. Bobath, Vojtas, Proprioceptive Neuromuscular Techniques; carried out regularly and with sufficient intensity, have evidence of improvement in patients with MS [20] Exercise improves impairments of aerobic capacity[21], lower extremity muscle strength[22], fatigue, and depression[23]; reduced activity limitations such as walking performance and balance; and confirms that it positively impacts quality of life.[24]
- According to Döring et al., aerobic training seems to have a positive effect on fatigue[25]. The physical activity guidelines for MS people state that those with mild to moderate disability need at least 30 minutes of moderate-intensity aerobic activity (2 times per week) and strength training' exercises for major muscle groups (2 times per week). [22][26]There is sufficient evidence that these exercises may reduce fatigue, improve mobility, and enhance health-related quality of life, and people with MS and health professionals are encouraged to adopt these rigorously developed guidelines[26]. Aerobic exercise training with low to moderate intensity can result in the improvement of aerobic fitness and reduction of fatigue in MS patients, affected with mild or moderate disability [27]
- According to the rapid review and synthesis by Yumi Kim et.al, the recommended exercise guidelines for MS: aerobic training 2–3 days/week (10–30 minutes at moderate intensity) and resistance training 2–3 days/week of (1–3 sets of 8–15 repetition maximum (RM)). However, further research is needed to examine the benefits and training adaptation with combined or isolated aerobic and strength training.[28]
- Aquatic exercise programs have a positive effect on persons with progressive multiple sclerosis. It promotes general health, improves energy levels and mental health, and aids social interaction in the presence of physical disability [29]. Because of the reduced impact of gravity, aquatic training allows patients with even severe paresis of the lower extremities to perform standing and moving exercises. A systematic review and Meta-Analysis recommends combining aquatic therapy with conventional physical therapy for MS patients[30].
- Specific balance exercises can improve balance. Poor postural control increases the risk of falls. MS patients have increased sway in quiet stance, delayed postural perturbations and reduced ability to move towards limits of stability. These impairments are likely causes of falls. Reduced gait speed, decreased stride length, cadence, and joint movement are observed in most studies of gait in MS [31].
- Hippotherapy has a positive effect on the balance of persons with multiple sclerosis and improves the quality of life [32]. A systematic review and meta-analysis of the therapeutic effect of Horseback riding intervention show positive physical and emotional effects of horse riding in individuals with neuromotor development and physical disabilities [33]. Horseback riding improved balance and gait of ambulatory patients with MS [34] and helps the rider, by providing effective sensory stimulation and rhythmic anterior and posterior swinging motion. It also improves posture and balance [35].
- Motor Imagery is increasingly used in neuro-rehabilitation to facilitate motor performance. Motor imagery and rhythmic auditory stimulation can be used for walking rehabilitation in MS patients [36]. Randomized controlled trial studying the effects of motor imagery showed significant improvement in walking speed, walking distance, perception and quality of living [37]
- Cognitive Behavioral Therapy (CBT) ] has a moderately positive effect on fatigue in MS. However, this effect declines after cessation of treatment. To have good results, the patient should be referred to a CBT specialist [38][39]. CBT can also be an effective intervention for reducing moderate depression, over a short term, in MS patients, which may also improve patient quality of life[40].
- Gait rehabilitation forms a large part of neuro-rehabilitation for people living with MS. A systematic review published in Diagnostics describing the gait pattern in people with multiple sclerosis (MS) shows a decrease in speed stride and step length, increase in the step width, decrease in hip extension during the stance period, a reduction in knee flexion in the swing period, a decrease in ankle dorsiflexion in the initial contact and a decrease in ankle plantarflexion during the pre-swing phase; thus concluding that rehabilitation should focus on combating asymmetrical gait characteristics.[41]
Aims in the progression of MS[edit | edit source]
- During the early stages of MS (patients may present with minimal impairments) - focus on educating the patient and family members or caregivers on disease progression and compensatory strategies to conserve energy [2], [42]. Emphasize movement outdoors, especially in sunlight (direct benefits of sunlight in MS). Research suggests lifetime sun exposure appears to reduce the risk of Multiple Sclerosis regardless of race/ethnicity and indicates the protective effect of sun exposure in MS is most likely mediated through immunomodulatory mechanisms [43]
- In the moderate stage might notice impairments at varying degrees and activities of daily living (ADL) may require assistance. Therapy should focus more on improving or maintaining motor functions through strength, endurance, flexibility, balance, respiratory training and assistive device training as well as suggesting environment modifications to the home or assessing mobility aids required to move about in the community to sustain the quality of life [2], [42]. Education about correct postures is important to prevent further complications. A close collaboration between professional community carers and non-professional caregivers at home is a key factor for successful home rehabilitation [44].
- Advanced stages of MS often present with multiple impairments at increasing severity compared to earlier stages. The primary goals of the PT in late stages are to maximize independence through postural and ADL training, respiratory function, safety and prevention strategies for contracture development or pressure wounds, equipment suggestions, and proper transfer techniques [2][42] [6]
Throughout all stages of MS, PT can offer psychological support to the patient and family/caregiver [2]
General preventive measures
Here are certain problems seen in most patients with disability which are possible to anticipate and prevent
- Plantar flexed feet
- Predominant pattern of extension and adduction in lower extremities
- Knee flexion contracture
- Hip flexion Contracture
- Flexed thoracic spine
- Flexion and internal rotation at the shoulders
- Flexed head positions
PT Interventions for Common Symptoms of Patients with MS
In the 3-minute video below a PT advises on the PPMS treatment approach,
- Pain. Patients with MS often experience pain directly from the disease, secondary to medication or other symptoms, or from something completely separate. PT helps relieve pain through exercise, stretching, massage, ultrasound, postural training, or hydrotherapy.[2]
- Sensory Deficits. Tapping and verbal cues during exercise and resistance training can help improve proprioception losses. Vision issues, such as blurred or double vision, often occur in patients with MS. PT can offer education on how to be safe at home and offer strategies to improve balance and coordination in dimly lit settings. PT treatment interventions for decreased sensation to light touch include education on awareness, protection, and personal care for desensitized body parts. Pressure-relieving devices are a primary prevention strategy along with proper transfer techniques and daily skin inspections for maintaining skin integrity.[2]
- Fatigue. One of the most debilitating symptoms of MS is experienced by an overwhelming majority of patients: fatigue. PT strategies to help patients combat feelings of excessive tiredness include aerobic exercise, energy conservation, and activity pacing. Aerobic exercise activities are closely monitored by a PT to ensure a patient does not overheat but can work on increasing their endurance capacity which will help them be more functional throughout the day. PTs can also teach energy conservation strategies and activity pacing to help someone sustain their daily activities by minimizing fatigue.[2]
- Spasticity. The physical and functional limitations spasticity leads to include a variety of impairments which can present as contractures, postural deformities, decubitus ulcers, and more. PT interventions range from cryotherapy and hydrotherapy to therapeutic exercise, stretching, range of motion activities, postural training, and electrical stimulation. A combination of therapeutic interventions is often the route taken.[2]
- Balance, Coordination, & Postural Deficits. Ataxia, postural instability, muscle spasms, and generalized muscle weakness all contribute to balance and coordination deficits. PT techniques to address these issues include postural exercise, core strengthening, rhythmic stabilization, static/dynamic balance training, aquatic therapy, proprioceptive loading, and resistance training.[2]
- Mobility Issues. Weakness, particularly in the lower extremity, balance deficits, fatigue, posture, contractures, sensation deficits, heat intolerance, among other deficits, can impede an individual's ability to be mobile. In combination with the treatment previously described, PTs work to help patients overcome their mobility limitations through locomotor and functional training. Locomotor training focuses on increasing thigh and hip strength along with posture and balance training through walking activities. Orthotics and assistive devices are added as necessary. Functional training involves bed mobility, transfers, and developing strategies with the patient on how to be able to safely navigate around the home and out in the community.[2]
Team Work[edit | edit source]
A study carrying out an online cross-sectional survey of physical therapists specialized in multiple sclerosis across Europe concluded that the content and delivery of physical therapy in Multiple Sclerosis differs across Europe and the guidance concerning access to treatment and adjustment according to disability do not appear to be widely implemented in clinical practice[46]. Also. a recent online cross-sectional survey taken by Physical therapists specialized in Multiple Sclerosis, to study the real-world use of goal setting and outcome measures in Europe showed discrepancies in goal setting and assessment across European regions[47].
Multiple sclerosis is a complex disease. In addition to sensory changes, weakness, and visual changes, coordination problems or spasticity can be seen. Other complaints related to general health include bladder and bowel dysfunction, cognitive impairment, depression, fatigue, sexual dysfunction, sleep problems, and vertigo. Because of the shortened life expectancy and multisystem involvement, the disorder is best managed by an interprofessional team that includes a neurologist, physical therapist, pain specialist, nurse specialist, ophthalmologist, mental health nurse, gastroenterologist and a urologist. Because there is no cure, it is vital to ensure that the patient's quality of life is not eroded. Social workers must be involved early in the care and the patient provided with all the possible supportive assistance.[1]
Dietary Modification[edit | edit source]
Some preliminary research investigating inflammation-reducing diet which could help control chronic inflammation.[48][49] Many researchers are exploring dietary intervention approaches in MS to improve lifestyle[49].
- Probiotics[50] may improve the health of people with MS by reducing disability and improving inflammatory and metabolic parameters[51]according to an Iranian study.
- Vitamin D supplementation may assist in the prevention and treatment of MS however existing evidence is of very low quality.[52] Various research studies are studying the effectiveness of vitamin D therapy in MS. [53]
- Fish oil supplementation given together with vitamins and dietary advice can improve clinical outcome in patients with newly diagnosed MS.[54]More research is required to assess the effectiveness of dietary interventions of omega 3 in MS and its interaction with medications used for treating MS.[55][56] Dysfunction of mitochondria is thought to play an important role in the mechanism of progression of demyelinating disorders.[57]Observations in animal and histopathological studies suggest that dysfunctional mitochondria are important contributors to damage and loss of both axons and neurons.[58] The relationship between mitochondrial dysfunction and neurodegeneration in MS is explored.
- Ketogenic diet has the potential to treat the neurodegenerative component of progressive MS, though more research is required in this field.[59][49]
Medical Management[edit | edit source]
Acute Relapse Management[edit | edit source]
Management works as immunosuppressants and anti-inflammatory drugs to reduce CNS swelling. There are numerous medications available to assist acute attacks, and disease progression, and to help manage symptoms [3].
- Prednisone: Typically, a high dose of a corticosteroid, such as - methylprednisolone is the first line of treatment against an attack of MS[60][11]. Corticosteroids help to reduce inflammation by suppressing the immune system, and when given intravenously can work quickly [60]. Oral doses are often given as follow-up treatments during acute exacerbations [60]. Side effects include sleep disturbance, headache, excessive sweating, or increased hair growth[3]. Prolonged corticosteroid use can also lead to skin problems, oedema of the face or lower extremities, arthralgias, irregular menstruation, muscle cramps, and pain[3]. Brand Name: Deltasone[3]
- Plasmapheresis: As a supplemental or secondary treatment, plasmapheresis (plasma exchange) can be used in relapsing forms of MS to help control MS attacks [60]. During the plasmapheresis procedure, potentially harmful components of plasma are separated and removed from the blood, then replacement plasma and blood cells are returned to the body [60] This method is thought to be useful as a secondary treatment option for severe relapsing forms of MS but is not recommended for PPMS or SPMS[3].
Disease-Modifying Agents[edit | edit source]
work to slow progress or reduce the number of MS attacks: They are most commonly used for decreasing relapses in patients with RRMS [60]. Before initiating disease-modifying treatment, a complete diagnostic workup is crucial to help begin treatment at the appropriate time. Early intervention using disease-modifying drugs is most effective however the risks involved in prematurely starting treatment for MS if this is not the true diagnosis can cause an individual to become susceptible to the serious side effects of taking some of these drugs [60]. The following disease-modifying drugs work to slow progress or reduce the number of MS attacks.
- Beta Interferons
- Glatiramer acetate - Injectable disease-modifying drugs that may help alter immune cells from attacking myelin[11].
- Mitoxantrone - an injectable drug given four times per year that suppresses immune functions thought to attack myelin[60]. This drug is approved for treating SPMS, PRMS, and RRMS[3]. Brand Name: Novantrone[3]
- Natalizumab
- Fingolimod
Symptom Management[edit | edit source]
It is an integral component of helping patients with MS function in their daily lives. Numerous pharmacological agents can be used to relieve common symptoms of MS. e.g. Spasticity, Pain, Fatigue, Tremor, Cognitive & Emotional Impairments, and Bowel & Bladder Impairments.
For more information and drug listings on symptom management, please visit the following link: Medications.
Resources[edit | edit source]
National Multiple Sclerosis Society
Multiple Sclerosis Association of America
References[edit | edit source]
- ↑ 1.0 1.1 1.2 William Gossman; Moavia Ehsan; Kathryn L. Xixis. Multiple Sclerosis Last Update: July 12, 2019. Available from:https://www.ncbi.nlm.nih.gov/books/NBK499849/ (last accessed 4.1.2020)
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 O'Sullivan S, Schmitz T, Fulk G: Physical Rehabilitation. 6th edition. Philadelphia, PA. F.A. Davis Company; 2014.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 National Multiple Sclerosis Society. Incidence and Prevalence of MS. http://www.nationalmssociety.org/What-is-MS/Who-Gets-MS. (Accessed: 21 March 2014)
- ↑ https://www.nationalmssociety.org/What-is-MS/Definition-of-MS/Immune-mediated-disease
- ↑ Owens GP, Gilden D, Burgoon MP, Yu X, Bennett JL. Viruses and multiple sclerosis.https://www.ncbi.nlm.nih.gov/pubmed/22130640 The Neuroscientist. 2011 Dec;17(6):659-76.
- ↑ 6.0 6.1 Tselis A. Epstein–Barr virus cause of multiple sclerosis. https://www.ncbi.nlm.nih.gov/pubmed/22617821Current opinion in rheumatology. 2012 Jul 1;24(4):424-8.
- ↑ Fernández-Menéndez S, Fernández-Morán M, Fernández-Vega I, Pérez-Álvarez A, Villafani-Echazú J. Epstein–Barr virus and multiple sclerosis. From evidence to therapeutic strategies. https://www.ncbi.nlm.nih.gov/pubmed/26810546Journal of the neurological sciences. 2016 Feb 15;361:213-9.
- ↑ Chen J, Chia N, Kalari KR, Yao JZ, Novotna M, Soldan MM, Luckey DH, Marietta EV, Jeraldo PR, Chen X, Weinshenker BG.https://www.nature.com/articles/srep28484 Multiple sclerosis patients have a distinct gut microbiota compared to healthy controls. Scientific reports. 2016 Jun 27;6:28484.
- ↑ Shahi SK, Freedman SN, Mangalam AK. Gut microbiome in multiple sclerosis: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5730390/The players involved and the roles they play. Gut microbes. 2017 Aug 2;6:1-9.
- ↑ Baecher-Allan C, Kaskow BJ, Weiner HL. Multiple Sclerosis: Mechanisms and Immunotherapy. Neuron. 2018 Feb 21;97(4):742-68.https://www.ncbi.nlm.nih.gov/pubmed/29470968
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269Disease and Conditions Multiple Sclerosis
- ↑ European-wide recommendations on rehabilitation for people affected by multiple sclerosis; EMSP and R.I.MS; October 2004
- ↑ Sean Horton, Dany J. MacDonald, Karl Erickson; MS, exercise, and the potential for older adults.fckLREur Rev Aging Phys Act. 2010; 7:49–57
- ↑ Sandra Vukusica and Christian Confavreux.; Natural history of multiple sclerosis: risk factors and prognostic indicators.; Current Opinion in Neurology. 2007; 20:269–274
- ↑ Miller, A. Multiple Sclerosis—Part 2. American Academy of Neurology 2013; 2. http://www.audio-digest.org/adfwebcasts/pdfs/ca0214.pdf (accessed 21 March 2014).
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 16.7 16.8 16.9 Health Line. Multiple Sclerosis From Top to Bottom.http://www.healthline.com/health/multiple-sclerosis/effects-on-the-body. (Accessed: 23 March 2014)
- ↑ 17.0 17.1 Learmonth YC, Motl RW. Exercise Training for Multiple Sclerosis: A Narrative Review of History, Benefits, Safety, Guidelines, and Promotion. International Journal of Environmental Research and Public Health. 2021 Jan;18(24):13245.
- ↑ Horton S, MacDonald DJ, Erickson K. MS, exercise, and the potential for older adults. European Review of Aging and Physical Activity. 2010 Apr;7(1):49-57.
- ↑ Halabchi F, Alizadeh Z, Sahraian MA, Abolhasani M. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations.https://www.ncbi.nlm.nih.gov/pubmed/28915856 BMC neurology. 2017 Dec;17(1):185.
- ↑ Döring A, Pfueller CF, Paul F, Dörr J. Exercise in multiple sclerosis--an integral component of disease management.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3375103/ EPMA Journal. 2012 Dec 1;3(1):2.
- ↑ Langeskov-Christensen M, Heine M, Kwakkel G, Dalgas U. Aerobic capacity in persons with multiple sclerosis: a systematic review and meta-analysis. Sports Med. 2015;45(6):905-923.
- ↑ 22.0 22.1 Latimer-Cheung AE, Martin Ginis KA, Hicks AL, et al. Development of evidence-informed physical activity guidelines for adults with multiple sclerosis. Arch Phys Med Rehabil. 2013;94(9):1829-1836.e7.
- ↑ Ensari I, Motl RW, Pilutti LA. Exercise training improves depressive symptoms in people with multiple sclerosis: results of a meta-analysis. J Psychosom Res. 2014;76(6):465-471. doi:10.1016/j.jpsychores.2014.03.014.
- ↑ Kuspinar A, RodriguezAM, Mayo NE. The effects of clinical interventions on health-related quality of life in multiple sclerosis: a meta-analysis. MultScler. 2012;18(12):1686-1704.
- ↑ Döring et al. Exercise in multiple sclerosis – an integral component of disease management. EPMA Journal. 2012 Dec 1;3(1):2.
- ↑ 26.0 26.1 Latimer-Cheung AE, Pilutti LA, Hicks AL, Ginis KA, Fenuta AM, MacKibbon KA, Motl RW. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Archives of physical medicine and rehabilitation. 2013 Sep 1;94(9):1800-28.
- ↑ Halabchi F, Alizadeh Z, Sahraian MA, Abolhasani M. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC neurology. 2017 Dec;17(1):185.
- ↑ Kim Y, Lai B, Mehta T, Thirumalai M, Padalabalanarayanan S, Rimmer JH, Motl RW. Exercise training guidelines for multiple sclerosis, stroke, and Parkinson’s disease: Rapid review and synthesis. American journal of physical medicine & rehabilitation. 2019 Jul;98(7):613.
- ↑ G. Roehrs, Gregory M. Karst; Effects of an Aquatics Exercise Program on Quality of Life Measures for Individuals with Progressive Multiple Sclerosis; Journal of Neurological Physical Therapy. 2004; 28, 63-71
- ↑ Amedoro A, Berardi A, Conte A, Pelosin E, Valente D, Maggi G, Tofani M, Galeoto G. The effect of aquatic physical therapy on patients with multiple sclerosis: A systematic review and meta-analysis. Multiple Sclerosis and Related Disorders. 2020 Feb 22:102022.
- ↑ Cameron MH, Lord S. Postural control in multiple sclerosis: implications for fall prevention.https://www.ncbi.nlm.nih.gov/pubmed/20567946/ Current neurology and neuroscience reports. 2010 Sep 1;10(5):407-12.
- ↑ C. Bronson, K. Brewerton, J. Ong.; Does hippotherapy improve balance in persons with multiple sclerosis: a systematic review.; Eur J Phys Rehabil Med. 2010 ; 46(3):347–53
- ↑ Stergiou A, Tzoufi M, Ntzani E, Varvarousis D, Beris A, Ploumis A. Therapeutic Effects of Horseback Riding Interventions: https://www.ncbi.nlm.nih.gov/pubmed/28252520A Systematic Review and Meta-analysis. American journal of physical medicine & rehabilitation. 2017 Oct 1;96(10):717-25.
- ↑ Muñoz-Lasa S, Ferriero G, Valero R, Gomez-Muñiz F, Rabini A, Varela E.https://www.ncbi.nlm.nih.gov/pubmed/22452106 Effect of therapeutic horseback riding on balance and gait of people with multiple sclerosis. G Ital Med Lav Ergon. 2011 Oct;33(4):462-7.
- ↑ Koca TT, Ataseven H. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5175116/What is hippotherapy? The indications and effectiveness of hippotherapy. Northern clinics of Istanbul. 2015;2(3):247.
- ↑ Seebacher B, Kuisma R, Glynn A, Berger T. The effect of rhythmic-cued motor imagery on walking, fatigue and quality of life in people with multiple sclerosis:https://www.ncbi.nlm.nih.gov/pubmed/27055804 A randomised controlled trial. Multiple Sclerosis Journal. 2017 Feb;23(2):286-96.
- ↑ Seebacher B, Kuisma R, Glynn A, Berger T. Exploring cued and non-cued motor imagery interventions in people with multiple sclerosis:https://www.ncbi.nlm.nih.gov/pubmed/29507773 a randomised feasibility trial and reliability study. Archives of physiotherapy. 2018 Dec;8(1):6.
- ↑ Van den Akker LE et al. Effectiveness of cognitive behavioural therapy for the treatment of fatigue in patients with multiple sclerosis: A systematic review and meta-analysis. J Psychosom Res. 2016;90:33-42
- ↑ Nazarboland N et al. Effectiveness of Cognitive Behavioral Therapy for Multiple Sclerosis (MS) Fatigue. Int J Behav Sci. 2017; 11(1): 19-24
- ↑ Hind et al. Cognitive behavioural therapy for the treatment of depression in people with multiple sclerosis: a systematic review and meta-analysis. BMC Psychiatry. 2014;14:5
- ↑ Coca-Tapia M, Cuesta-Gómez A, Molina-Rueda F, Carratalá-Tejada M. Gait Pattern in People with Multiple Sclerosis: A Systematic Review. Diagnostics. 2021 Apr;11(4):584.
- ↑ 42.0 42.1 42.2 Provance, P. Physical Therapy in Multiple Sclerosis Rehabilitation. New York: A Clinical Bulletin from the Professional Resource Center of the National Multiple Sclerosis Society, 2011. http://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical-Bulletin-Physical-Therapy-in-Multiple-Sclerosis-Rehabilitation.pdf (accessed 23 March 2014)
- ↑ Langer-Gould A, Lucas R, Xiang AH, Chen LH, Wu J, Gonzalez E, Haraszti S, Smith JB, Quach H, Barcellos LF.[1] MS Sunshine Study: Sun Exposure But Not Vitamin D Is Associated with Multiple Sclerosis Risk in Blacks and Hispanics. Nutrients. 2018 Feb 27;10(3):268.
- ↑ European-wide recommendations on rehabilitation for people affected by multiple sclerosis; EMSP and R.I.MS; October 2004
- ↑ NationalMSSociety Physical Therapist (SK) PPMS Care Team - National MS Society. Available from: https://www.youtube.com/watch?time_continue=6&v=dd1wfNBKk_Y
- ↑ Bethoux F, Marrie RA. A cross-sectional study of the impact of spasticity on daily activities in multiple sclerosis. The Patient-Patient-Centered Outcomes Research. 2016 Dec 1;9(6):537-46.
- ↑ Řasová K, Martinková P, Soler B, Freeman J, Cattaneo D, Jonsdottir J, Smedal T, Romberg A, Henze T, Santoyo-Medina C, Feys P. Real-world goal setting and use of outcome measures according to the international classification of functioning, disability and health: A European survey of physical therapy practice in multiple sclerosis. International journal of environmental research and public health. 2020 Jan;17(13):4774.
- ↑ https://www.amymyersmd.com/2018/02/7-foods-fight-inflammation/
- ↑ 49.0 49.1 49.2 https://www.nationalmssociety.org/NationalMSSociety/media/Mid-America/Stay%20Informed/MS-Connection-Summer16.pdf
- ↑ https://multiplesclerosisnewstoday.com/2017/09/15/ms-patients-who-take-probiotics-ma-improve-certain-disease-parameters-study-suggests/
- ↑ Kouchaki E, Tamtaji OR, Salami M, Bahmani F, Kakhaki RD, Akbari E, Tajabadi-Ebrahimi M, Jafari P, Asemi Z. https://www.ncbi.nlm.nih.gov/pubmed/27669638Clinical and metabolic response to probiotic supplementation in patients with multiple sclerosis: a randomized, double-blind, placebo-controlled trial. Clinical Nutrition. 2017 Oct 1;36(5):1245-9.
- ↑ Brown SJ. The role of vitamin D in multiple sclerosis. Annals of Pharmacotherapy.https://www.ncbi.nlm.nih.gov/pubmed/16684809 2006 Jun;40(6):1158-61.
- ↑ https://www.nationalmssociety.org/Research/Research-News-Progress/Vitamin-D
- ↑ Nordvik I, Myhr KM, Nyland H, Bjerve KS. Effect of dietary advice and n‐3 supplementation in newly diagnosed MS patientshttps://www.ncbi.nlm.nih.gov/pubmed/10987373. Acta Neurologica Scandinavica. 2000 Sep 1;102(3):143-9.
- ↑ https://www.nationalmssociety.org/About-the-Society/News/Dietary-Omega-3-Fatty-Acids-Linked-to-Lower-Risk-o
- ↑ https://www.nationalmssociety.org/Living-Well-With-MS/Diet-Exercise-Healthy-Behaviors/Diet-Nutrition/Omega-3
- ↑ Carvalho KS. Mitochondrial dysfunction in demyelinating diseases.https://www.ncbi.nlm.nih.gov/pubmed/24331361 InSeminars in pediatric neurology 2013 Sep 1 (Vol. 20, No. 3, pp. 194-201). Elsevier.
- ↑ Witte ME, Mahad DJ, Lassmann H, van Horssen J. Mitochondrial dysfunction contributes to neurodegeneration in multiple sclerosis.https://www.ncbi.nlm.nih.gov/pubmed/24369898 Trends in molecular medicine. 2014 Mar 1;20(3):179-87.
- ↑ Storoni M, Plant GT. The therapeutic potential of the ketogenic diet in treating progressive multiple sclerosis.Storoni M, Plant GT. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709725/ Multiple sclerosis international. 2015;2015.
- ↑ 60.0 60.1 60.2 60.3 60.4 60.5 60.6 60.7 National Institute of Neurological Disorders and Stroke. Multiple Sclerosishttps://www.ninds.nih.gov/Disorders/All-Disorders/Multiple-Sclerosis-Information-Page#disorders-r1