Heterotopic Ossification: Difference between revisions
No edit summary |
No edit summary |
||
| (209 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- Bruce Tan as part of the [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | |||
'''Original Editors '''- Bruce Tan | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
''' | == Introduction == | ||
Heterotopic ossification is seen often in [[Rehabilitation Contexts|rehabilitation]] population. It refers to the formation of mature, lamellar [[bone]] in extraskeletal soft tissue where bone should not be. Patients at risk of developing heterotopic ossification include patients with [[Burns Overview|burns]], [[Stroke|strokes]], [[Spinal Cord Injury|spinal cord injuries (SCI)]], [[amputations]], joint replacements, and [[Overview of Traumatic Brain Injury|traumatic brain injuries (TBI)]].<ref name=":0">Sun E, Hanyu-Deutmeyer AA. [https://www.ncbi.nlm.nih.gov/books/NBK519029/ Heterotopic Ossification].Available: https://www.ncbi.nlm.nih.gov/books/NBK519029/<nowiki/>(accessed 24.10.2021)</ref> | |||
* Lesions range from small, clinically insignificant foci of ossification to large deposits of bone that cause pain and restriction. | |||
* The most common presentation is with pain around the ossification site<ref>Radiopedia [https://radiopaedia.org/articles/heterotopic-ossification HO] Available: https://radiopaedia.org/articles/heterotopic-ossification<nowiki/>(accessed 24.10.2021)</ref> | |||
<br> | |||
<div class="row"> | |||
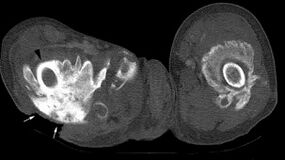
<div class="col-md-6">[[Image:HO CT scan.jpg|center|alt=|thumb|'''Figure.1''' CT Scan showing Heterotopic Ossification of Proximal Femur|285x285px]]</div> | |||
<div class="col-md-6">[[Image:Ho1.jpg|center|alt=|thumb|'''Figure.2''' Radiograph showing Heterotopic Ossification of the Hip|213x213px]]</div> | |||
</div> | </div> | ||
== Etiology == | |||
The exact mechanism of heterotopic ossification (HO) in traumatic and neurogenic heterotopic ossification is unknown, but two common factors precede the formation of heterotopic ossification , the first being trauma or an inciting neurological event. | |||
# Traumatic (fracture, arthroplasty, muscular trauma, joint dislocation, burns). In total joint arthroplasty, heterotopic ossification most commonly occurs for the [[Total Hip Replacement|rep]]<nowiki/>[[Total Hip Replacement|lacement of hips]], [[Total Knee Arthroplasty|knees]], elbow, and [[Total Shoulder Arthroplasty|shoulder]]. Chronic muscular trauma leads to what is traditionally known specifically as traumatic [[Myositis Ossificans|myositis ossificans]]. The most common sites for traumatic [[Myositis Ossificans|myositis ossificans]] are the [[Quadriceps Muscle|quadriceps femoris]] muscle and the [[brachialis]] muscle. | |||
# Neurogenic (Stroke, SCI, TBI, Brain Tumors). The most common sites for neurogenic heterotopic ossification are the hips, elbows (extensor side), shoulders, and knees. Uncommon sites of heterotopic ossification that may be encountered in a rehabilitation setting are incisions, [[Kidney|kidneys]], uterus, corpora cavernosum, and the gastrointestinal tract. The exact cause and mechanism of neurogenic heterotopic ossification are unknown. | |||
=== Risk Factors === | |||
*[[Spasticity]], [[Older People - An Introduction|older age]], [[Pressure Ulcers|pressure ulcer]], the presence of [[Deep Vein Thrombosis|deep vein thrombosis,]] having a tracheostomy, long bone [[Fracture|fractures]], prior injury to the same area, [[Oedema Assessment|edema]], immobility, long-term [[Coma Recovery Scale (Revised)|coma]], and severity of injury (Trauma, TBI, SCI, Stroke). | |||
* High/Moderate risk factors in the THA population include men with bilateral THA, prior history of heterotopic ossification, [[Ankylosing Spondylitis (Axial Spondyloarthritis)|ankylosing spondylitis]], diffuse idiopathic hyperostosis, or [[Paget's Disease]].<ref name=":0" /> | |||
== Epidemiology == | |||
* Heterotopic Ossification is twice as common in males versus females, but it is noted that females older than 65 years old have an increased risk of developing heterotopic ossification. | |||
* The incidence of neurogenic heterotopic ossification is 10% to 20%.<ref name=":0" /> | |||
* Following lower extremity amputation: 7%<sup><ref name="p6">Hsu JE, Keenan MA. Current review of heterotopic ossification. UPOJ 2010; 20: 126-130.</ref></sup> | |||
* Following SCI: 20% (ranges reported from 20-40%)<sup><ref name="p6" /></sup> | |||
* Following [[Total Hip Replacement|THA (total hip arthroplasty)]]: 55%<sup><ref name="p1">Mavrogenis AF, Soucacos PN, Papagelopoulos PJ. Heterotopic Ossification Revisited. Orthopedics. 2011Jan;34(3):177.</ref></sup> | |||
* Following Elbow Fracture and/or Dislocation: 90%<ref name="p8">Dalury DF, Jiranek WA. The incidence of heterotopic ossification after total knee arthroplasty. Journal of Arthroplasty 2004; 19: 447-457.</ref><br> | |||
== Signs and Symptoms == | |||
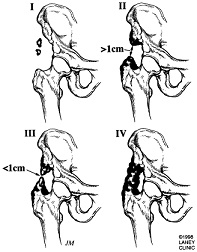
[[Image:Heterotopic.jpg|frame|right|'''Figure.3''' Heterotopic Ossification Progression of the Hip]]Clinical signs and symptoms of heterotopic ossification may appear as soon as 3 weeks or up to 12 weeks after initial musculoskeletal trauma, spinal cord injury, or other precipitating events.<sup><ref name="p9">Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. Jour of Nuclear Medicine 2002; 43: 346-353.</ref></sup> The first sign of heterotopic ossification is generally loss of joint mobility and subsequently loss of function. Other findings that may suggest the presence of heterotopic ossification include swelling, erythema, heat, pain depending on sensory deficit, hard, palpable mass, pressure area, contracture formation and spasticity and autonomic dysreflexia in individuals with spinal cord injury. In some cases, a fever may be present.<sup><ref name="p1" /> </sup> | |||
#'''Symptoms:''' Painless Loss of ROM, Interferes with activities of daily living) ADL, [[Complex Regional Pain Syndrome (CRPS)|Complex regional pain syndrome) CRPS]], [[Fever]] | |||
#'''Inspection:''' Warm, Painful, Swollen Joint; may have effusion; Skin Problems (pressure ulcers from contractures around skin, muscles, ligaments, skin maceration and hygiene problems) | |||
#'''Movement:''' Decreased Joint ROM; Joint Ankylosis; with heterotopic ossification after [[Total Knee Arthroplasty|total knee arthroplasty]] (TKA), might develop quadricep muscle snapping or patella instability | |||
#'''Neurovascular:''' Peripheral Neuropathy; heterotopic ossification often impinges on adjacent neurovascular structures<ref name=":1">Orthobullets [https://www.orthobullets.com/pathology/8044/heterotopic-ossification HO] Available: https://www.orthobullets.com/pathology/8044/heterotopic-ossification<nowiki/>(accessed 24.10.2021)</ref> | |||
== | =='''Differential Diagnoses'''== | ||
The initial inflammatory phase of heterotopic ossification may mimic other pathologies such as cellulitis, thrombophlebitis, osteomyelitis, or a tumorous process.<sup><ref name="p3">Firoozabadi R, Alton T, Sagi HC. Heterotopic Ossification in Acetabular Fracture Surgery. Journal of the American Academy of Orthopaedic Surgeons. 2017;25(2):117–24.</ref></sup><ref name="p4">Bossche LV, Vanderstraeten G. Heterotopic ossification: a review. J Rehabil Med 2005; 37: 129-136.5. Pape HC et al. Current concepts in the development of hetetrotopic ossification. Journ Bone and Joint Surg 2004; 86: 783-787.</ref> | |||
Other differential diagnoses include [[Deep Vein Thrombosis|deep veinous thrombosis (DVT]]), [[Septic (Infectious) Arthritis|Septic Arthritis]], Haematoma, or [[Fracture]]. DVT and heterotopic ossification have been positively associated. This is thought to be due to the mass effect and local inflammation of the HO, encouraging thrombus formation. The thrombus formation is caused by venous compression and phlebitis.<sup><ref name="p1" /></sup> | |||
== Diagnosis == | |||
Diagnosis is made when soft tissue ossification with sharp demarcation from surrounding soft tissues is seen on radiograph.<ref name=":1" /> However, plain radiographs may not be able to detect early lesions, so ultrasonography is more commonly used as an early screening modality, despite magnetic resonance imaging remaining the gold standard for imaging of soft tissue masses.<ref name=":2">Devilbiss Z, Hess M, Ho GWK. [https://pubmed.ncbi.nlm.nih.gov/30204632/ Myositis Ossificans in Sport: A Review]. Curr Sports Med Rep. 2018 Sep;17(9):290-295. doi: 10.1249/JSR.0000000000000515. PMID: 30204632. Available:https://pubmed.ncbi.nlm.nih.gov/30204632/ (accessed 25.10.2021)</ref><div class="row"> | |||
<div class="col-md-6">[[Image:Shoulder HO CT 2.JPG|center|'''Figure.4''' CT Scan showing Heterotopic Ossification of the Shoulder|alt=|thumb|300x300px]]</div> | |||
<div class="col-md-6">[[Image:Shoulder HO Xray 2.JPG|center|'''Figure.5''' AP X-ray Showing Heterotopic Ossification of Shoulder|alt=|thumb|300x300px]]</div> | |||
</div> | |||
''' | |||
== Associated Co-Morbidities == | |||
The most common conditions found in conjunction with heterotopic ossification:<sup><ref name="p4" /> <ref name="p2">McCarthy EF, Sundaram M. Heterotopic ossification: a review. Skeletal Radiol 2005; 34: 609-619.</ref></sup> | |||
* | *[[Ankylosing Spondylitis]] | ||
* | *[[Rheumatoid Arthritis|Rhuematoid Arthritis]]<sup><ref name="p7">Foruria AM, Augustin S, Morrey BF, Sanchez-Sotelo Joaquin. Heterotopic Ossification After Surgery for Fractures and Fractures-Dislocations Involving the Proximal Aspect of the Radius or Ulna. The Journal of Bone and Joint Surgery, Incorporated. 2015May15;95-A(10):e66(1)-e66(7).</ref></sup> | ||
*Hypertrophic Osteoarthritis | |||
* | *[[Diffuse Idiopathic Skeletal Hyperostosis]] | ||
* | *[[Paget's Disease]] | ||
*[[Spinal Cord Injury]] <br> | |||
== Treatment == | |||
Heterotopic Ossification is best managed by an interprofessional team. The condition is not only difficult to diagnose because of lack of specific markers but its treatment is not satisfactory. Current treatment recommendations consist of mobilisations with gentle ROM exercises, indomethacin, etidronate, and surgical resection. | |||
* Early treatment with a passive range of motion exercises should be implemented once the presence of HO is confirmed to prevent ankylosing of joints. | |||
* Absolute treatment consists of surgical resection of mature bone once the HO has fully matured. This can be 12 to 18 months after the initial presentation. | |||
* Surgical consultation with an orthopaedic surgeon is warranted only if there will be an improvement in function as demonstrated by mobility, transfers, hygiene, and ADLs. | |||
* Indomethacin and etidronate are also used to help arrest bone formation in HO, but efficacy in the traumatic brain injury population has not been clearly proven (see below). | |||
* The most effective treatment option in the TBI population is surgical resection. In the SCI population, the most effective [[NSAIDs|Non-Steroidal Anti-Inflammatory Drugs (NSAID)]] treatment regiments are either Rofecoxib 25 mg per day for 4 weeks or indomethacin 75 mg daily for 3 weeks.<ref name=":0" /> | |||
== Medications == | |||
* | The two types of medications shown to have both prophylactic and treatment benefits are as follows: | ||
* | # Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)<br>Indomethacin (two-fold action) | ||
#* Inhibition of the differentiation of mesenchymal cells into osteogenic cells (direct) | |||
* | #* Inhibition of post-traumatic bone remodelling by suppression of prostaglandin-mediated response (indirect) and anti-inflammatory properties | ||
* | # Biphosphonates: Three-fold action | ||
* | #* Inhibition of calcium phosphate precipitation | ||
#* Slowing of hydroxyapatite crystal aggregation | |||
#* Inhibition of the transformation of calcium phosphate to hydroxyapatite. | |||
== '''Surgical Interventions''' == | |||
The two main goals of surgical intervention are to | |||
# Alter the position of the affected joint | |||
# Improve its range of motion (ROM).<ref name="p5">Pape HC et al. Current concepts in the development of hetetrotopic ossification. Journ Bone and Joint Surg 2004; 86: 783-787.</ref> | |||
<br> | <br> | ||
Rehabilitation Post-Operatively: It is recommended that a rehabilitation program should start within the first 24 hours after surgery. The program should last for 3 weeks to prevent adhesion.<sup><ref name="p7" /></sup> | |||
== Prognosis == | |||
Complications of heterotopic ossification present itself through decreased function and mobility, peripheral nerve entrapment, and pressure ulcers. | |||
# Up to 70% of cases involving HA are asymptomatic. | |||
# Ankylosis, vascular compression, and lymphedema can also be complications manifested in HO. | |||
# Prognosis is generally good after surgery. Mean time from injury to surgery is 3.6 years. Once the surgery is performed, studies have shown that average ROM in the hip can improve from 24.3 to. After surgery, improvement was maintained in follow up 6 months after surgery. Complications from surgical resection of HO, such as infection, severe hematoma, and DVT<ref name=":0" /> | |||
<br> | <br> | ||
In the case of sporting myositis ossificans, usually athletes are able to progress to light activity at 2 to 3 months, full activity by 6 months, and back to their pre-injury level by 1 year.<ref name=":2" /> | |||
== Physical Therapy Management == | |||
Physical therapy has been shown to benefit patients suffering from heterotopic ossification. Pre-operative PT can be used to help preserve the structures around the lesion. ROM exercises (PROM, AAROM, AROM) and strengthening will help prevent muscle atrophy and preserve joint motion. <blockquote>'''''Clinical Note''''': Caution must be taken when working with patients with known heterotopic lesions. Therapy which is too aggressive can aggravate the condition and lead to inflammation, erythema, haemorrhage, and increased pain. </blockquote>Post-operative rehabilitation has also shown to benefit patients with recent surgical resection of heterotopic ossification. The post-op management of HO is similar to pre-op treatment but much more emphasis is placed on [[Edema Assessment|edema]] control, [[Scar Management|scar management]], and [[Infection Prevention and Control|infection prevention]]. Calandruccio et al. outlined a rehabilitation protocol for patients who underwent surgical excision of heterotopic ossification of the elbow. The phases of rehab and goals for each phase are as follows:<sup><ref name="p6"/></sup> | |||
''' | |||
''' | |||
The | |||
| === Phase I''' '''(Week 1) === | ||
[[Image:Elbow HO.png|frame|right|Elbow Heterotopic Ossification]] | |||
'''Goals:''' | |||
#Prevent infection | #Prevent infection | ||
| Line 221: | Line 109: | ||
#Maintain ROM of joint proximal and distal to surgical site | #Maintain ROM of joint proximal and distal to surgical site | ||
=== Phase II (2-8 Weeks) === | |||
'''Goals:''' | |||
#Reduce | #Reduce ain | ||
#Manage | #Manage [[Oedema Assessment|Edema]] | ||
#Encourage limited ADL performances | #Encourage limited ADL performances | ||
#Promote | #Promote Scar Mobility and proper remodeling | ||
#Promote full ROM of affected joint | #Promote full ROM of affected joint | ||
#Encourage quality muscle contractions [[Image:Hand-elbow-horiz01.jpg|frame|right|Photo courtesy of prosportscare.com]] | #Encourage quality muscle contractions [[Image:Hand-elbow-horiz01.jpg|frame|right|Photo courtesy of prosportscare.com]] | ||
=== Phase III (9-24 Weeks) === | |||
'''Goals:''' | |||
#Self-manage | #Self-manage Pain | ||
#Prevent flare-up with functional activities | #Prevent flare-up with functional activities | ||
#Improve | #Improve Strength | ||
#Improve ROM (if still limited) | #Improve ROM (if still limited) | ||
#Return to previous levels of activity | #Return to previous levels of activity | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Bone - Conditions]] | |||
[[Category:Neurological - Conditions]] | |||
Latest revision as of 02:02, 9 March 2023
Original Editors - Bruce Tan as part of the from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Bruce Tan, Morgan Yoder, Hannah McCabe, Naomi O'Reilly, Lucinda hampton, Admin, Elaine Lonnemann, 127.0.0.1, Wendy Walker, WikiSysop and Kim JacksonIntroduction[edit | edit source]
Heterotopic ossification is seen often in rehabilitation population. It refers to the formation of mature, lamellar bone in extraskeletal soft tissue where bone should not be. Patients at risk of developing heterotopic ossification include patients with burns, strokes, spinal cord injuries (SCI), amputations, joint replacements, and traumatic brain injuries (TBI).[1]
- Lesions range from small, clinically insignificant foci of ossification to large deposits of bone that cause pain and restriction.
- The most common presentation is with pain around the ossification site[2]
Etiology[edit | edit source]
The exact mechanism of heterotopic ossification (HO) in traumatic and neurogenic heterotopic ossification is unknown, but two common factors precede the formation of heterotopic ossification , the first being trauma or an inciting neurological event.
- Traumatic (fracture, arthroplasty, muscular trauma, joint dislocation, burns). In total joint arthroplasty, heterotopic ossification most commonly occurs for the replacement of hips, knees, elbow, and shoulder. Chronic muscular trauma leads to what is traditionally known specifically as traumatic myositis ossificans. The most common sites for traumatic myositis ossificans are the quadriceps femoris muscle and the brachialis muscle.
- Neurogenic (Stroke, SCI, TBI, Brain Tumors). The most common sites for neurogenic heterotopic ossification are the hips, elbows (extensor side), shoulders, and knees. Uncommon sites of heterotopic ossification that may be encountered in a rehabilitation setting are incisions, kidneys, uterus, corpora cavernosum, and the gastrointestinal tract. The exact cause and mechanism of neurogenic heterotopic ossification are unknown.
Risk Factors[edit | edit source]
- Spasticity, older age, pressure ulcer, the presence of deep vein thrombosis, having a tracheostomy, long bone fractures, prior injury to the same area, edema, immobility, long-term coma, and severity of injury (Trauma, TBI, SCI, Stroke).
- High/Moderate risk factors in the THA population include men with bilateral THA, prior history of heterotopic ossification, ankylosing spondylitis, diffuse idiopathic hyperostosis, or Paget's Disease.[1]
Epidemiology[edit | edit source]
- Heterotopic Ossification is twice as common in males versus females, but it is noted that females older than 65 years old have an increased risk of developing heterotopic ossification.
- The incidence of neurogenic heterotopic ossification is 10% to 20%.[1]
- Following lower extremity amputation: 7%[3]
- Following SCI: 20% (ranges reported from 20-40%)[3]
- Following THA (total hip arthroplasty): 55%[4]
- Following Elbow Fracture and/or Dislocation: 90%[5]
Signs and Symptoms[edit | edit source]
Clinical signs and symptoms of heterotopic ossification may appear as soon as 3 weeks or up to 12 weeks after initial musculoskeletal trauma, spinal cord injury, or other precipitating events.[6] The first sign of heterotopic ossification is generally loss of joint mobility and subsequently loss of function. Other findings that may suggest the presence of heterotopic ossification include swelling, erythema, heat, pain depending on sensory deficit, hard, palpable mass, pressure area, contracture formation and spasticity and autonomic dysreflexia in individuals with spinal cord injury. In some cases, a fever may be present.[4]
- Symptoms: Painless Loss of ROM, Interferes with activities of daily living) ADL, Complex regional pain syndrome) CRPS, Fever
- Inspection: Warm, Painful, Swollen Joint; may have effusion; Skin Problems (pressure ulcers from contractures around skin, muscles, ligaments, skin maceration and hygiene problems)
- Movement: Decreased Joint ROM; Joint Ankylosis; with heterotopic ossification after total knee arthroplasty (TKA), might develop quadricep muscle snapping or patella instability
- Neurovascular: Peripheral Neuropathy; heterotopic ossification often impinges on adjacent neurovascular structures[7]
Differential Diagnoses[edit | edit source]
The initial inflammatory phase of heterotopic ossification may mimic other pathologies such as cellulitis, thrombophlebitis, osteomyelitis, or a tumorous process.[8][9]
Other differential diagnoses include deep veinous thrombosis (DVT), Septic Arthritis, Haematoma, or Fracture. DVT and heterotopic ossification have been positively associated. This is thought to be due to the mass effect and local inflammation of the HO, encouraging thrombus formation. The thrombus formation is caused by venous compression and phlebitis.[4]
Diagnosis[edit | edit source]
Diagnosis is made when soft tissue ossification with sharp demarcation from surrounding soft tissues is seen on radiograph.[7] However, plain radiographs may not be able to detect early lesions, so ultrasonography is more commonly used as an early screening modality, despite magnetic resonance imaging remaining the gold standard for imaging of soft tissue masses.[10]
Associated Co-Morbidities[edit | edit source]
The most common conditions found in conjunction with heterotopic ossification:[9] [11]
- Ankylosing Spondylitis
- Rhuematoid Arthritis[12]
- Hypertrophic Osteoarthritis
- Diffuse Idiopathic Skeletal Hyperostosis
- Paget's Disease
- Spinal Cord Injury
Treatment[edit | edit source]
Heterotopic Ossification is best managed by an interprofessional team. The condition is not only difficult to diagnose because of lack of specific markers but its treatment is not satisfactory. Current treatment recommendations consist of mobilisations with gentle ROM exercises, indomethacin, etidronate, and surgical resection.
- Early treatment with a passive range of motion exercises should be implemented once the presence of HO is confirmed to prevent ankylosing of joints.
- Absolute treatment consists of surgical resection of mature bone once the HO has fully matured. This can be 12 to 18 months after the initial presentation.
- Surgical consultation with an orthopaedic surgeon is warranted only if there will be an improvement in function as demonstrated by mobility, transfers, hygiene, and ADLs.
- Indomethacin and etidronate are also used to help arrest bone formation in HO, but efficacy in the traumatic brain injury population has not been clearly proven (see below).
- The most effective treatment option in the TBI population is surgical resection. In the SCI population, the most effective Non-Steroidal Anti-Inflammatory Drugs (NSAID) treatment regiments are either Rofecoxib 25 mg per day for 4 weeks or indomethacin 75 mg daily for 3 weeks.[1]
Medications[edit | edit source]
The two types of medications shown to have both prophylactic and treatment benefits are as follows:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
Indomethacin (two-fold action)- Inhibition of the differentiation of mesenchymal cells into osteogenic cells (direct)
- Inhibition of post-traumatic bone remodelling by suppression of prostaglandin-mediated response (indirect) and anti-inflammatory properties
- Biphosphonates: Three-fold action
- Inhibition of calcium phosphate precipitation
- Slowing of hydroxyapatite crystal aggregation
- Inhibition of the transformation of calcium phosphate to hydroxyapatite.
Surgical Interventions[edit | edit source]
The two main goals of surgical intervention are to
- Alter the position of the affected joint
- Improve its range of motion (ROM).[13]
Rehabilitation Post-Operatively: It is recommended that a rehabilitation program should start within the first 24 hours after surgery. The program should last for 3 weeks to prevent adhesion.[12]
Prognosis[edit | edit source]
Complications of heterotopic ossification present itself through decreased function and mobility, peripheral nerve entrapment, and pressure ulcers.
- Up to 70% of cases involving HA are asymptomatic.
- Ankylosis, vascular compression, and lymphedema can also be complications manifested in HO.
- Prognosis is generally good after surgery. Mean time from injury to surgery is 3.6 years. Once the surgery is performed, studies have shown that average ROM in the hip can improve from 24.3 to. After surgery, improvement was maintained in follow up 6 months after surgery. Complications from surgical resection of HO, such as infection, severe hematoma, and DVT[1]
In the case of sporting myositis ossificans, usually athletes are able to progress to light activity at 2 to 3 months, full activity by 6 months, and back to their pre-injury level by 1 year.[10]
Physical Therapy Management[edit | edit source]
Physical therapy has been shown to benefit patients suffering from heterotopic ossification. Pre-operative PT can be used to help preserve the structures around the lesion. ROM exercises (PROM, AAROM, AROM) and strengthening will help prevent muscle atrophy and preserve joint motion.
Clinical Note: Caution must be taken when working with patients with known heterotopic lesions. Therapy which is too aggressive can aggravate the condition and lead to inflammation, erythema, haemorrhage, and increased pain.
Post-operative rehabilitation has also shown to benefit patients with recent surgical resection of heterotopic ossification. The post-op management of HO is similar to pre-op treatment but much more emphasis is placed on edema control, scar management, and infection prevention. Calandruccio et al. outlined a rehabilitation protocol for patients who underwent surgical excision of heterotopic ossification of the elbow. The phases of rehab and goals for each phase are as follows:[3]
Phase I (Week 1)[edit | edit source]
Goals:
- Prevent infection
- Protect and decrease stress on surgical site
- Decrease pain
- Control and decrease edema
- ROM to 80% of affected joint
- Maintain ROM of joint proximal and distal to surgical site
Phase II (2-8 Weeks)[edit | edit source]
Goals:
- Reduce ain
- Manage Edema
- Encourage limited ADL performances
- Promote Scar Mobility and proper remodeling
- Promote full ROM of affected joint
- Encourage quality muscle contractions
Phase III (9-24 Weeks)[edit | edit source]
Goals:
- Self-manage Pain
- Prevent flare-up with functional activities
- Improve Strength
- Improve ROM (if still limited)
- Return to previous levels of activity
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Sun E, Hanyu-Deutmeyer AA. Heterotopic Ossification.Available: https://www.ncbi.nlm.nih.gov/books/NBK519029/(accessed 24.10.2021)
- ↑ Radiopedia HO Available: https://radiopaedia.org/articles/heterotopic-ossification(accessed 24.10.2021)
- ↑ 3.0 3.1 3.2 Hsu JE, Keenan MA. Current review of heterotopic ossification. UPOJ 2010; 20: 126-130.
- ↑ 4.0 4.1 4.2 Mavrogenis AF, Soucacos PN, Papagelopoulos PJ. Heterotopic Ossification Revisited. Orthopedics. 2011Jan;34(3):177.
- ↑ Dalury DF, Jiranek WA. The incidence of heterotopic ossification after total knee arthroplasty. Journal of Arthroplasty 2004; 19: 447-457.
- ↑ Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. Jour of Nuclear Medicine 2002; 43: 346-353.
- ↑ 7.0 7.1 Orthobullets HO Available: https://www.orthobullets.com/pathology/8044/heterotopic-ossification(accessed 24.10.2021)
- ↑ Firoozabadi R, Alton T, Sagi HC. Heterotopic Ossification in Acetabular Fracture Surgery. Journal of the American Academy of Orthopaedic Surgeons. 2017;25(2):117–24.
- ↑ 9.0 9.1 Bossche LV, Vanderstraeten G. Heterotopic ossification: a review. J Rehabil Med 2005; 37: 129-136.5. Pape HC et al. Current concepts in the development of hetetrotopic ossification. Journ Bone and Joint Surg 2004; 86: 783-787.
- ↑ 10.0 10.1 Devilbiss Z, Hess M, Ho GWK. Myositis Ossificans in Sport: A Review. Curr Sports Med Rep. 2018 Sep;17(9):290-295. doi: 10.1249/JSR.0000000000000515. PMID: 30204632. Available:https://pubmed.ncbi.nlm.nih.gov/30204632/ (accessed 25.10.2021)
- ↑ McCarthy EF, Sundaram M. Heterotopic ossification: a review. Skeletal Radiol 2005; 34: 609-619.
- ↑ 12.0 12.1 Foruria AM, Augustin S, Morrey BF, Sanchez-Sotelo Joaquin. Heterotopic Ossification After Surgery for Fractures and Fractures-Dislocations Involving the Proximal Aspect of the Radius or Ulna. The Journal of Bone and Joint Surgery, Incorporated. 2015May15;95-A(10):e66(1)-e66(7).
- ↑ Pape HC et al. Current concepts in the development of hetetrotopic ossification. Journ Bone and Joint Surg 2004; 86: 783-787.