Tibia
Original Editor - The Open Physio project
Top Contributors - Kim Jackson, Sai Kripa, Admin, Daphne Jackson, WikiSysop, 127.0.0.1, Rachael Lowe, Rucha Gadgil and Pinar Kisacik
Introduction[edit | edit source]
The tibia is a medial and large long bone of the lower extremity, connecting the knee and ankle joints. It is considered to be the second largest bone in the body and it plays an important role in weight bearing.[1] Osteologic features of the tibia include medial and lateral condyles, the tibial plateau, the tibial tuberosity, the soleal line, the medial malleolus, and the fibular notch.
Osteologic Features[edit | edit source]
Tibial plateau[edit | edit source]
The proximal end of the tibia terminates in a broad, flat region called the tibial plateau. The intercondylar eminence runs down the midline of the plateau, separating the medial and lateral condyles of the tibia. The two condyles form a flat, broad surface for articulation with the medial and lateral condyles of the femur.[2]
Shaft[edit | edit source]
The tibial tuberosity is a palpable bony prominence located on the anterior surface of the proximal shaft of the tibia. On the posterior aspect of the tibia, the soleal line runs diagonally in a distal-to-medial direction across the proximal third of the tibia.[2]
Lateral Distal End[edit | edit source]
The lateral aspect of the distal tibia forms the fibular notch, creating an articulation between the distal tibia and fibula, the distal tibiofibular joint.[3]
Medial Distal End-Medial Malleolus[edit | edit source]
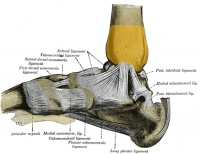
The medial malleolus is the medial surface of the distal portion of the tibia.[4] It is prolonged downward to form a strong pyramidal process and flattened from without, inward.
The medial surface of this process is convex and subcutaneous. The lateral, or articular surface, is smooth and slightly concave, and articulates with the talus. The anterior border is rough, for the attachment of the anterior fibers of the deltoid ligament of the ankle joint. The posterior border presents a broad groove, the malleolar sulcus, directed obliquely downward and medially, and occasionally double; this sulcus contains the tendons of the tibialis posterior and flexor digitorum longus. The summit of the medial malleolus is marked by a rough depression behind, for the attachment of the deltoid ligament.
Blood supply[edit | edit source]
The Tibia bone is supplied by nutrient artery which is considered as the largest nutrient artery in the human body. Posterior tibial artery mainly enters the bone through its posterior surface and nutrient artery is the branch of this posterior tibial artery.[5]
Muscles[edit | edit source]
- The Semimembranosus muscle originates from the ischial tuberosity and gets insert on the medial condyle of tibia.[5]
- The Tibialis anterior muscle gets attach on the shaft of the tibia. It originates from the upper 2/3rd area of lateral surface of the shaft. The primary action of tibialis anterior is dorsiflexion and inversion of the foot.[5]
- Sartorius, gracilis and semitendinosus are inserted on the upper part of medial surface of the shaft of tibia.[5]
- The soleus muscle originates from the soleal line present on the medial border of tibia and it primarily performs plantar flexion.[5]
- The popliteus muscle originates from the lateral epicondyle of femur and gets insert on the triangular area that is present above the soleal line.[5]
Articulations[edit | edit source]
Proximally, the tibia articulates with the femur to form the tibial-femoral joint of the knee.[4]
Distally, the tibia articulates with the talus to form the talocrural joint of the ankle.[4]
Although not functionally a part of the knee, the fibula articulates proximally with the lateral aspect of the tibia, forming the proximal tibiofibular joint. The distal tibiofibular joint is formed by the articulation of the distal tibia and fibula. There is relatively little movement at the proximal and distal tibiofibular joints.[2][3]
Functions[edit | edit source]
The primary function of the tibia is to accept and distribute weight across the knee and to the ankle.[2] The tibia's articulations with the relatively non-weight bearing fibula serve to maintain alignment of the tibia. Distally, the concave surface formed by the medial malleolus of the tibia and the lateral malleolus of the fibula creates a stable enclosure for the talocrural joint.[3]
Injuries and Conditions[edit | edit source]
Fractures of the tibial shaft are most likely to occur at the inferior and middle thirds, where the bone is most narrow. Fractures of the tibial plateau are often related to high-impact trauma from motor vehicle collisions or sports.[4]
Osgood-Schlatter Disease is a painful condition in adolescents in which repetitive strain of the quadriceps muscle on the tibial tuberosity leads to ossification and microavulsions.
Suddenly, when a person's foot is stuck in a hole in the ground or while landing from a jump, it causes aggressive abduction and external rotation. Initially, there will be a spiral fracture of lateral malleolus followed by the fracture of medial malleolus. Finally, in the end, there will be cutting off the posterior margin of lower end of tibia. Such type of stages are called as 1st, 2nd and 3rd degrees of Pott's fracture,[5]
References[edit | edit source]
- ↑ Teach me anatomy Tibia Available from:https://teachmeanatomy.info/lower-limb/bones/tibia/(last accessed 29.10.2020)
- ↑ 2.0 2.1 2.2 2.3 Neumann DA, Knee. In: Neumann DA, editor. Kinesiology of the musculoskeletal system: Foundations for rehabilitation. 2nd ed. St. Louis, MO: Mosby Elsevier, 2010. p520-71.
- ↑ 3.0 3.1 3.2 Neumann DA, Ankle and Foot. In: Neumann DA, editor. Kinesiology of the musculoskeletal system: Foundations for rehabilitation. 2nd ed. St. Louis, MO: Mosby Elsevier, 2010. p573-626.
- ↑ 4.0 4.1 4.2 4.3 Moore KL, Agur AM, Dalley AF. Essential Clinical Anatomy. 4th ed. Baltimore, MD: Lippincott Williams & Wilkins, 2011.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Chaurasia BD. Human Anatomy Regional and Applied Dissection and Clinical. Vol 2. CBS Publishers and Distributors Pvt Ltd, 2010