Bone
Original Editors - Candace Goh
Top Contributors - Lucinda hampton, Candace Goh, Admin, Shaimaa Eldib, Kim Jackson, Wataru Okuyama, Jess Bell, Robin Tacchetti, George Prudden, Claire Knott, Manisha Shrestha, Khloud Shreif, Tony Lowe, Stephanie Geeurickx, WikiSysop, Joao Costa and Sai Kripa
Introduction[edit | edit source]
The function of bone tissue is both supportive and locomotive.[1] Bones not only provide the physical scaffold of the body but enable locomotion by providing attachment sites for muscles, tendons and ligaments.[2] In addition, bones permit motor capability, protect vital organs, facilitate breathing, play a role in homeostasis, and produce a variety of cells in the marrow critical for survival.[3] Bone tissue is unique in that it can regenerate, restoring to a fully-functional, pre-injury state.[2]
Bone is a metabolically active connective tissue that provides structural support, facilitates movement, and protects vital organs. Bone is composed of an extracellular matrix and bone cells (osteocytes).[4] Under the right conditions, bone tissue undergoes a process of mineralisation, and is hardened by deposited calcium. Bone is hard and many of its functions depend on that characteristic hardness.[5]
The adult human skeleton is composed of 206 bones. At birth, there are approximately 270 bones, with the final adult count decreasing as a portion of these bones fuse during phases of skeletal growth and maturation. During life, bone is constantly remodelling with most of the adult skeleton being replaced about every 10 years.[6]
Watch this 10 minute video on the skeletal system and why astronauts Scott Kelly and Mikhail Kornienko are out in space studying it. It also includes anatomy of the skeletal system, including the flat, short, and irregular bones, and their individual arrangements of compact and spongy
Bone Structure[edit | edit source]
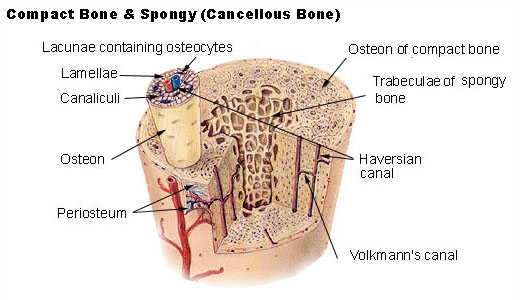
Bone consists of two types of tissue:
- Compact (cortical) bone: makes up 80% of the total bone in the body and is much stronger than cancellous/trabecular bone. It is very resistant to bending, torsion, and compression. It is much more dense and has a minimal role in metabolism. It is seen mostly in the shaft of long bones like the femur and the tibia as well as in the outer shell of trabecular bone
- Cancellous (trabecular or spongy) bone: makes up only 20% of the total bone but has ten times the surface/volume ratio of cortical bone. It responds eight times faster to changes in load making it far more dynamic. It occurs in areas that are more subject to compression such as the vertebral body, pelvis, and the metaphyses.[8]
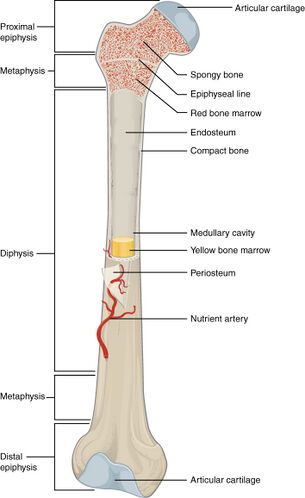
Bones also contain:
- Osteoblasts and osteocytes, responsible for creating bone
- Osteoclasts or bone resorbing cells
- Osteoid, a mix of collagen and other proteins
- Inorganic mineral salts within the extracellular matrix (ECM)
- Nerves and blood vessels
- Bone marrow
- Cartilage
- Membranes, including the endosteum and periosteum[9]
Bone Types[edit | edit source]
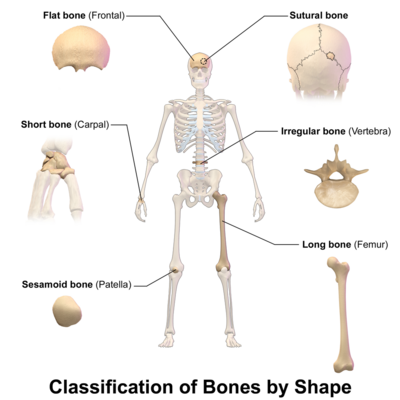
In the human body, five bone types exist:
- Long bones: Mostly made of compact bone, and have little marrow. Most bones in the limbs are long bones. These bones tend to support weight and help movement (e.g., femur, tibia, fibula, humerus).
- Short bones: Have only a thin layer of compact bone (e.g. bones of the wrist and ankle).
- Flat bones: Usually bones that are thin and curved. They consist of two outer layers of compact bone and an inner layer of spongy bone. Flat bones include most of the bones of the skull and the sternum or breastbone. They tend to have a protective role (e.g. sternum, ribs).
- Sesamoid bones: These are embedded in tendons (e,g, patella). They protect tendons from wear and stress.
- Irregular bones: As their name implies, these are bones that do not fit into the first four categories and have an unusual shape. They include the bones of the spine and pelvis. They are often protecting organs or tissues.
Gross Anatomy[edit | edit source]
A long bone has two parts, the diaphysis and the epiphysis. Bones that undergo endochondral ossification also have a physis (growth plate).
- The diaphysis is the tubular shaft that runs between the proximal and distal ends of the bone. The hollow region in the diaphysis is called the medullary cavity, which is filled with yellow marrow. The walls of the diaphysis are composed of dense and hard compact bone.[10]
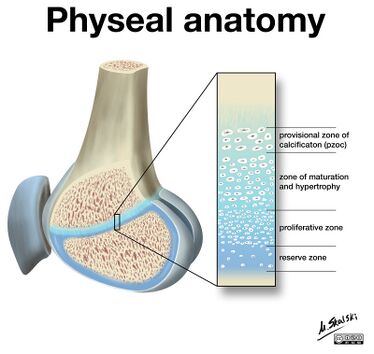
- The physes (singular: physis) or growth plates are found in bones that undergo endochondral ossification (the process by which the embryonic cartilaginous model of most bones contributes to longitudinal growth and is gradually replaced by bone).[11]
- The epiphysis - the part or process of a bone that ossifies separately and later becomes ankylosed to the main part of the bone. The epiphysis contributes to a joint, compared with an apophysis which is a site of tendon or ligament attachment. Once the growth plate has fused, the epiphysis and metaphysis are joined.
Bone Composition[edit | edit source]
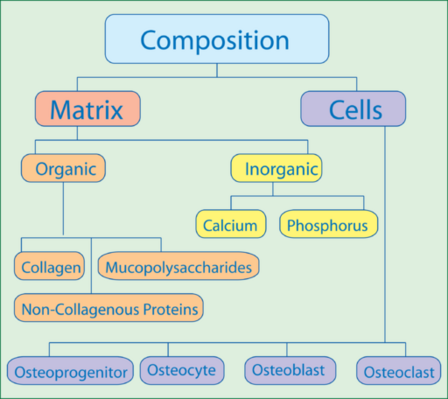
Bone is composed of cells and the extracellular matrix (ECM), which has both organic and inorganic substances. Osteoblasts synthesise bone ECM.
The ECM consists of:
- Type I collagen mixed with a matrix of calcium phosphate crystal (which is up to 70 % of the dry weight)
- Proteoglycans and glycoproteins, which are less abundant, but vital for the organisation of collagen fibers, mineralisation and resorption of bone. Chondroitin sulfate accounts for 67-97 % of the bone glycosaminoglycans.[12]
Bone Cells [edit | edit source]
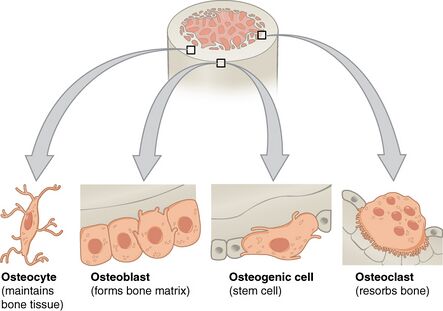
Bone cells make up about 10% of total bone volume. Bones are not a static tissue but need to be constantly maintained and remodelled. There are three main cell types involved in this process.
- Osteoblasts: Bone marrow stem cells can differentiate into osteoblasts. Osteoblasts are responsible for making new bone and repairing older bone. Osteoblasts produce a protein mixture called osteoid, which is mineralised and becomes bone. Another function is to manufacture hormones, including prostaglandins.
- Osteocytes: Inactive osteoblasts that have become trapped in the bone that they have created. They maintain connections to other osteocytes and osteoblasts. They are important for communication within bone tissue.
- Osteoclasts: Large cells with more than one nucleus, which break down bone. They release enzymes and acids to dissolve minerals in bone and digest them in a process called resorption. Osteoclasts help remodel injured bones and create pathways for nerves and blood vessels to travel through.[9]
Extracellular Matrix[edit | edit source]
Bones are, in reality, living cells embedded in a mineral-based organic matrix. This extracellular matrix consists of:
- organic components, being mostly type 1 collagen
- inorganic components, including hydroxyapatite and other salts, such as calcium and phosphate
Collagen gives bone its tensile strength, namely the resistance to being pulled apart. Hydroxyapatite gives bones compressive strength or resistance to being compressed.[9]
Bone Marrow and Hematopoiesis[edit | edit source]
Bone marrow is found in almost all bones where cancellous bone is present. Bone marrow is responsible for hematopoiesis, or the production of red blood cells, white blood cells, and platelets.[8] It makes around 2 million red blood cells every second, as well as producing platelets, and white blood cells. Defective and old red blood cells are also destroyed in the bone marrow.[9][8]
This 4 minute video explains Hematopoiesis: Formation of Blood Cells
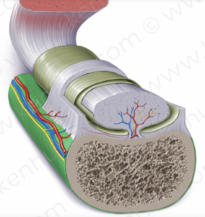
Functional Unit of Compact Bone[edit | edit source]
Osteons represents a single functional unit of bone tissue. It is arranged with concentric lamellae of collagen fibre orientations around a central canal "consisting of osteocyte’s arterial, venous, and nerve supply",[8] which is known as the Haversian canal. This system also includes the canaliculi and Volkmann canal. These allow for communication between neighboring osteocytes and osteons, respectively. Osteons are several millimetres long and about 0.2 millimetre (0.008 inch) in diameter; they tend to run parallel to the long axis of a bone.[8]
Mechanical Functions[edit | edit source]
- Protection. Bones are vital for protecting the important and fragile organs in the body. For example bones protect the heart and the brain.
- Structure. Without bones, our body would have no frame and essentially be an immobile lump of flesh and tissue.
- Movement. The bones pair up with the joints, ligaments, tendons and muscles to allow the body to move as it does.
- Sound Transduction. Bones are also important for conduction vibrations which allow us to hear.[14][8]
Metabolic Functions[edit | edit source]
The metabolic functions of the bone are many:
- The bone matrix can store several minerals, chiefly calcium and phosphorus as well as iron in the form of ferritin.
- Chondroitin sulfate, a carbohydrate moiety, is also a commonly found element in the matrices.
- Specific growth factors, including insulin-like growth factor or IGF-1, are housed in bone and then released periodically.
- pH balance is also regulated as bones may alter the composition of alkaline salts in the serum to maintain the optimal pH level.
- Osteocytes can engulf toxic molecules and heavy metals from the serum as a means of detoxification.
- Fat storage.[8]
Remodelling[edit | edit source]
This is a physiological process in which old or damaged bone is removed by osteoclasts and then replaced by new bone formed by osteoblasts.[15] [16] There is a tight coupling of bone formation to bone resorption to ensure no net change in bone mass or quality after each remodelling. It requires coordinated action of the four types of bone cells. The process involves four major distinct but overlapping phases:
- Initiation/activation of bone remodelling at a specific site. The osteoclast precursors are recruited to bone remodelling compartments (BRC).
- Bone resorption and concurrent recruitment of osteoprogenitors. Bone resorption represents the predominant event, but the recruitment of mesenchymal stem cells (MSCs) and/or osteoprogenitors into the BRC is also initiated.
- Osteoblast differentiation and function (osteoid synthesis). Excavated bone is replaced with osteoid produced by osteoblasts.
- Mineralisation of osteoid and completion of bone remodelling.[4]
Watch this 8 minute video on bone remodeling .
Clinical Significance[edit | edit source]
Bone tissue is susceptible to a myriad of pathologies that may range from aetiologies of embryological, metabolic, autoimmune, neoplastic, or idiopathic origins. These include, but are not limited to, the conditions discussed below.
- Achondroplasia is a genetic disorder commonly associated as a cause of dwarfism. Individuals affected may present with short extremities due to decreased development of endochondral bone.
- Paget disease of the bone is characterised to be an imbalance amongst the activities of osteoblasts and osteoclasts. Of unknown aetiology, the condition only affects localised portions of the skeletal tissue, generally involving one or more neighboring bones rather than the whole skeletal system.
- If untreated, Paget disease of the bone can act as a risk factor for osteosarcoma, a malignant proliferation of osteoblasts.
- Skeletal neoplasm begins in the metaphysis of long bones. Patients may report bone pain with swelling or a pathologic fracture may occur (i.e. a break in the bone caused by weakness of the bone through disease rather than trauma). This is much more common in teenagers than in the elderly.[8]
- Bone fractures
- Osteoporosis. This is a common disorder of bone remodelling which is characterised by low bone mass and structural deterioration of bone. It causes bone fragility and increased vulnerability to fractures.[4]
- Osteoarthritis
- Osteomalacia
- Rickets
- Epiphyseal plate disorders
References[edit | edit source]
- ↑ Proia P, Amato A, Drid P, Korovljev D, Vasto S, Baldassano S. The impact of diet and physical activity on bone health in children and adolescents. Frontiers in Endocrinology. 2021;12.
- ↑ 2.0 2.1 Salhotra A, Shah HN, Levi B, Longaker MT. Mechanisms of bone development and repair. Nature reviews Molecular cell biology. 2020 Nov;21(11):696-711.
- ↑ Cowan PT, Kahai P. Anatomy, Bones.[Updated 2021 Jul 26]. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2022.
- ↑ 4.0 4.1 4.2 El Sayed SA, Nezwek TA, Varacallo M. Physiology, Bone. InStatPearls [Internet] 2019 Jul 29. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK441968/ (last accessed 10.2.2020)
- ↑ Opentextbc.ca. (2018). 6.3 Bone Structure – Anatomy and Physiology. [online] Available at: https://opentextbc.ca/anatomyandphysiology/chapter/6-3-bone-structure/
- ↑ Office of the Surgeon General (US. The Basics of Bone in Health and Disease. InBone Health and Osteoporosis: A Report of the Surgeon General 2004. Office of the Surgeon General (US). Available from:https://www.ncbi.nlm.nih.gov/books/NBK45504/ (last accessed 10.2.2020)
- ↑ Crash Course. The Skeletal System: Crash Course Anatomy & Physiology #19. Available from: http://www.youtube.com/watch?v=dMH0bHeiRNg [last accessed 7.8.2022]
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 Baig MA, Bacha D. Histology, Bone. InStatPearls [Internet] 2019 May 5. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK541132/ (last accessed 10.2.2020)
- ↑ 9.0 9.1 9.2 9.3 Medical News Today Bones Available:https://www.medicalnewstoday.com/articles/320444#The-structure-of-bones (accessed 7.8.2022)
- ↑ Hall JE. Guyton and Hall textbook of medical physiology e-Book. Elsevier Health Sciences; 2015 May 31.
- ↑ Radiopedia Physes Available:https://radiopaedia.org/articles/physis?lang=us (accessed 8.8.2022)
- ↑ Mmegias ECM Available: https://mmegias.webs.uvigo.es/02-english/5-celulas/2-tipos_mat_met.php (accessed 28.6.2022)
- ↑ Alila Medical Media. Hematopoiesis - Formation of Blood Cells, Animation. Available from: https://www.youtube.com/watch?v=0deCbmh7PHs [last accessed 7.8.2022]
- ↑ Med net health Functions of bones Available: http://www.med-health.net/Functions-Of-Bones.html (accessed 7.8.2022)
- ↑ Epsley S, Tadros S, Farid A, Kargilis D, Mehta S, Rajapakse CS. The effect of inflammation on bone. Frontiers in physiology. 2021:1695.
- ↑ Ofer L, Dean MN, Zaslansky P, Kult S, Shwartz Y, Zaretsky J, Griess-Fishheimer S, Monsonego-Ornan E, Zelzer E, Shahar R. A novel nonosteocytic regulatory mechanism of bone modeling. PLoS biology. 2019 Feb 1;17(2):e3000140.
- ↑ Physiology for Hippies . How are bones remodeled?. Available from: https://www.youtube.com/watch?v=sNfY8z3CqDg [last accessed 8.8.2022]