Spinal Cord Injury
Original Editor - Killian Borms,Lisa De Pelsemaeker, Boris Coessens,Cedric Cludts
Top Contributors - Kim Jackson, Rachael Lowe, Lucinda hampton, Admin, Vidya Acharya, Chrysolite Jyothi Kommu, Tarina van der Stockt and Jess Bell
Introduction[edit | edit source]
Spinal cord injury (SCI) is a debilitating neurological condition with tremendous socioeconomic impact on affected individuals and the health care system. Today, the estimated lifetime cost of an SCI patient is $2.35 million per patient. According to the National Spinal Cord Injury Statistical Center, there are 12,500 new cases of SCI each year in North America. More than 90% of SCI cases are traumatic and caused by incidences such as traffic accidents, violence, sports, or falls. The Male-to-female ratio of 2:1 for SCI, which happens more frequently in adults compared to children. Demographically, men are mostly affected during their early and late adulthood (3rd and 8th decades of life) while women are at higher risk during their adolescence (15–19 years) and 7th decade of their lives i.e. age distribution is bimodal, with a first peak involving young adults and a second peak involving adults over the age of 60. Those over 60 years of age who suffer SCI have considerably worse outcomes than younger patients their injuries usually resulting from falls and age-related bony changes[1].
Definition/Description[edit | edit source]
Spinal cord injury is defined as traumatic damage to the spinal cord or nerves at the end of the spinal canal. This affects the conduction of sensory and motor signals across the site of the lesion.
There are two types: incomplete and complete injury. [2]
- Incomplete Lesion: not all the nerves are severed or the nerves are only slightly damaged. Recovery is possible, but never to the pre-injury level.
- Complete lesion: the nerves are severed and there is no motor or sensory function preserved of this point.
Clinically Relevant Anatomy[edit | edit source]
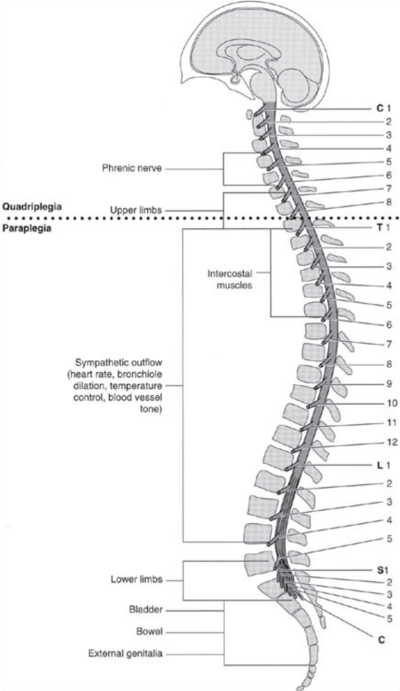
The spinal cord is the major conduit through which motor and sensory information travel between brain and body. The spinal cord contains longitudinally oriented spinal tracts (white matter) surrounding central areas (gray matter) where most spinal neuronal cell bodies are located.
The grey matter is organized into segments comprising sensory and motor neurons.Axons from spinal sensory neurons enter and axons from motor neurons leave the spinal cord via segmental nerves or roots. The roots are numbered and named according to the foramina through which they enter/exit the vertebral column. Each root receives sensory information from skin areas called dermatomes. Similarly, each root innervates a group of muscles called a myotome.
The spinal column is divided into four regions: Cervical (7 vertebrae), thoracic (12 vertebrae), lumbar (5 vertebrae), and sacral (5 vertebrae). [3]
Epidemiology/Etiology[edit | edit source]
A recent systematic review found the prevalence of Spinal Cord Injury to be dependent on the region the studies were conducted in, ranging from 906 per million in the USA up to 250 per million in Rhone-Alpes, France.[4] Annual incidence rates also varied significantly between regions, ranging from 49.1 per million in New Zealand to 8.0 per million in Spain. [4] A further review found similar results with prevalence ranging from 1298 per million to 50 per million and incidence ranging from 246 per million to 3.3 per million.[5] These results indicate that the incidence, prevalence, and causation of Spinal Cord Injury can differ significantly between developing and developed countries (high in developed countries).
Strong inconsistencies in data were noted when analyzed between countries but the most frequent causes of Spinal Cord Injury reported are, in order; [5]
- Motor Vehicle Accidents
- Falls
- Sport Injuries
- Violence
- Self-harm
- Work-related Accidents.
Data from the National Spinal Cord Injury Statistical Center (USA) 2010 - 2014 provided the following statistics for etiology (illustration). Other interesting statistics from this report include:
- Males account for 80% of new cases
- The average age at injury has gone up from 29 years old (1970) to 42 years old currently.
- Only about 12% of patients are employed 1 year after trauma, rising to 34.4% 20 years post-injury
- Life expectancy decreases for all individuals with Spinal Cord Injury, compared to those without a spinal cord injury.
Characteristics / Clinical Presentation[edit | edit source]
As spinal cord injuries are by definition caused by traumas, the primary examination and presentation will be done in an emergency response setting. Initial evaluation includes a pulmonary evaluation to determine loss of ventilatory function and/or lung injury. Signs of hemorrhage and neurogenic shock are also checked in this initial evaluation.
Finally, and most relevant to physical therapy, neurologic assessment is done which includes checking motor function, sensory evaluation, deep tendon reflexes, and perineal evaluation.[6]
The ASIA (American Spinal Injury Association) has established an international standard neurological which can be used to classify the lesion according to a specific cord syndrome. This includes motor and sensory evaluation. This also includes an impairment scale which indicates the severity of the lesion.
(for more information see article)
The clinical outcomes of SCI depend on the severity and location of the lesion and may include partial or complete loss of sensory and/or motor function below the level of injury.
- Lower thoracic lesions can cause paraplegia (Traumatic Paraplegia)
- Cervical level lesions are associated with quadriplegia.
SCI typically affects: the cervical level of the spinal cord (50%) with the single most common level affected being C5; thoracic level (35%); lumbar region (11%).
- With recent advancements in medical procedures and patient care, SCI patients often survive these traumatic injuries and live for decades after the initial injury.
- Reports on the clinical outcomes of patients who suffered SCI between 1955 and 2006 in Australia demonstrated that survival rates for those suffering from tetraplegia and paraplegia are 91.2 and 95.9%, respectively. The 40-year survival rate of these individuals was 47 and 62% for persons with tetraplegia and paraplegia, respectively.
- The life expectancy of SCI patients highly depends on the level of injury and preserved functions eg ASIA Impairment Scale (AIS) grade D, requiring a wheelchair for daily activities have an estimated 75% of a normal life expectancy; patients not requiring wheelchair and catheterization can have a higher life expectancy up to 90% of a normal individual[1].
Differential Diagnosis[edit | edit source]
- Aortic Artery Dissection
- Epidural and Subdural Infections
- Spinal Cord Infections
- Syphilis (Tertiary)
- Vertebral Fracture and here
- Transverse Myelitis
- Acute Intervertebral Disk Herniation
- Spinal Abscess
Medical Management[edit | edit source]
The ideal management of acute spinal cord injury is a combination of pharmacological therapy, early surgery, aggressive volume resuscitation, and blood pressure elevation to maximize spinal cord perfusion, early rehabilitation, and cellular therapies.[7]
Pharmacological Intervention[edit | edit source]
There is still no commonly accepted pharmacological agent.[7] The most important candidates are
Glucocorticoids (Methylprednisolone), which suppress many of the ‘secondary’ events of spinal cord injury. These are inflammation, lipid peroxidation, and excitotoxicity. Randomized clinical trials are contradictory in their results and so are the opinions of experts. [8]
Thyrotropin-releasing Hormone (TRH) shows antagonistic effects against the secondary injury mediators.[7]
For more information, see the article.
Polyunsaturated Fatty Acids (PUFA) such as Docosahexaenoic Acid (DHA) have recently been explored for spinal cord injury management. It is said to improve neurological recovery through increased neuronal and oligodendrocyte survival and decreased microglia/macrophage responses, which reduces the axonal accumulation of B-Amyloid Precursor Protein (b-APP) and increases synaptic connectivity. Similarly Eicosapentaenoic Acid (EPA) increases synaptic connectivity, to restore neuro-plasticity.[9]
Surgical Intervention[edit | edit source]
Early surgical decompression results in a better neurological outcome.
Cellular Therapy Interventions[edit | edit source]
Traumatic SCI represents heterogeneous and complex pathophysiology. While pre-clinical research on SCI has been an ongoing endeavor for over a century, our understanding of SCI mechanisms has been increased remarkably over the past few decades. This is mainly due to the development of new transgenic and preclinical animal models that has facilitated rapid discoveries in SCI mechanisms. Although SCI research has made an impressive advancement, much work is still needed to translate the gained knowledge from animal studies to clinical applications in humans.[1]
The aim of cellular therapies is to provide functional recovery of the deficit through axonal regeneration and restoration.
Schwann Cell is one of the most widely used cell types for the repair of the spinal cord.
Olfactory Ensheating Cells are capable of promoting axonal regeneration and remyelination after injury.
Bone Marrow derived Mononuclear Cells (BM-MNC’s) transplantation is feasible, safe, and has a good degree of outcome improvement.
Stimulated Macrophages invade the impaired tissue.[7]
Diagnostic Procedures[edit | edit source]
Imaging technology is an important part of the diagnostic process of acute or chronic spinal cord injuries. Spinal cord injuries can be detected using different types of imaging which depends on the type of underlying pathology.
- MRI Scans have become the golden standard for imaging neurological tissues such as the spinal cord, ligaments, discs, and other soft tissues. Only MRI sequences of sagittal T2 were found to be useful for prognosticative purposes. [10]
- Spinal fractures and bony lesions are better characterized by computed tomography (CT) and vascular injuries can be detected by using an MR angiography or by a CT scan.[11]
Outcome Measures[edit | edit source]
- Cite instrument related to ICF classification
- Instruments to measure impairments
- Instruments to measure disability
- Spinal Cord Independence Measure (SCIM)[12]
- Spinal Cord Injury Lifestyle Scale (SCILS)[13]
- WHOQOL-BREF[13]
Examination[edit | edit source]
A diagnosis can be made through a thorough history and examination. By performing a neurological examination, if possible to participate in a reliable physical neurological examination, for the sensory and motoric functions of the body in the corresponding area of complaints. After the examination, we can make a judgment of the severity and the location of the injury.[14] If the place of injury is diagnosed we can perform some extra examinations as described on the following pages:
Physical Therapy Management[edit | edit source]
The rehabilitation of patients who had a spinal cord injury depends on which level of the spine the injury occurred. Also, the therapy depends on whether it was a complete or incomplete spinal cord injury. In case of an incomplete spinal cord injury, 25% do not become independent ambulators. The therapies differ according to where the lesion happened, cervical, thoracic, or lumbar. The rehabilitation of SCI is a multidisciplinary approach! [15][16]
Possible Upper Incomplete SCI Therapy:
When the cervical spine is injured, the consequences for the patient are life-changing. Patients need therapy for movement and strength recovery of the upper body and probable respiratory training.[16][17] Respiratory muscle training consists of inspiratory, expiratory, or both improvements in muscle strength and endurance. Normocapnic hyperpnoea is a method of respiratory muscle endurance training that simultaneously trains the inspiratory and expiratory muscles. This device consists of a re-breathing bag that works at 30 to 40% of the patient’s vital capacity and is connected to a tube system and mouthpiece.[18] The patient must fill and empty the bag completely with each breath. Other respiratory muscle training exists and is also effective.[19] The study by Holmlund T et al. guides the clinician in the rehabilitation program for persons with SCI to meet required physical activity levels[20]. Spinal immobilization should be the primary focus in patients with bone or ligament injuries and the prevention of inducing spinal cord injury[21].
Training of the upper limb after SCI consists usually of specific exercises or conventional therapy using Bobath principles combined with functional electrical stimulation.[16]
Possible Lower Incomplete SCI Therapy:
The main limitations with lower incomplete SCI patients are that they have reduced coordination, leg paresis, and impaired balance.[15] These limitations can be worked on with the use of braces and tilt tables.
If the leg strength improves, therapists can use braces, parallel bars, and other walking aids to work on the balance weight-bearing of the patient. In combination with those instruments, the therapist needs to train the patient using the repetitive and intensive practice of gait.
The use of a treadmill with an overhead harness is applied to certain SCI cases and only by choice of the therapist. Thanks to the harness, patients can more easily focus on their gait under the supervision of their therapist. In addition to this therapy, the use of functional electrical stimulation is needed to optimize the rehabilitation of the patient.[15][22]
New therapies are emerging and showing positive evolution, such as robotic-assisted gait training. This therapy uses a treatment of 40 minutes twice a day at a rate of 5 times a week. 3 days using robotic-gait training and 2 days of regular physical therapy. Included in the regular physical therapy are, functional electrical stimulation and physical therapy using the Bobath principles.[15][22]
Complete recovery after incomplete or complete SCI is never attainable.[15][22][17]
Future Public Health Directions[edit | edit source]
The total number of patients living with SCI is likely to be increasing because the global population is increasing. The main causes of SCI across most geographical locations were falls and road traffic accidents, suggesting that interventions targeting fall prevention and improved road safety should be key public health priorities. Furthermore, policymakers and governments should be prepared to invest resources into centers specializing in multidisciplinary care for people with SCI, because available systems are likely to become overburdened. This may entail Infrastructural changes at a health-care-systems level to establish appropriate clinical care pathways and improve timely access to quality care[23].
Clinical Bottom Line[edit | edit source]
Spinal cord injuries are a serious, widespread health issue resulting in a large amount of disfunction and as such have a big socio-economic impact.
Therapy is multidisciplinary and the focus should be on regaining function (relevant to the patient!), as tissue recovery is often impossible.
Resources[edit | edit source]
ASIA - International Standards for Neurological Classification of SCI (ISNCSCI) Exam
http://www.asia-spinalinjury.org/elearning/isncsci_worksheet_2015_web.pdf
Article Exploring additional pharmacological options
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4303789/pdf/WJO-6-42.pdf
Website of National Spinal Cord Injury Statistical Center (NSCISC) - Accessed 18/11/2015
https://www.nscisc.uab.edu/Public/Facts%202015%20Aug.pdf
Key Research[edit | edit source]
Singh, A. et al. “Global prevalence and incidence of traumatic spinal cord injury”, Clin. Epidemiol. 2014; 6: 309-331. (level of evidence 1A)
Furlan, J.C. et al. “Global incidence and prevalence of traumatic spinal cord injury.” Can J Neurol Sci. 2013 Jul;40(4):456-64. (level of evidence = 1A)
V. Cheung et al., Methylprednisolone in the management of spinal cord injuries: Lessons from randomized, controlled trials. (level of evidence =1A)
Xiao Lu et al., effects of training on upper limb function after cervical spinal cord injury: a systematic review, clinical rehabilitation 2015, vol. 29(1) 3-13 (level of evidence = 1A)
J.C.Shin et al., effect of robotic-assisted gait training in patients with incomplete spinal cord injury, Ann Rehabil Med 2014;38(6):719-725 ( level of evidence = 1B)
Berlowitz D et al., respiratory muscle training for cervical spinal cord injury, Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No.: CD008507. DOI: 10.1002/14651858.CD008507.pub2.(level of evidence 1A)
Anthony B. et al., The Role of Magnetic Resonance Imaging in the Management of Acute Spinal Cord Injury, J Neurotrauma. 2011 Aug; 28(8): 1401–1411. (level of evidence 1B)
M R Hill et al., Quality of life instruments and definitions in individuals with spinal cord injury: a systematic review, Spinal Cord (2010) 48, 438–450 (level of evidence 1A)
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Alizadeh A, Dyck SM, Karimi-Abdolrezaee S. Traumatic spinal cord injury: an overview of pathophysiology, models and acute injury mechanisms. Frontiers in neurology. 2019;10:282.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6439316/ (last accessed 5.1.2020)
- ↑ Frederick M Maynard et al., International Standards for Neurological and Functional Classification of Spinal Cord Injury, American Spinal Injury Association, 1996
- ↑ Francisco de Assis Aquino Gondim et al., Topographic and Functional Anatomy of the Spinal Cord, Medshape, 2015
- ↑ 4.0 4.1 Singh, A. et al. “Global prevalence and incidence of traumatic spinal cord injury”, Clin. Epidemiol. 2014; 6: 309-331
- ↑ 5.0 5.1 Furlan, J.C. et al. “Global incidence and prevalence of traumatic spinal cord injury.” Can J Neurol Sci. 2013 Jul;40(4):456-64
- ↑ J.W. McDonald et al. Spinal-Cord Injury. Lancet 2002 Fed2;359(9304):417-25 (level of evidence = 5)
- ↑ 7.0 7.1 7.2 7.3 Yilmaz T., et al., Current and future medical therapeutic strategies for the functional repair of spinal cord injury, 2015, World J Orthop. 2015 Jan 18;6(1):42-55
- ↑ V. Cheung et al., Methylprednisolone in the management of spinal cord injuries: Lessons from randomized, controlled trials Surg Neurol Int. 2015; 6: 142
- ↑ W.-Y. Yu et al., Current trends in spinal cord injury repair. Eur Rev Med Pharmacol Sci 2015; 19 (18): 3340-3344
- ↑ Anthony B. et al., The Role of Magnetic Resonance Imaging in the Management of Acute Spinal Cord Injury, J Neurotrauma. 2011 Aug; 28(8): 1401–1411
- ↑ Andrew L G. et al., Advances in Imaging of Vertebral and Spinal Cord Injury, J Spinal Cord Med. 2010 Apr; 33(2): 105–116
- ↑ M. Itzkovich et al., The Spinal Cord Independence Measure (SCIM) version III: Reliability and validity in a multi-center international, Disability and Rehabilitation Volume 29, Issue 24, 2007
- ↑ 13.0 13.1 Pruitt SD. Et al., Health behavior in persons with spinal cord injury: development and initial validation of an outcome measure, Spinal Cord [1998, 36(10):724-731]
- ↑ Joost J. van M. et al., Diagnosis and Prognosis of Traumatic Spinal Cord Injury, Global Spine J. 2011 Dec; 1(1): 1–8
- ↑ 15.0 15.1 15.2 15.3 15.4 Mehrholz J et al., locomotor training for walking after spinal cord injury (review), Cochrane Database of Systematic Reviews 2012, Issue 11. Art. No.: CD006676 (level of evidence 2A)
- ↑ 16.0 16.1 16.2 Xiao Lu et al., effects of training on upper limb function after cervical spinal cord injury: a systematic review, Clinical Rehabilitation 2015, vol. 29(1) 3-13 (level of evidence = 1A)
- ↑ 17.0 17.1 Martin G et al., Medical, psychosocial and vocational aspect of disability, Athens GA, Third Edition, 2009, p. 291 ( level of evidence 2C)
- ↑ Koppers R. et al., Tube breathing as a new potential method to perform respiratory muscle training: Safety in healthy volunteers, Respiratory Medicine (2006) 100, 714-720 (level of ev-idence 2B)
- ↑ Berlowitz D et al., respiratory muscle training for cervical spinal cord injury, Cochrane Data-base of Systematic Reviews 2013, Issue 7. Art. No.: CD008507 (level of evidence 1A)
- ↑ https://scholar.google.com/scholar_url?url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6890239/&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=2874072364265094802&ei=HBQiXuaQMLGKy9YP5rKTwAg&scisig=AAGBfm3MEuyszF16bXLhYKxjk6TSjIEZoA
- ↑ Matthew J Eckert, Matthew J Martin.Trauma: Spinal Cord Injury.PMID: 28958356.DOI: 10.1016/j.suc.2017.06.008.. 2017 Oct;97(5):1031-1045.PubMed.gov. National Library of Medicine. National Centr for Biotechnology Information.
- ↑ 22.0 22.1 22.2 J.C.Shin et al., effect of robotic-assisted gait training in patients with incomplete spinal cord injury, Ann Rehabil Med 2014;38(6):719-725 ( level of evidence = 1B)
- ↑ Badhiwala JH, Wilson JR, Fehlings MG. Global burden of traumatic brain and spinal cord injury. The Lancet Neurology. 2019 Jan 1;18(1):24-5.Available from:https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(18)30444-7/fulltext (last accessed 5.1.2020)