Orthostatic Hypotension
Definition[edit | edit source]
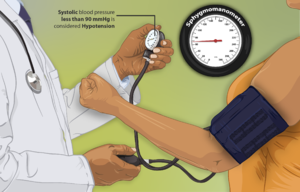
Orthostatic hypotension (OH) is defined as a sudden drop in blood pressure upon standing from a sitting or supine position. It is also known as postural hypotension.
- Diagnosis is made if the blood pressure drops by or greater 20mmHg systolically and 10mmHg diastolically. This occurs within three minutes of standing after being supine for 5 minutes or at 60% angle on a tilt table[1]. This sudden drop in blood pressure is due to failure of autonomic reflex, volume depletion, or adverse reaction to medication.
- Symptoms on presentation are commonly related to reduced blood flow to the brain but many patients can be asymptomatic. Frequent falls occur due to this disease process resulting in a high rate of morbitity and mortality and multiple hospital admissions.[2]
Watch this informative 4 minute viewing.
Etiology[edit | edit source]
Orthostatic hypotension etiology causes include:
- Medication related: a common causes of OH. High risk medications include cardiovascular drugs (e.g., diuretics, nitrates, β- and α-receptor blockers), non-cardiovascular drugs (e.g., antidepressants, antipsychotics, trazodone, and BDZs), and polypharmacy.[4]
- Non-neurogenic causes of the condition include: Heart attack; Aortic stenosis; Vasodilation; Volume depletion (eg Dehydration, Hyperglycemia, Hemorrhage, Vomiting)[5].[2]
- Neurogenic eg Parkinson's disease, Diabetic nerve damage, Lewy body disease 9one of the most common causes of dementia in older adults), Postural Orthostatic Tachycardia Syndrome (POTS), Vasovagal syncope, Postprandial hypotension See 5 minute video clip below.
Epidemiolgy[edit | edit source]
Prevalence varies with age: In those <50 OH occurs 5% in patients, whilst those >70 years of age prevalence is 30%.[7]
Signs and Symptoms[edit | edit source]
The person will present with symptoms occurring when rise from standing or sitting, particularly if done rapidly. The related signs and symptoms are due to reduced cerebral blood flow. These include: lightheadedness; generalised tiredness; vertigo; blurred vision; difficulty concentrating; palpitations; anxiety; nausea; falls.[8]
Diagnostic Procedures[edit | edit source]
Take the BP
- 5 minutes after lying
- 1 minute after standing
- 3 minutes after standing
A drop in systolic BP of 20mmHg or greater, a drop in systolic BP of 10mmHg or greater is diagnostic tool[8].
Outcome Measures[edit | edit source]
Doing BP measures again as in initial diagnosis.
Management / Interventions[edit | edit source]
Apart from removing any offending medications the initial line of management are lifestyle related. These include:
- Drinking 2-3 litres of water, in small boluses over the day.
- Use of compression stockings and corsets when out.
- Exercising major muscle groups eg static gluteals just before standing or on standing
- Counting a slow 10 before moving on from sit to stand position
- Increasing salt intake or salt supplements.
- Elevating bed head at night to decrease fluid to kidneys with resultant urine production and fluid loss[8]
- Exercise, for cases caused by a weakened cardiovascular system[5].
Pharmacologic treatment should be implemented after lifestyle interventions have failed to relieve symptoms. Medications that work through different mechanisms in order to increase vascular tone are utilised. These include fludrocortisone and midodrine which are the first-line medications, but many other pharmacologic therapies can be used, including pyridostigmine.[2]
Physiotherapy[edit | edit source]
During a PT session, it will be important to monitor a patient's BP before, during, and after exercise. It will also be necessary to choose appropriate exercises and environment to avoid these symptoms from occurring
- Falls prevention training. OH is positively associated with a greater falls risk.[10] Parkinson's clients have a 40-60% chance of having OH and hence a significant increase in falls risk.[11]
- Compression garments. Measuring and fitting of appropriate garments and teaching in the fitting of these with aids eg stocking donner.
- Lifestyle strategies. As physiotherapists often are in regular contact with there clients take the time to consul on eg fluid and salt intake; use of bed head raisers; exercises to increase venous return on standing or just prior eg calf pumps, static quads or gluteals; avoiding standing for prolonged periods; not going out in hot sun or stuffy environments; small regular meals to prevent post prandial OH. Advising the patient to refrain from quick postural changes.[12]
- Education. Movement changes eg sit on edge of bed for 30 seconds before rising, count 10 once standing before moving off, rise slowly and wait 10 seconds if out in sun, fluid intake checks and taking water when going out. Swimming/aquatherapy could be suggested, as the hydrostatic pressure of the water counteracts the hypotension the patient is experiencing.[12]
Implications of OH[edit | edit source]
The importance of treating OH is many fold
- Dementia risk in increased by having OH[13]
- Orthostatic hypotension is associated with a significantly increased risk of all-cause death, incident CAD, HF, and stroke.[14]
- A increased risk of falls
- An impaired quality of life[2]
References[edit | edit source]
- ↑ Schatz IJ, Bannister R, Freeman RL, Jankovic J, Koller WC, Low PA, Mathias CJ, Polinsky RJ, Quinn NP, Robertson D, Streeten DH. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multiple system atrophy. Clinical Autonomic Research. 1996;6(2):125-6. Available:https://pubmed.ncbi.nlm.nih.gov/8628505/ (accessed 16.9.2023)
- ↑ 2.0 2.1 2.2 2.3 Ringer M, Lappin SL. Orthostatic Hypotension. InStatPearls [Internet] 2017 Oct 4. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448192/ (last accessed 1.4.2019)
- ↑ Health Link. Dizziness : what is orthostatic hypotension?. Available from: https://www.youtube.com/watch?v=_N8iwBn9u2s (last accessed 11.4.2022)
- ↑ Rivasi G, Rafanelli M, Mossello E, Brignole M, Ungar A. Drug-related orthostatic hypotension: beyond anti-hypertensive medications. Drugs & Aging. 2020 Oct;37:725-38. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7524811/ (accessed 16.9.2023)
- ↑ 5.0 5.1 very well health Orthotatic hypotension Available: https://www.verywellhealth.com/postural-hypotension-1764028 (accessed 11.4.2022)
- ↑ TreatneurogenicOHnow. Neurogenic orthostatic hypotension. Available from: https://www.youtube.com/watch?v=6LcX7fGaUe0&t=215s (last accessed 1.4.2019)
- ↑ Ricci F, De Caterina R, Fedorowski A. Orthostatic hypotension: epidemiology, prognosis, and treatment. Journal of the American College of Cardiology. 2015 Aug 18;66(7):848-60.Available:https://www.sciencedirect.com/science/article/pii/S073510971503939X?via%3Dihub (accessed 16.9.2023)
- ↑ 8.0 8.1 8.2 Wikipedia. Orthostatic hypotension. Available from: https://en.wikipedia.org/wiki/Orthostatic_hypotension (last accessed 2.4.2019)
- ↑ Top doctors UK. How you can increase your BP. Available from: https://www.youtube.com/watch?v=s7YcptyqYrQ&app=desktop (last accessed 2.4.2019)
- ↑ Mol A, Hoang PT, Sharmin S, Reijnierse EM, van Wezel RJ, Meskers CG, Maier AB. Orthostatic hypotension and falls in older adults: a systematic review and meta-analysis. Journal of the American Medical Directors Association. 2018 Dec 21. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30583909/ (last accessed 2.4.2019)
- ↑ Isaacson SH, Skettini J. Neurogenic orthostatic hypotension in Parkinson’s disease: evaluation, management, and emerging role of droxidopa. Vascular health and risk management. 2014;10:169. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3979788/ (last accessed 2.4.2019)
- ↑ 12.0 12.1 Swan L, Dupont J. Multiple system atrophy. Physical therapy. 1999 May 1;79(5):488-94.Available:https://pubmed.ncbi.nlm.nih.gov/10331752/ (accessed 16.9.2023)
- ↑ Cardiology advisor. OH may increase risk for dementia. Available from: https://www.thecardiologyadvisor.com/home/topics/hypertension/orthostatic-hypotension-may-increase-risk-for-dementia/ (last accessed 2.4.2019)
- ↑ Ricci F, Fedorowski A, Radico F, Romanello M, Tatasciore A, Di Nicola M, Zimarino M, De Caterina R. Cardiovascular morbidity and mortality related to orthostatic hypotension: a meta-analysis of prospective observational studies. European heart journal. 2015 Jul 1;36(25):1609-17.Available: https://academic.oup.com/eurheartj/article/36/25/1609/2293316?login=false(accessed 16.9.2023)