Falls
Original Editor - Bhanu Ramaswamy as part of the AGILE Project.
Top Contributors - Andeela Hafeez, Lucinda hampton, Kim Jackson, Vidya Acharya, Lauren Lopez, Shaimaa Eldib, Tony Lowe, Rochelle Dsouza, Christina Nowak, WikiSysop, 127.0.0.1, Admin, Scott Buxton and Alan Jit Ho Mak
Introduction[edit | edit source]
A fall is defined as an incident which results in a person coming to rest accidentally on the ground or floor or other lower level. Fall-related injuries may be fatal however most are non-fatal. While all people who fall are at risk of injury, the age, gender and health of the individual can affect the type and severity of injury.
- Falls are the second leading cause of unintentional injury deaths globally. Each year worldwide: an estimated 684 000 individuals die from falls; 37.3 million falls are severe enough to require medical attention.
- Adults older than 60 years of age suffer the greatest number of fatal falls.[1]
Causes of Falls[edit | edit source]
All people who fall are at risk of injury, however, the age, gender and health of the individual can affect the type and severity of injury.
- Age is a key risk factors for falls. Older people have the highest risk of death or serious injury arising from a fall and the risk increases with age. This risk level is in part due to physical, sensory, and cognitive changes associated with ageing[2], plus environments that are not adapted for older persons. See Physical Activity in Ageing and Falls
- Gender. Both genders are at risk of falls. Older women and younger children are more prone to serious injury from falls. Globally, males consistently sustain higher death rates and DALYs lost, possibly due to males having higher levels of risk-taking behaviours and hazards within occupations.
Other risk factors include:
- Occupations at raised heights or other hazardous working conditions.
- Alcohol or substance use.
- Socioeconomic factors eg. poverty, overcrowded housing, sole parenthood, young maternal age.
- Underlying medical conditions, examples include neurological (see eg falls and traumatic brain injury, falls and dementia, orthostatic hypotension), cardiac vascular conditions (eg heart rhythm problem, persons recovering from stroke, with weakness on one side)[3] or other disabling conditions (eg see falls in amputees).[4]
- Medication side effects (see Medication and Falls)
- Sendentary lifestyle.
- Poor mobility, cognition, and vision, particularly in those in aged care facilities.
- Unsafe environments, particularly for those with poor balance and limited vision (see Eyesight in the Elderly and Ageing on the Special Senses).[1]
Intrinsic and Extrinsic Risk Factors[edit | edit source]
Fall risk factors can be classified as intrinsic and extrinsic.
- Intrinsic risk factors are traits of an individual that increase their risk of falling[5]; these are more important amongst the oldest age group and can be related to neurosensory impairment, certain drugs, or the presence of diseases associated with an increased risk of falling (e.g. Parkinson's, stroke, osteoarthritis or diabetes[4]). The risk of having a fall or recurrent falls increases with the number of associated intrinsic risk factors.
- Extrinsic causes are social and physical factors that relate to an external environment, unrelated to disease or drug use; a slip on ice for example. Falls amongst people < 75 years are more likely to be due to extrinsic factors than those aged 75 and over. If both intrinsic and extrinsic factors are present, falls are classified as combined[6][7].
Health literacy is positively correlated with gait speed. According to research, community-dwelling old adults with higher health literacy have faster gait speed.[8]
Management of Falls[edit | edit source]
The management of falls can be complicated. A combination of interventions, for example - medication review, an exercise program, vitamin D supplementation, and home assessment are recommended. As the causes of falls are often multiple, the treatment should be tailored to each patient based on the history and physical examination.[9]
Clinical practice guidelines (CPGs) are clear that all older adult should be screened for fall risk at least once per year. Balance impairment and gait and mobility limitations screening are an integral part of the fall risk screening. Fall risk screening may prompt a multifactorial risk assessment, some of it being implemented by the physical therapist in consultation with other health care providers. [10]
It is becoming increasingly recognised that falls prevention requires a change in the person’s behaviour and should be approached from a psychological, and not just a physical perspective. This is becoming the focus of health promotion[11] and it is such multidisciplinary intervention that has been proven to be of most effect for fallers. [12][13].
The physiotherapist’s role is to work with the interdisciplinary team (whether actual or virtual) and investigate possible falls causes, working holistically to address issues[14]. Management is multifactorial aiming to prevent and minimise future falls risks.
Physiotherapy Assessment[edit | edit source]
The NICE guidelines stipulates a Falls risk assessment and prevention for all those:
- People aged 65 years & older during their hospital stay.
- People aged 50-64 years who are judged by the clinician to be at a higher risk of falling because of an underlying condition.[15]
A complete Falls assessment will be part of a bigger, Interdisciplinary Multifactorial assessment which would include liaison with the Doctors, Nurses, OTs and other health care professionals. Key components of a multifactorial assessment include:
- A detailed falls history, medication review, risk factor assessment including osteoporosis and bone health, urinary incontinence and cardiovascular disease.
- Physical examination including gait and balance, neurological and cognitive function, lower limb strength, visual acuity, feet and footwear
- Functional assessment such as activities of daily living perceived functional ability and fear of falling[16].
History[edit | edit source]
The physiotherapist should be clear why they are asking specific questions and what they need to physically assess to guide their management options. A good history allows the clinician to build a picture around the falls and identify any patterns, risk factors or causes, leading to a possible explanation or clinical diagnosis. Physiotherapists are well-placed to lead a falls assessment as other professionals (whether qualified and unqualified, of a health or social care background) may have completed only a falls ‘screen’ rather than a full multi-factorial falls risk assessment.
A thorough physiotherapy assessment might identify additional cause(s) of falls not previously known that might be addressed. To include falls and near misses (also indicators of falls risk), it is recommended to pose the question using the following wording: “In the past month, have you had any fall, including a slip or trip in which you lost your balance and landed on the floor or ground or lower level?”[17]
Physical Examination[edit | edit source]
The physical examination should include assessment of gait, balance, joint range of movement and muscle strength. It is recommended that validated assessment tools are used. Outcome measures such as the Timed Up and Go Test or Berg Balance Scale can be found here on Physiopedia or via an evidenced-based health database.
A fall or potential fall event should be assessed through multi-factorial tools such as the Physiological Profile Assessment (PPA). This screening procedure evaluates an older person’s likelihood of falling[6]. It involves a comprehensive series of simple tests of vision, peripheral sensation, muscle force, reaction time, and postural sway that can be administered quickly with portable equipment. The results can differentiate people at risk of falls (“fallers”) from people less at risk (“non-fallers”) as the tests identify specific contributions of the visual, vestibular, proprioceptive, and musculoskeletal systems to create a ‘balance profile’. The research shows the difference between instability produced by failing strength, decreased leg sensitivity (e.g. from diabetes), visual problems (e.g. glaucoma), and other issues.
Functional Ability[edit | edit source]
Functional ability can be reviewed through subjective questioning of how a person manages personal and domestic activities of daily living; or observation of how the person performs everyday tasks such as standing up from a chair or multi-tasking e.g. walk and carry objects. Poor response in a dual-task setting is a possible prognostic value for multiple falls[18].
Apart from the financial costs to the health system falling can have a major impact on a person's lifestyle as well as that of their family[6]. Psychological and physical consequences of falling include loss of confidence, activity restriction, social interaction and an increased dependency on carers that can cause family or carer strain[6][19][20]. A scale such as the Falls Efficacy Scale International (FES-I) developed through ProFaNE (See Further Reading section below) might be used to determine a patient’s confidence when performing activities. It can highlight when the fear of falling may be preventing activity and therefore needs addressing.
Physiotherapy[edit | edit source]
Exercise, including structured physical therapy, is an effective component of a fall prevention program, and the physical therapist also may directly provide home hazard and footwear modification and education about fall risk.
Four main physiotherapy goals have been identified when working with older fallers[21].
- Prevention of further falls by working on mobility, balance and strength (the most effective intervention)
- Training clients to cope with further falls and minimise the consequences of a long lie. Also teach clients how to get off the floor or to call for help, and keep warm in the meantime.
- Ensuring their living environment is as safe as possible.
- Restoration of confidence and self-esteem to improve their quality of life.
Physiotherapy Interventions[edit | edit source]
Exercise (for strength and balance) has been shown to have the most effective outcomes in reduction of falls rates[22]. As the majority of people who attend balance programmes relapse into old ways by six months, the physiotherapist should attempt to reinforce and encourage adherence to their home exercise program.
For examples of Physiotherapy Interventions see:
- Inoculation Against Falls: Balance Intervention Strategies
- Reactive Balance Training
- Otago Exercise Programme
- Backward-chaining
- Tai Chi and the Older Person
Sherrington et al’s research[22] demonstrated these factors:
- The balance training needs to be highly challenging and should be individualised & progressive
- Exercise should be at least twice a week and for a minimum duration of 6 months.
- Walking should only be prescribed in addition to a high intensity / high dose programme
- People in sub-acute hospital inpatients settings could benefit from a multi-factorial intervention – particularly those at high risk of falls if the fall was related to postural instability. The person had to be able to participate in a 45 minutes group exercise session at least 3 x week for the duration of their stay.
Prevention[edit | edit source]
The scope for prevention can be appreciated by considering some of the common conditions and risk factors predisposing to falls in the elderly. From this, the wide range of preventative measures and treatment possibilities can be appreciated. Falls should be considered a symptom rather than a diagnosis so that when a patient, usually an elderly person, presents with a history of falls, effort should be made to find the cause or causes[23].
Strategies to prevent falls occurring[24]:
- Exercise regularly. It is important that the exercises focus on increasing leg strength and improving balance, and that they get more challenging over time. Tai Chi programs are especially good. Also, according to the systematic review, prevention-focused unimodal exercise programs that incorporate only strength training approach seems as effective as alternative unimodal (Tai-chi, stretching) or multimodal exercise programs(balance + tone training or balance + strength training) in tackling the risk of falls in older adults. Thus findings suggest that the implementation of supervised strength training might be a time-efficient exercise strategy to prevent falls in older adults. [25]
- Ask their doctor or pharmacist to review their medicines—both prescription and over-the-counter—to identify medicines that may cause side effects or interactions such as dizziness or drowsiness. Vitamin D supplementation and psychoactive drug withdrawal are also effective[16]. The recent study suggests that implementing a fall treatment protocol comprised of a multidisciplinary team of a Family Medicine (FM) physician, an Internal Medicine (IM) physician, a Physical Therapist, and a Home Health (HH) nurse leads to more consistent care of elderly patients who experience falls. However, there is a need for reviewing and updating the protocol based on outcomes, and subsequent research is required for improvement in patient care[26].
- Have their eyes checked by an eye doctor at least once a year and update their eyeglasses to maximise their vision. Consider getting a pair with single vision distance lenses for some activities such as walking outside.
- Make their homes safer by reducing tripping hazards, adding grab bars inside and outside the tub or shower and next to the toilet, adding railings on both sides of stairways, and improving the lighting in their homes.
Further Reading[edit | edit source]
- Lord S, Sherrington C, Menz H, Close J. Falls in Older People: risk factors and strategies for prevention. Second Edition. New York: Cambridge University Press, 2007.
- NICE(2013) Falls in older people: assessing risk and prevention.
- Department of Health UK. Prevention Package for Older People.
- The ProFaNE network (of 25 partners) focuses on the issue of prevention of falls and improvement of postural stability amongst elderly people across Europe.
- The Falls and Balance Research Group based in New South Wales, Australia are leading the field of applied research examining different factors that contribute to older people falling and experimental interventions to decrease the contribution of any single factor.
- The Postural Stability Instructor Course for Laterlife Training: http://www.laterlifetraining.co.uk/page5.html
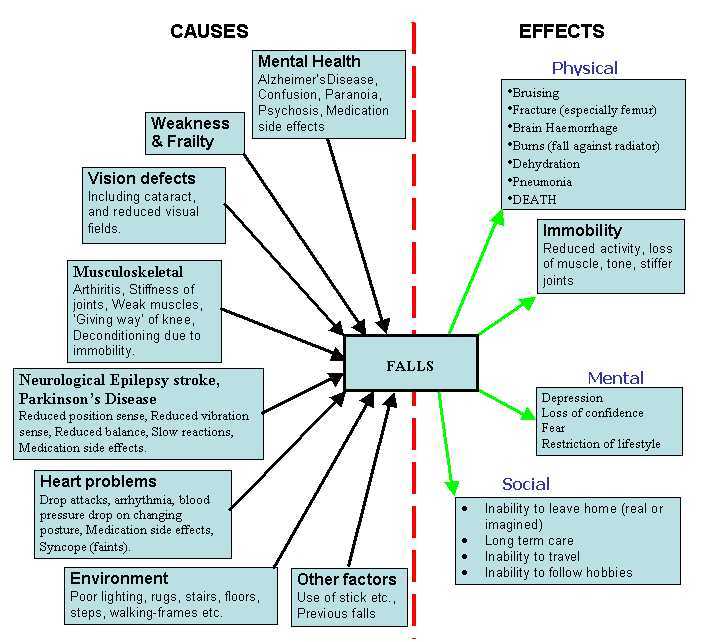
Falls factors[edit | edit source]
Many things causes and effects exist as shown below.
Falls Factors (from the UK Department of Work and Pensions site)
Resources[edit | edit source]
Falls Efficacy Scale - International (FES-I) - Outcome Measure
References[edit | edit source]
- ↑ 1.0 1.1 WHO Falls Available:https://www.who.int/news-room/fact-sheets/detail/falls (accessed 3.11.2022)
- ↑ Tsujishita S, Nagamatsu M, Sanada K. Overlap of Physical, Cognitive, and Social Frailty Affects Ikigai in Community-Dwelling Japanese Older Adults. InHealthcare 2022 Nov 4 (Vol. 10, No. 11, p. 2216). MDPI.
- ↑ Heart org Falls can be a serious, poorly understood threat to people with heart disease Available:https://www.heart.org/en/news/2022/05/19/falls-can-be-a-serious-poorly-understood-threat-to-people-with-heart-disease (accessed 3.11.2022)
- ↑ 4.0 4.1 Wu X, Guo J, Chen X, Han P, Huang L, Peng Y, Zhou X, Huang J, Wei C, Zheng Y, Zhang Z. Comparison of the relationship between cognitive function and future falls in Chinese community-dwelling older adults with and without diabetes mellitus. Journal of the Formosan Medical Association. 2022 Nov 3.
- ↑ Smith M. Medication & The Risk of Falls in the Older Person: The Facts. Produced on behalf of WAM Falls in Elderly Steering Group. 2004.
- ↑ 6.0 6.1 6.2 6.3 Lord S, Sherrington C, Menz H, Close J. Falls in older people – Risk Factors and strategies for prevention. 2nd edition. Cambridge: Cambridge University Press, 2007.
- ↑ Formiga F, Soto A, Duaso E, Chivite D, Ruiz D, Perez-Castejon J. Letter to the Editor in: Bone; 40 (1); 242. Re: “Incidence and characteristics of falls leading to hip fracture in Iranian population” by Abolhassani et al. BONE 2006:39;408–13.
- ↑ Anami K, Murata S, Nakano H, Nonaka K, Iwase H, Shiraiwa K, Abiko T, Goda A, Horie J. The Association between Health Literacy and Gait Speed in Community-Dwelling Older Adults. InHealthcare 2020 Dec (Vol. 8, No. 4, p. 369). Multidisciplinary Digital Publishing Institute.
- ↑ Appeadu MK, Bordoni B. Falls and fall prevention in the elderly. InStatPearls [Internet] 2022 Feb 22. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK560761/ (accessed 8.11.2022)
- ↑ Avin KG, Hanke TA, Kirk-Sanchez N, McDonough CM, Shubert TE, Hardage J, Hartley G. Management of falls in community-dwelling older adults: clinical guidance statement from the Academy of Geriatric Physical Therapy of the American Physical Therapy Association. Physical therapy. 2015 Jun 1;95(6):815-34.Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4757637/ (accessed 4.11.2022)
- ↑ Benedetto V, Hill J, Harrison J. Cost effectiveness of fall prevention programmes for older adults. British Journal of Community Nursing. 2022 Nov 2;27(11):530-3.
- ↑ National Institute for Health and Clinical Excellence. 2004. CG21: Falls. Accessed from www.nice.org.uk
- ↑ Cameron ID, Gillespie LD, Robertson M, Murray GR, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in care facilities and hospitals (Cochrane review). Cochrane Database Syst Rev 2012: (12): CD005465.
- ↑ Squires A, Hastings M, editors. Rehabilitation of Older People: A handbook for the interdisciplinary team. 3rd edition. Cheltenham: Nelson Thornes, 2000.
- ↑ National Institute for Health and Care Excellence.Falls in older people: assessing risk and prevention. Clinical guideline [CG161]. Published:12 June 2013.
- ↑ 16.0 16.1 Waldron N, Hill A, Barker A. Falls prevention in older adults: assessment and management. Aust Fam Physician. 2012; 41(12): 930-935. Accessed 28 September 2018.
- ↑ Lamb S. Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe Consensus. JAGS 2005; 53 (9); 161-22.
- ↑ Faulkner K, Redfern M, Cauley J (2007). Multitasking: association between poorer performance and a history of recurrent falls: a brief report. J Am Geriatr Soc. 2007; 55(4): 570-576.
- ↑ Elliott T, Pezent G. Family caregivers of older persons in rehabilitation. NeuroRehabilitation. 2008; 23 (5): 439–446.
- ↑ Martin F, Husk J, Foster N, Ballinger C, Spencer-Williams M. Patient and public involvement older people’s experiences of falls and bone health services (England). RCP: London, 2008.
- ↑ AGILE. Guidelines for collaborative management of elderly people who have fallen. CSP and College of Occupational Therapist. London, 1998.
- ↑ 22.0 22.1 Sherrington C, Whitney J, Lord S, Herbert R, Cumming R, Close J. Effective exercise for the prevention of falls: A systematic review and meta-analysis. J Am Geriatr Soc. 2008; 56 (12): 2234 - 43.
- ↑ Tidy C, Knott L. Prevention of Falls in the Elderly. 2016. Available at https://patient.info/doctor/prevention-of-falls-in-the-elderly-pro. (accessed 28 September 2018).
- ↑ Centers for Disease Control and Prevention. Available at https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html (accessed 28 September 2018).
- ↑ Claudino JG, Afonso J, Sarvestan J, Lanza MB, Pennone J, Serrão JC, Espregueira-Mendes J, Vasconcelos AL, de Andrade MP, Rocha-Rodrigues S, Andrade R. Strength training to prevent falls in older adults: a systematic review with meta-analysis of randomized controlled trials. Journal of clinical medicine. 2021 Jan;10(14):3184.
- ↑ Cicerone KD, Langenbahn DM, Braden C, Malec JF, Kalmar K, Fraas M, Felicetti T, Laatsch L, Harley JP, Bergquist T, Azulay J. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Archives of physical medicine and rehabilitation. 2011 Apr 1;92(4):519-30.