Ankle Joint
Original Editor - Naomi O'Reilly
Lead Editors - Naomi O'Reilly, Kim Jackson, Lucinda hampton, Joanne Garvey, Ewa Jaraczewska, Rachael Lowe, Admin, WikiSysop, Simisola Ajeyalemi, Vidya Acharya, Jess Bell, Khloud Shreif, Kirenga Bamurange Liliane, Olajumoke Ogunleye, Sona Eyobe, Evan Thomas, Oyemi Sillo, Tarina van der Stockt and Rucha Gadgil
Description[edit | edit source]
The ankle joint is a hinged synovial joint that is formed by the articulation of the talus, tibia, and fibula bones. Together, the three borders (listed below) form the ankle mortise.
- The articular facet of the lateral malleolus (bony prominence on the lower fibula) forms the lateral border of the ankle joint
- The articular facet of the medial malleolus (bony prominence on the lower tibia) forms the medial border of the joint
- The superior portion of the ankle joint forms from the inferior articular surface of the tibia and the superior margin of the talus.
The talus articulates inferiorly with the calcaneus and anteriorly with the navicular.
- The upper surface, called the trochlear surface, is somewhat cylindrical and allows for dorsiflexion and plantarflexion of the ankle.
- The talus is wider anteriorly and more narrow posteriorly.
- It forms a wedge that fits between the medial and lateral malleoli making dorsiflexion the most stable position for the ankle.[1]
Anatomy[edit | edit source]
This 7-minute video is a good summary of the ankle.
Structure and Function[edit | edit source]
- The ankle joint is important during ambulation because it adapts to the surface on which one walks.
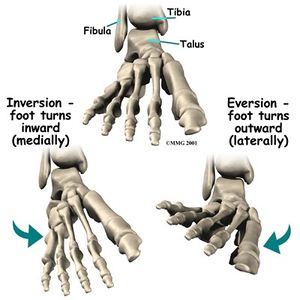
- The movements that occur at the ankle joint are plantar flexion, dorsiflexion, inversion, and eversion.
- The muscles of the leg divide into anterior, posterior, and lateral compartments. [1]
Articulating Surfaces[edit | edit source]
- Trochlea of Talus
- Malleolar Mortise formed by Tibia & Fibula
- Lateral & Medial Malleolus
Joint Capsule[edit | edit source]
The articular capsule surrounds the joints, and is attached, above, to the borders of the articular surfaces of the tibia and malleoli, and below, to the talus around its upper articular surface.
The joint capsule anteriorly is a broad, thin, fibrous layer. Posteriorly, the fibres are thin and run mainly transversely, blending with the transverse ligament. Laterally the capsule is thickened and attaches to the hollow on the medial surface of the lateral malleolus. The synovial membrane extends superiorly between Tibia & Fibula as far as the Interosseous Tibiofibular Ligament.[3]
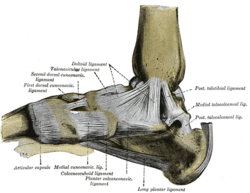
Ligaments[edit | edit source]
The main stabilizing ligaments are deltoid ligament medially, anterior, posterior talofibular and calcaneofibular ligament laterally.
Medial Ligament[edit | edit source]
The deltoid ligament, consists of four ligaments that form a triangle connecting the tibia to the navicular, the calcaneus, and the talus. It stabilises the ankle joint during eversion of the foot and prevents subluxation of the ankle joint. [3]
- The anterior and posterior tibiotalar ligaments connect the tibia to the talus.
- The tibionavicular ligament which attaches to the navicular anteriorly and the tibiocalcaneal ligament which attaches to the calcaneus inferiorly
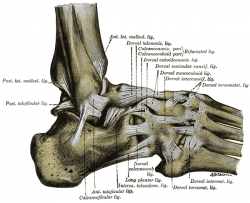
Lateral Ligament[edit | edit source]
Laterally the ankle has stabilization from three separate ligaments, the anterior and posterior talofibular ligaments, and the calcaneofibular ligament. [1]The lateral ligaments stabilize the ankle, and serve as a guide to direct ankle motion by attaching the lateral malleolus to the bones below the ankle joint. They are responsible for resistance against inversion and internal rotation stress. [3]
- The anterior talofibular ligament connects the talus to the fibula, the weakest of the three lateral ligaments and thus the most frequently injured.
- The posterior talofibular ligament connects the talus to the fibula
- The calcaneofibular ligament connects the fibula to the calcaneus inferiorly.
See the table below for a full description of ligaments.
|
LIGAMENT |
DESCRIPTION | PROXIMAL ATTACHMENT | DISTAL ATTACHMENT | FUNCTION |
|---|---|---|---|---|
|
Anterior Talofibular Ligament (ATFL) |
Flat Weak Band that extends Anteriomedially. Most commonly damaged ligament of the ankle. |
Lateral Malleolus | Neck of Talus |
Restrain anterior displacement of the talus in respect to the fibula and tibia. Resists Inversion in plantarflexion. |
|
Posterior Talofibular Ligament (PTFL) |
Thick, a fairly strong band that runs horizontally medially. This ligament is under greater strain in full dorsiflexion of the ankle. Rarely injured because bony stability protects ligaments when ankle in dorsiflexion. |
Malleolar Fossa of Fibula | Lateral Tubercle of Talus |
Forms the back wall of the recipient socket for the talus' trochlea. Resists posterior displacement of the talus. |
|
Calcaneofibular Ligament (CFL) |
Round cord that passes posteroinferior | Tip of Lateral Malleolus | Lateral Surface of Calcaneus |
Aids Talofibular stability during Dorsiflexion. Restrain inversion of the calcaneus with respect to the fibula. Prevent Talar tilt into Inversion. |
|
LIGAMENTS |
DESCRIPTION | PROXIMAL ATTACHMENT | DISTAL ATTACHMENT | FUNCTION |
|---|---|---|---|---|
|
Anterior Tibiotalar Ligament |
Medial Malleolus |
Head of Talus |
Reinforces Ankle Joint. Control Plantarflexion & Eversion | |
|
Posterior Tibiotalar Ligament |
Talus Posteriorly | Control Dorsiflexion | ||
|
Tibionavicular Ligament |
Forms most anterior part of the Deltoid Ligament |
Dorsomedial Aspect of Navicular | Reinforces Ankle Joint | |
|
Tibiocalcaneal Ligament |
Very thin ligament | Sustentaculum Tali | Reinforces Ankle Joint |
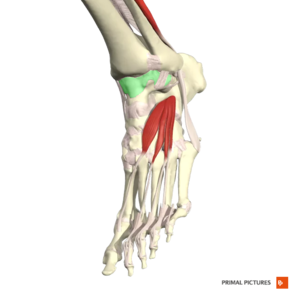
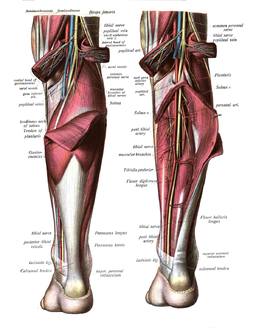
Muscles[edit | edit source]
The muscles of the leg divide into anterior, posterior, and lateral compartments.
- The leg's posterior compartment of the leg divides into the superficial posterior compartment and the deep posterior compartment. The superficial posterior compartment consists of the gastrocnemius and the soleus muscles, which are the primary muscles involved in ankle plantarflexion. The deep compartment plays a role in ankle joint inversion.
- The tibialis anterior muscle, found in the anterior compartment of the leg, is the primary muscle that facilitates dorsiflexion of the ankle joint.
- The peroneus longus and Peroneus Brevis muscles, found in the lateral compartment of the leg, function to facilitate eversion of the ankle joint.[1]
A complete listing of muscles are described below.
Plantar flexion[edit | edit source]
Muscles which contribute to Plantar flexion
|
MUSCLE |
ACTION | PROXIMAL ATTACHMENT | DISTAL ATTACHMENT | INNERVATION |
|---|---|---|---|---|
|
POSTERIOR COMPARTMENT | ||||
|
SUPERFICIAL | ||||
| Gastrocnemius |
Plantarflexion when Knee Extended Flexion Knee Raises Heel during Walking |
Lateral Head: Lateral Aspect of Lateral Femoral Condyle Medial Head: Popliteal Surface of Femur Superior to Medial Femoral Condyle |
Posterior Surface Calcaneus via Calcaneal Tendon (Achilles Tendon) |
Tibial Nerve S1-S2 |
| Soleus |
Plantarflexion Steadies Leg on Foot |
Posterior Aspect of Head Fibula Superior ¼ Posterior Surface Tibia Soleal Line & Medial Border Tibia | ||
| Plantaris |
Weakly Assists Gastrocnemius in Plantarflexion |
Inferior end Lateral Supracondylar Line of Femur Oblique Popliteal Ligament | ||
|
DEEP | ||||
| Tibialis Posterior |
Plantarflexion Inversion Supports Medial Longitudinal Arch |
Interosseous Membrane Posterior Surface Tibia inferior to Soleal Line Posterior Surface Fibula |
Navicular Tuberosity Cuneiform Cuboid Bases of Metatarsals 2-4 |
Tibial Nerve L4-L5 |
| Flexor Digitorum Longus |
Plantarflexion Flexion Lateral Four Digits Supports Longitudinal Arch |
Medial Part Posterior Surface Tibia inferior to Soleal Line Broad Tendon to Fibula |
Base Distal Phalanges Digits 2-4 |
Tibial Nerve S2-S3 |
| Flexor Hallucis Longus |
Weak Plantarflexion Flexion Big Toe at all Joints Supports Medial Longitudinal Arch |
Inferior 2/3 Posterior Surface Fibula Inferior Part Interosseous Membrane |
Base Distal Phalanx of Big Toe | |
|
LATERAL COMPARTMENT | ||||
|
Peroneus Brevis |
Weak Plantarflexion Eversion |
Inferior 2/3 of Lateral Surface Fibula |
Dorsal Surface Tuberosity of Base 5th Metatarsal |
Superficial Peroneal Nerve (Superficial Fibular Nerve) L5 - S2 |
|
Peroneus Longus |
Weak Plantarflexion Eversion Supports Transverse Arch |
Head & Superior 2/3 of Lateral Surface Fibula |
Base 1st Metatarsal Medial Cuniform | |
Dorsiflexion[edit | edit source]
Muscles which contribute to Dorsiflexion
|
MUSCLE |
ACTION | PROXIMAL ATTACHMENT | DISTAL ATTACHMENT | INNERVATION |
|
ANTERIOR COMPARTMENT | ||||
|
Tibialis Anterior |
Dorsiflexion Inversion Supports Medial Longitudinal Arch |
Lateral Condyle Tibia Superior ½ Lateral Surface Tibia Interosseous Membrane |
Medial & Inferior Surfaces Medial Cuniform Base of 1st Metatarsal |
Deep Peroneal Nerve (Deep Fibular Nerve) L4-L5 |
|
Extensor Digitorum Longus |
Dorsiflexion Extends Lateral Four Digits |
Lateral Condyle Tibia Superior ¾ Anterior Surface Interosseous Membrane |
Middle & Distal Phalanges of Lateral Four Digits |
Deep Peroneal Nerve (Deep Fibular Nerve) L5-S1 |
|
Extensor Hallucis Longus |
Dorsiflexion Extends Big Toe |
Middle Part Anterior Surface Fibula Interosseous Membrane |
Dorsal Aspect of Base Distal Phalanx of Big Toe | |
|
Peroneus Tertius |
Dorsiflexion Aids Eversion |
Inferior 1/3 Anterior Surface Fibula Interosseous Membrane |
Dorsum Base 5th Metatarsal | |
Blood Supply[edit | edit source]
Derived from Malleolar Branches of:
- Peroneal Artery
- Anterior and posterior Tibial Artery
Nerve Supply[edit | edit source]
Clinical Significance[edit | edit source]
Ankle Fracture - Ankle fractures are common in all ages with the involvement of one or both malleoli. The fracture pattern determines the stability of the fracture. Patients typically present with pain, swelling, and inability to bear weight on the ankle joint. Management of stable fractures includes a short leg cast for 4 to 6 weeks. Unstable fractures require an open reduction and internal fixation (ORIF) to restore a congruent mortise and fibular length.
Talus Fracture - This injury usually occurs from a high energy injury like a motor vehicle accident or a fall from a height. The talus has a tenuous blood supply and is at high risk of avascular necrosis (AVN) in displaced fractures.[1]
Ligament Injury - Ankle sprain is one of the most common musculoskeletal injuries, Females were at a higher risk of sustaining an ankle sprain compared with males and children compared with adolescents and adults, with indoor and court sports the highest risk activity.[4]
Motions Available[edit | edit source]
- Talocrural Joint is a uniaxial hinge joint that has just 1° of Motion
- The reported normal available range for dorsiflexion varies in the literature between 0-16.5o[5] and 0-25o.[6] This changes in weight-bearing.
- The normal range of Plantarflexion has been reported to be around 0°- 50°
Closed Packed Position[edit | edit source]
- Maximum Dorsiflexion
Open Packed Position[edit | edit source]
- 10° Plantarflexion
Structures Limiting Movement[edit | edit source]
| Movement | Limiting Structures |
|---|---|
| Plantarflexion Posterior & Lateral Compartment |
Anterior Talofibular Ligamanet Anterior Part of Medial Ligament Anterior Joint Capsule Tension Contact of Talus with Tibia Dorsiflexor Tension |
| Dorsiflexion Anterior Compartment |
Medial Ligament Calcaneofibular Ligament Posterior Talofibular Ligament Posterior Joint Capsule Tension Contact of Talus with Tibia Plantarflexors Tension |
Clinical Examination[edit | edit source]
Assessment[edit | edit source]
Special Tests[edit | edit source]
- Kaltenborn Ankle & Foot Examination
- Anterior Drawer of the Ankle
- Squeeze Test
- Talar Tilt Test
- Kleiger Test
Clinical Prediction Rules[edit | edit source]
- Ottawa Ankle Rules to rule in/out radiography of the ankle after trauma. Ankle X-ray is necessary if any of the following are present.
- Inability to bear weight on the affected ankle
- Bone tenderness along the posterior aspect of the distal 6 cm of either the medial or lateral malleolus
- Point tenderness at the proximal base of the fifth metatarsal
- Point tenderness over the navicular bone[1]
Outcome Measures[edit | edit source]
- Foot and Disability Index&is a 34-item self-report questionnaire divided into two subscales: the Foot and Ankle Disability Index and the Foot and Ankle Disability Index Sport
Pathology/Injury[edit | edit source]
- Ankle Arthrodesis
- Ankle Impingement
- Ankle Osteoarthritis
- Ankle Osteochondral Lesions
- Ankle Sprain
- Ankle and Foot Fractures
- Ankle and Foot Arthropathies
- Chronic Ankle Instability
Physiotherapeutic Techniques[edit | edit source]
Rehabilitation of ankle injuries should be structured and individualized.
- In the acute phase, the focus should be on controlling inflammation, reestablishing full range of motion, and gaining strength.
- Once a pain-free range of motion and weight-bearing has been established, balance-training exercises should be incorporated to normalize neuromuscular control.
- Advanced-phase rehabilitation activities should focus on regaining normal function eg exercises specific to those that will be performed during sport.
- While having a basic template to follow for the rehabilitation of ankle injuries is important, clinicians must remember that individuals respond differently to exercises. Therefore, each program needs to be modified to fit the individual's needs.[7]
Below are examples of techniques that could be incorporated in rehabilitation.
Manual Therapy[edit | edit source]
- Talocrural Joint Posterior Glide to Promote Dorsiflexion
- Talocrural Joint Anterior Glide to Promote Plantarflexion
- Talocrural Joint Distal Distraction [8][8]
Balance Retraining[edit | edit source]
Return to activity specific training[edit | edit source]
For sports persons an example is given below:
When pain-free walking is achieved, progress to a regimen of 50% walking and 50% jogging. Using the same criteria, jogging eventually progresses to running, backward running, and pattern running. Circles and figures of 8 are commonly employed patterns. The final phase of the rehabilitation process is the athlete can perform sport-specific exercises pain-free and at a level consistent with pre-injury status.
These routines represent the final phase of ankle-joint rehabilitation, and completion of this program is essential for the recovery of ankle stability. Physiotherapists need to create exercises and movement patterns that will increasingly challenge the neuromuscular coordination of the injured athlete.[7]
Procedures[edit | edit source]
Resources[edit | edit source]
- Anatomy of the Ankle Ligaments: A Pictorial Essay - In this pictorial essay, the ligaments around the ankle are grouped, depending on their anatomic orientation, and each of the ankle ligaments is discussed in detail.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Manganaro D, Dollinger B, Nezwek TA, Sadiq NM. Anatomy, Bony Pelvis and Lower Limb, Foot Joints.2019 Available from:https://www.ncbi.nlm.nih.gov/books/NBK545158/ (last accessed 10.3.2020)
- ↑ Anatomyzone Ankle anatomy Available from:https://www.youtube.com/watch?v=lPLdoFQlZXQ&t=23s (last accessed 10.3.2020)
- ↑ 3.0 3.1 3.2 Moore KL, Agur AMR, Dalley AF. Essential Clinical Anatomy. Baltimore: Lippincott Williams and Wilkins, 2011.
- ↑ Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports medicine. 2014 Jan 1;44(1):123-40. Available from:https://www.ncbi.nlm.nih.gov/pubmed/24105612 (last accessed 10.3.2020)
- ↑ Baggett BD, Young G. Ankle joint dorsiflexion. Establishment of a normal range. Journal of the American Podiatric Medical Association. 1993 May;83(5):251-4.
- ↑ CDCP. Normal joint range of motion study. Accessed https://www.cdc.gov/ncbddd/jointrom/
- ↑ 7.0 7.1 Mattacola CG, Dwyer MK. Rehabilitation of the ankle after an acute sprain or chronic instability. Journal of athletic training. 2002 Oct;37(4):413. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164373/ (last accessed 10.3.2020)
- ↑ PT Haven. Talocrural Joint Distal Distraction. Available from: http://www.pthaven.com/page/show/162347-talocrural-joint-distal-distraction [last accessed 19/03/2015]