Inflammation Acute and Chronic
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Bruno Serra, Rishika Babburu, Temitope Olowoyeye, Kim Jackson, Vidya Acharya and Sehriban Ozmen
Introduction[edit | edit source]
Inflammation has a major impact on our health and quality of life. It is the trigger behind many chronic diseases and a growing burden affecting health care across the globe. What do we know about it?
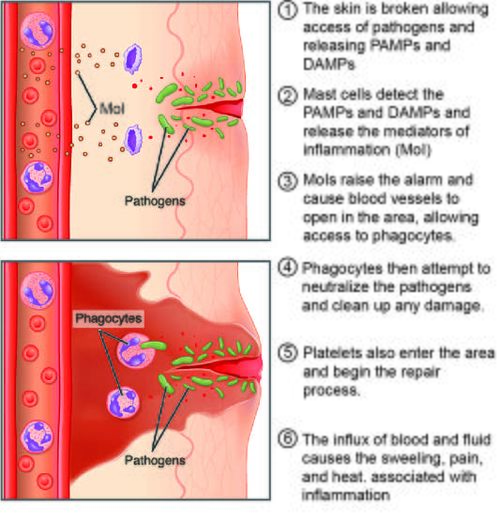
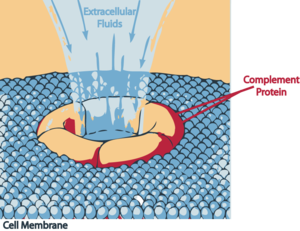
Inflammation is the immune system's response to harmful stimuli eg. pathogens, damaged cells, toxic compounds, or irradiation, and acts by removing injurious stimuli and initiating the healing process.
- Inflammation is a defense mechanism that is vital to health. During acute inflammatory responses, cellular and molecular events and interactions efficiently minimize impending injury or infection. This process contributes to restoration of tissue homeostasis and resolution of the acute inflammation.
- Uncontrolled acute inflammation may become chronic, contributing to a variety of chronic inflammatory diseases[1]. Inflammation can be hence be either acute or chronic.
- Acute Inflammation - Tissue damage due to trauma, microbial invasion, or noxious compounds can induce acute inflammation. It starts rapidly, becomes severe in a short time and symptoms may last for a few days eg. cellulitis; acute pneumonia. Subacute inflammation is the period between acute and chronic inflammation and may last 2 to 6 weeks.
- Chronic Inflammation - Chronic inflammation is also referred to as slow, long-term inflammation lasting for prolonged periods of several months to years. Generally, the extent and effects of chronic inflammation vary with the cause of the injury and the ability of the body to repair and overcome the damage[2].
Process and Resolution of Inflammation[edit | edit source]
In chronic inflammation, most of the features of acute inflammation continue, e.g., the expansion of blood vessels (vasodilation), increase in blood flow, capillary permeability, and migration of neutrophils into the infected tissue through the capillary wall (diapedesis). However, the composition of the white blood cells changes soon, and macrophages and lymphocytes begin to replace short-lived neutrophils. The hallmarks of chronic inflammation are the infiltration of primary inflammatory cells such as macrophages, lymphocytes, and plasma cells in the tissue site, producing inflammatory cytokines, growth factor and enzymes. This all contributes to the progression of tissue damage and secondary repair i,ncluding fibrosis and granuloma formation. [2]
- To prevent progression from acute inflammation to persistent chronic inflammation, the inflammatory response must be suppressed to prevent additional tissue damage. Inflammation resolution is a well-managed process involving the controlled production of mediators, during which chemokine gradients are diluted over time. Circulating white blood cells eventually no longer sense these gradients and are not recruited to sites of injury.
- Dysregulation of this process can lead to uncontrolled chronic inflammation. Inflammation resolution processes that rectify tissue homeostasis include reduction or cessation of tissue infiltration by neutrophils and apoptosis of spent neutrophils, counter-regulation of chemokines and cytokines, macrophage transformation from classically to alternatively activated cells, and initiation of healing.[1]
Causes[edit | edit source]
Chronic inflammation is not obvious, is often insidious, and often begins without an apparent cause. Our modern society is replete with inflammation triggers. These can be found in cigarette smoke; pollutants in our air, water, or food; our gut microbiomes; and mental cues, such as stress. As a result of our environment and lifestyles, we now live constantly with low levels of inflammatory signals “arming” our immune systems. This is a silent menace, not causing the usual overt signs of inflammation, but nevertheless complicating other disease processes that may be present[3]. Examples of when Chronic inflammation can develop below:
- Exposure: Sometimes, long-term, low-level exposure to an irritant, eg an industrial chemical, smoke, air pollution, causes chronic inflammation.
- Sensitivity: Inflammation happens when the body senses something that should not be there. Hypersensitivity to an external trigger can result in an allergy.
- Autoimmune disorders: The immune system mistakenly attacks normal healthy tissue, as in psoriasis.
- Autoinflammatory diseases: A genetic factor affects the way the immune system works, as in Behçet’s disease.
- Persistent acute inflammation: In some cases, a person may not fully recover from acute inflammation. Sometimes, this can lead to chronic inflammation.
Factors that may increase the risk of chronic inflammation include:
- older age
- obesity
- a diet that is rich in unhealthful fats and added sugar
- smoking
- low sex hormones
- stress
- sleep[2]
Damage[edit | edit source]
Scientists think chronic inflammation causes oxidative stress in the body, which is an imbalance between the production of dangerous free radicals, molecules that harm healthy tissue in the body, and antioxidants, substances that clean up waste products and neutralize them. This can damage DNA as well as proteins and fatty tissue, which in turn accelerates biological aging.
Chronic inflammation is involved in not just a few select disorders but a wide variety of very serious physical and mental health conditions. Indeed, chronic inflammatory diseases are the most significant cause of death in the world today, with more than 50 percent of all deaths being attributable to inflammation-related diseases.[4]
Chronic Inflammatory Complications[edit | edit source]
It is important to note that chronic inflammation is not a specific disease but a mechanistic process. Chronic inflammation progresses silently. It is the cause of most chronic diseases and presents a major threat to the health and longevity of individuals. The diseases associated with chronic inflammation are multiple.
- Cardiovascular diseases: Many clinical studies have shown strong and consistent relationships between markers of inflammation and cardiovascular disease. Atherosclerosis is a pro-inflammatory state with all the features of chronic low-grade inflammation and leads to an increase in cardiovascular events eg.g.,myocardial infarction, andstroke.
- Cancer: Chronic low-level inflammation also appears to participate in many types of cancer such as kidney, prostate, ovarian, hepatocellular, pancreatic, colorectal, lung, and mesothelioma.
- Diabetes: Immune cells like macrophages infiltrate pancreatic tissues, releasing pro-inflammatory molecules in diabetic individuals. Both circulating and cellular biomarkers underscore that diabetes is a chronic inflammatory disease. Chronic complications linked to diabetes include both microvascular and macrovascular complications. Diabetes not only increases the risk of macrovascular complications like strokes and heart attacks but also microvascular complications like diabetic retinopathy, neuropathy, and nephropathy.
- Rheumatoid arthritis
- IBD: a group of chronic inflammatory disorders of the digestive tract. It can develop as ulcerative colitis, causing long-lasting inflammation and ulcers in the lining of the large intestine and rectum, or Crohn's disease, characterised by inflammation of the lining of the digestive tract dispersing into affected tissues such as the mouth, oesophagus, stomach, and the anus.
- Chronic kidney disease: Low-grade inflammation is a common feature of chronic kidney disease. It can lead to the retention of several pro-inflammatory molecules in the blood and contributes to the progression of CKD and mortality.
- Allergic asthma
- COPD
- Alzheimer’s: In older adults, chronic low-level inflammation is linked to cognitive decline and dementia.[2]
- Metabolic Syndrome
- Multiple Autoimmune Syndrome
Ways of Reducing Inflammation[edit | edit source]
Inflammation can be reduced through: Medical interventions, natural approaches and lifestyle changes.
Medical intervention - There are various drugs that are routinely used to reduce inflammation in both acute and chronic illnesses. These drugs act by targeting several inflammatory pathways and can be administered based on the condition and its severity. The following are some of the most regularly used anti-inflammatory medicine classes:
- NSAIDs, like Ibuprofen, Naproxen, Aspirin, Diclofenac, and Celecoxib, reduce pain and inflammation in conditions like arthritis, muscle strains, and injuries by inhibiting COX enzymes by reducing the production pf prostaglandins.[5]
- Corticosteroids, like Prednisone, Prednisolone, and Dexamethasone, are potent anti-inflammatory drugs mimicking adrenal gland hormones. They treat various inflammatory conditions, including asthma, rheumatoid arthritis, and skin issues, topically, orally, or via injections.
- Antihistamines, like Cetirizine, Loratadine, and Fexofenadine, relieve allergic reactions and have anti-inflammatory effects by blocking histamine.
- Analgesics, like Acetaminophen and Tramadol, are pain relievers with mild anti-inflammatory effects, but may be preferred due to lower stomach irritation risks.
- Biologics are DMARDs targeting immune system molecules involved in inflammation, used in treating autoimmune diseases like rheumatoid arthritis and psoriasis.
- Immunosuppressants suppress the immune system, reducing inflammation and preventing organ rejection in transplant patients. Examples include Infliximab, Adalimumab, and Etanercept.
Natural approaches and lifestyle changes involve the use of diets, exercises and stress reduction.
- Dietary approaches to reduce inflammation include omega-3 fatty acids, antioxidant-rich foods, and the Mediterranean diet [6] [7] Omega-3 fatty acids modulate inflammatory pathways, while antioxidant-rich foods, such as fruits and vegetables, suppress inflammatory mediators. Herbal remedies, such as curcumin, ginger, and boswellia serrata, also have anti-inflammatory properties.[8]
- Avoiding smoking and alcohol and reducing stress levels. Cumulative smoking (pack-years) and time since smoking cessation were strongly associated with blood levels of some inflammatory markers[9].
- Exercise is an essential component in managing both acute and chronic inflammation. In human clinical trials, it has been shown that energy expenditure through exercise lowers multiple pro-inflammatory molecules and cytokines independently of weight loss,[2] and improves immune function.
- Stress management techniques, such as meditation, yoga, and deep breathing techniques, can also help reduce inflammatory markers. Some studies show that yoga-based lifestyle interventions are efficacious in reducing oxidative stress and risk of chronic diseases even in a short duration[10].
- Sleep quality is another factor that can exacerbate inflammation, and prioritizing sufficient and restorative sleep can have a positive impact on the body's inflammatory response. Poor sleep has been associated with increased levels of inflammatory markers[11].
Physiotherapy[edit | edit source]
A physical therapist can be an educator on risk reduction and lifestyle modifications. The emphasis is on diet and lifestyle modification, e.g., weight loss, regular exercise, smoking cessation, a healthy diet, and good sleep hygiene.
It's important to note that these lifestyle modifications should be done in consultation with healthcare professionals, such as a physical therapist or a registered dietitian, to ensure they are tailored to individual needs and health conditions.
References[edit | edit source]
- ↑ 1.0 1.1 Chen L, Deng H, Cui H, et al. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2017;9(6):7204-7218. Published 2017 Dec 14. doi:10.18632/oncotarget.23208 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5805548/(accessed 22.1.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 Pahwa R, Jialal I. Chronic inflammation.2019 Available from:https://www.ncbi.nlm.nih.gov/books/NBK493173/ (accessed 21.1.2021)
- ↑ The Conversation Explainer: what is inflammation and how does it cause disease? Available from: https://theconversation.com/explainer-what-is-inflammation-and-how-does-it-cause-disease-84997(accessed 23.1.2021)
- ↑ The washington post Chronic Inflammation Available from: https://www.washingtonpost.com/health/chronic-inflammation-is-long-lasting-insidious-dangerous-and-you-may-not-even-know-you-have-it/2020/01/17/93ab0fa2-316f-11ea-9313-6cba89b1b9fb_story.html (accessed22.1.2021)
- ↑ Crofford LJ. Use of NSAIDs in treating patients with arthritis. Arthritis research & therapy. 2013 Jul;15:1-0.
- ↑ Haß U, Herpich C, Norman K. Anti-inflammatory diets and fatigue. Nutrients. 2019 Sep 30;11(10):2315.
- ↑ Health line Understanding and Managing Chronic Inflammation Available from: https://www.healthline.com/health/chronic-inflammation(last accessed 23.1.2021)
- ↑ Kantor ED, Lampe JW, Kratz M, White E. Lifestyle factors and inflammation: associations by body mass index. PloS one. 2013 Jul 2;8(7):e67833.
- ↑ J. Sunyer et al. "Interaction between smoking and the interleukin-6 gene affects systemic levels of inflammatory biomarkers.." Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco, 11 11 (2009): 1347-53. https://doi.org/10.1093/ntr/ntp144.
- ↑ R. Yadav et al. "Efficacy of a short-term yoga-based lifestyle intervention in reducing stress and inflammation: preliminary results.." Journal of alternative and complementary medicine, 18 7 (2012): 662-7. https://doi.org/10.1089/acm.2011.0265.
- ↑ J. Dzierzewski et al. "Sleep Inconsistency and Markers of Inflammation." Frontiers in Neurology, 11 (2020).