Vitamin D Deficiency
Original Editors -Nicole Hess & Shannon McMullen from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Nicole Hess, Shannon McMullen, Lucinda hampton, Admin, Elaine Lonnemann, Kim Jackson, Vidya Acharya, WikiSysop and Wendy WalkerIntroduction[edit | edit source]
Vitamin D is a fat-soluble vitamin the body requires for normal bone development and maintenance (fat soluble vitamins, when in excess, are stored in the liver and fatty tissues for future use). Vitamin D is obtained from sun exposure, food, and supplements.
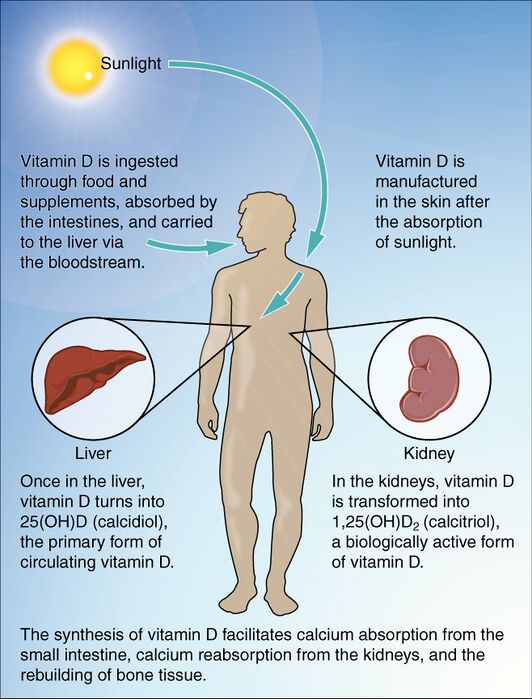
- Vitamin D is synthesized in the body when cholesterol activates with UVB rays from sunlight. When ingested, the intestines absorb the vitamin and send it to the liver and kidneys for further processing.[1] [2]
- Vitamin D deficiency can lead to an array of problems, most notably rickets in children and osteoporosis in adults[3].
- Vitamin D deficiency is a major public health problem worldwide in all age groups causing adverse effects on bone health and other health consequences. [4]
This infographic shows the steps in the synthesis of vitamin D.
Why Do We Need Vitamin D[edit | edit source]
Vitamin D is important to humans for various reasons:
- Aids our intestines to absorb calcium, essential for bones health
- Regulates the hormone insulin
- Supports the functioning of the body’s immune system.
- Help the body fight against cancer cells
- Helps in the correct heart and brain functioning
- Regulates blood pressure.[5]
Epidemiology[edit | edit source]
Vitamin D deficiency is a worldwide health issue. Roughly 1 billion people globally have vitamin D deficiency, and strikingly 50% of the world population has vitamin D insufficiency.[3]
Patients with vitamin D deficiency most at risk are the: elderly; obese; nursing home residents; hospitalized patients.[3]
Etiology[edit | edit source]
Vitamin D deficiency can result from 4 main causes:
- Decreased dietary intake and/or absorption. eg those with gastric disorders, chronic pancreatic insufficiency, cystic fibrosis and the elderly.[3]
- Decreased sun exposure eg hospitalized, nursing home residents, liberal use always of sunscreen, dark skinned people who have more melanin, which naturally protects us from the UV rays of the sun and hence limits vitamin D synthesis.[5]
- Decreased endogenous synthesis. eg people with chronic liver disease
- Those on medications that increase kidney catabolism (eg phenobarbital, spironolactone, clotrimazole, rifampin).[3]
Characteristics/Clinical Presentation[edit | edit source]
Most patients with vitamin D deficiency are asymptomatic.
- With prolonged and severe vitamin D deficiency symptoms may include: Associated effects of secondary hyperparathyroidism (bone pain, arthralgias, myalgias, fatigue, muscle twitching, and weakness); fragility fractures and osteoporosis.[3]
- Children typically present with rickets as their diagnosis. Symptoms may include irritability, lethargy, developmental delay, bone changes, or fractures ,[2]
Associated Co-morbidities[edit | edit source]
- Osteoporosis: The hormone 7-dehydrocholesterol (photochemically converted to vitamin D₃ in the skin) decreases in the skin as a person ages. By age 65, approximately only 25% of it remains in the body, leading to decreased synthesis of vitamin D and therefore calcium absorption.[2]
- Skeletal Deformities: In children with rickets there is often bowing of the long bones and widening, fraying, and clubbing near epiphyseal (growth) plates. Predominant areas include metaphysis of the long bones and sterna ends of the ribs, which is also known as rachitic rosary.[2]
- Electrolyte Imbalance: Often associated with hypomagnesemia[2]
- Hyperparathyroidism: Parathyroid hormone (PTH) is a key hormone that regulates renal synthesis of calcidiol or 25(OH)D, which therefore maintains calcium ions in the blood. Low levels of vitamin D (calcidiol) and calcium ions in the blood stimulate the PTH. Through this mechanism, the active vitamin D metabolite [1,25(OH)2D], also known as calcitriol, promotes calcium supply to the bloodstream. As the cascade progresses, parathyroid is overstimulated, causing secondary hyperparathyroidism.[6][7]
- Vitamin D deficiency negatively affects the immune system eg. Vitamin D is known to suppress the T cells that promote inflammation and stimulate the T cells that reduce inflammation; aide production of antimicrobial peptides that kill pathogens like bacteria, fungi, or viruses, and even cancer cells). This reduced immune effect can lead to conditions such as heart diseases and cancer.[5]
- Other potential comorbidities: Diabetes (type I and II), Insulin Intolerance, Hypertension, Multiple Sclerosis (MS), and decreased cognition as seen in Alzheimer’s disease[1][8]
Treatment[edit | edit source]
Replacement of vitamin D needs to be tailored for each patient and depends on the severity of the deficiency.
- A 2023 concensus statement recommended that vitamin D supplementation, combined with calcium, should be presecribed for the elderly population to lessen the burden of fractures (aiming for a serum level of vitamin D of 25(OH)D >50 nmol/l) Low dose regimes should be instituted as they reduce the risk of falls and fractures efficiently as opposed dose vitamin D regimens to infrequent, large bolus doses that may increase falls risk.[9]
- High-risk populations include nursing home residents, elderly patients, women with osteoporosis, African American/Hispanic individuals, hospitalized patients, patients with chronic kidney disease, chronic liver disease, and patients with malabsorption syndromes.[3]
Prevention[edit | edit source]
Research advice that 5–30 min of sun exposure (to the face, arms, hands, and legs, without sunscreen), especially between 10 AM and 4 PM daily or at least twice a week, usually leads to sufficient vitamin D synthesis. Proper sun exposure[1]:
- Cloud coverage can decrease absorption by as much as 50%
- Sun through windows is inadequate-Glass blocks the synthesis process
- Sunscreen may block synthesis if over the entire body
- Best exposure spots: face, arms, legs, and back
- Limit sun exposure without sunscreen to decrease risk of fatal cancers
Taking vitamin D supplements is a common method to correct vitamin D deficiency. Seek medical advice re correct dosage and medication.
- A daily intake of 1,000 IU (international units, or 25 mcg) of vitamin D3 is generally recommended to maintain an optimal level of this vitamin in the body.
- Adverse Effects: Too much vitamin D is harmful and can cause hypercalcemia (excess of calcium in human body) which in turn can lead to nausea and vomiting.[5]
Physical Therapy Management[edit | edit source]
Physical therapists can take a team approach with medical management through patient education on:
- Foods high in vitamin D
- Importance of following medical recommendations for vitamin D intake
- Importance of proper sun exposure with risks of overexposure. [10][10].
There are no direct physical therapy interventions for vitamin D deficiency. Patient will be referred to physical therapy for treatment of impairments that may be a cause of vitamin D deficiency such as decline in muscle strength, decline in physical functioning, or falls prevention. In these instances techniques could include:
- Falls prevention training eg Otago program, and falls exercise classes
- General muscle strengthening exercises. In older adults, there is a blunted responsiveness to resistance training and reduced muscle hypertrophy compared with younger adults. There is evidence that both exercise training and vitamin D supplementation may benefit musculoskeletal health in older adults, and combination their effects may be additive.[11] [12]
Vitamin D: Adequate Sources of Intake[edit | edit source]
- D2 (ergocalciferol) is found in vegetable sources and oral supplements
- D3 (cholecalciferol) is obtained primarily from skin exposure to ultraviolet B (UVB) radiation in sunlight, ingestion of food sources such as oily fish and variably fortified foods (milk, juices, margarines, yogurts, cereals, and soy), and oral supplements
Most foods contain between 50 and 200 IU per serving, which varies depending on geographical location and use of th fortification process [13]
| Food | IUs per Serving* | Percent DV** |
| Cod liver oil, 1 tablespoon | 1,360 | 340 |
| Swordfish, cooked, 3 ounces | 566 | 142 |
| Salmon (sockeye), cooked, 3 ounces | 447 | 112 |
| Tuna fish, canned in water, drained, 3 ounces | 154 | 39 |
| Orange juice fortified with vitamin D, 1 cup | 137 | 34 |
| Milk, nonfat, reduced fat, and whole, vitamin D fortified, 1 cup | 115-124 | 29-31 |
| Yogurt, fortified with 20% of the DV of vitamin D, 6 ounces | 80 | 20 |
| Margarine, fortified, 1 tablespoon | 60 | 15 |
| Sardines, canned in oil, drained, 2 sardines | 46 | 12 |
| Liver, beef, cooked, 3 ounces | 42 | 11 |
| Egg, 1 large (vitamin D found in yolk) | 41 | 10 |
| Cheese, Swiss, 1 ounce | 6 | 2 |
IUs= International Units
DV= Daily Values developed by U.S. Food and Drug Administration
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Office of Dietary Supplements National Institutes of Health. Dietary Supplement Fact Sheet: Vitamin D. Available at: http://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#ref. Accessibility verified March 28, 2013.
- ↑ 2.0 2.1 2.2 2.3 2.4 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. Missouri: Saunders Elsevier; 2009.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Sizar O, Khare S, Goyal A, Bansal P, Givler A. Vitamin D deficiency. InStatPearls [Internet] 2021 Jul 21. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK532266/ (accessed 4.1.2022)
- ↑ Palacios C, Gonzalez L. Is vitamin D deficiency a major global public health problem?. The Journal of steroid biochemistry and molecular biology. 2014 Oct 1;144:138-45. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4018438/ (last accessed 3.12.2019)
- ↑ 5.0 5.1 5.2 5.3 Harshini Rajendran et al Vitamin D: How the “Sunshine Vitamin” Affects Our Health Available:https://kids.frontiersin.org/articles/10.3389/frym.2022.763513 (accessed 4.1.2022)
- ↑ Malone R, Kessenich C. Vitamin D deficiency: implications across the lifespan. Journal For Nurse Practitioners [serial on the Internet]. (2008, June), [cited April 2, 2013]; 4(6): 448-454. Available from: CINAHL
- ↑ Prentice A. Vitamin D deficiency: a global perspective. Nutrition Reviews [serial on the Internet]. (2008, Oct 2), [cited March 29, 2013]; 66S153-S164. Available from: SPORTDiscus with Full Text.
- ↑ Kulie T, Groff A, Redmer J, Hounshell J, Schrager S. Vitamin D: an evidence-based review. Journal Of The American Board Of Family Medicine: JABFM [serial on the Internet]. (2009, Nov), [cited April 2, 2013]; 22(6): 698-706. Available from: MEDLINE.
- ↑ Giustina A, Bouillon R, Dawson-Hughes B, Ebeling PR, Lazaretti-Castro M, Lips P, Marcocci C, Bilezikian JP. Vitamin D in the older population: a consensus statement. Endocrine. 2023 Jan;79(1):31-44.Available:https://pubmed.ncbi.nlm.nih.gov/36287374/ (accessed 21.8.2023)
- ↑ 10.0 10.1 Harbison AJ, Prabhu S. Causation and Treatment Algorithms for Elderly Patients who have Fallen in the Twin Tiers.
- ↑ Antoniak AE, Greig CA. The effect of combined resistance exercise training and vitamin D3 supplementation on musculoskeletal health and function in older adults: a systematic review and meta-analysis. BMJ open. 2017 Jul 1;7(7):e014619. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28729308 (last accessed 3.12.2019)
- ↑ Aspell N, Laird E, Healy M, Lawlor B, O'Sullivan M. Vitamin D Deficiency Is Associated With Impaired Muscle Strength And Physical Performance In Community-Dwelling Older Adults: Findings From The English Longitudinal Study Of Ageing. Clinical interventions in aging. 2019;14:1751. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31686797 (last accessed 3.12.2019)
- ↑ Kennel KA, Drake MT, Hurley DL. Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc. 2010;85:752–757. quiz 757-8.