Ankle and Foot Arthropathies
Original Editors - Ward Willaert as part of the Vrije Universiteit Brussel Evidence-Based Practice Project Top Contributors - Anouck Leo, Admin, Arturo Quiroz Marnef, Evelien De Wolf, Scott Cornish, Kim Jackson, Lucinda hampton, Rachael Lowe, Ward Willaert, Yuli Borremans, 127.0.0.1, Gayatri Jadav Upadhyay, Cath Young, Maxim de Clippele, Mariam Hashem, Jan De Backer, Sai Kripa, Aminat Abolade, Fitim Cami and Veekhoven Laura
Introduction[edit | edit source]
Any joint in the ankle, foot and toes can be affected by an arthropathy (arthropathy is a general term for any disease of the joints).
- There are more than 100 forms of arthritis, many of which affect the foot and ankle, causing joint pain, swelling and stiffness.
- Arthritis in the feet can make standing and walking painful and the feet and/or toes may change shape, making it harder to fit shoes and Activities of Daily Living may be affected.
- Athropathies of the foot and ankle are an important public health challenge due to their increasing incidence combined with their substantial negative impact on patients’ quality of life.
- Although arthropathy is less common in the ankle than the hip and knee, it can be just as disabling.[1]
- Non-pharmacological treatments serve as the first line of treatment and are frequently used for patients with musculoskeletal conditions of the foot and ankle[2].
Arthropathy is a blanket or global term for a wide range of joint presentations.
- Noninfectious arthritis eg Psoriatic arthritis; Ankylosing spondylitis; Gout; Rheumatoid Arthritis; Osteoarthritis; Haemophilic Arthropathy (with severe haemophilia causes high levels of impairment) [3]; Post traumatic Arthritis.
- Reactive arthropathy occurs as a reaction against an infection site elsewhere in the body.[4]
- Enteropathic arthropathy Includes a group of rheumatic conditions such as arthritis caused by bacteria, parasitic infections and spondyloarthropathies. Other conditions that are included in this type of arthropathy are intestinal bypass arthritis, Whipple’s disease , collagenous colitis and celiac disease.[5][6]
- Crystal arthropathy is characterised by accumulation of tiny crystals in one or more joints.[7]
- Neuropathic arthropathy is gradual joint destruction when there is chronic damage of peripheral nerves and diminished proprioception (also called Charcot arthropathy and prominently affects patients with diabetes)[6] [8]
- Diabetic arthropathy is a neuropathic arthropathy occurring in diabetic patients. [9]
Be sure to look at all the links above for detailed information, this page is a general overview.
Relevant Anatomy[edit | edit source]
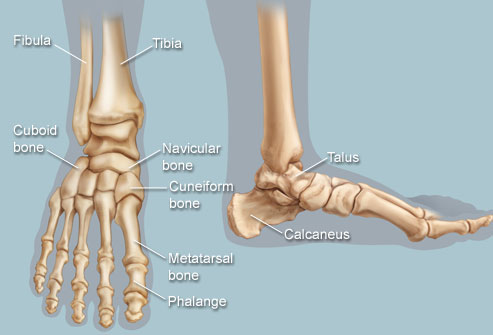
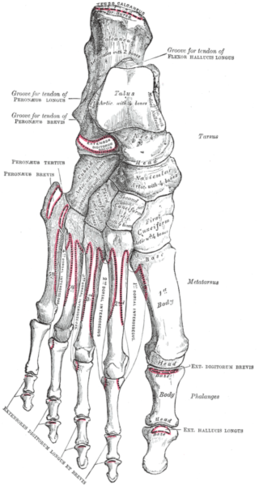
Each foot has 28 bones and more than 30 joints. The most common foot joints that arthritis affects are:
- The Ankle joint
- The 3 joints of the foot that involve the calcaneus, the navicular , and the cuboid bone.
- The !st MTP joint [10]
More information about the anatomy of the ankle and foot can be found here: Biomechanics of Foot and Ankle and Ankle Joint.
Signs and Symptoms[edit | edit source]
In general the symptoms are pain in the joints, reduction of the functions of the structure of connection or support and inflammation in the tendons, ligaments, joints, muscles and bones.
- Decreased range of motion, effusion, neumarthrosis, bone erosion.
- The symptoms are similar to rheumatic conditions and include pain, swelling and stiffness.
- Skeletal muscle is also affected by pain and inflammation of bones, structure, muscles, and is a type of joint disease[6].
- Pain usually increases on activities such as standing, walking or running.
- “Start-up pain” is also a common complaint, where the patient experiences pain and stiffness in the ankle on moving after being asleep or sitting for a long period, which takes a few minutes of motion to settle.
- The affected joints will tend to increasingly swell as the day progresses, particularly with a higher level of activity.
Assessment[edit | edit source]
A clinical examination of the foot includes ‘traditional’ components such as history, palpation, and assessments of sensation, range of motion and strength, as well as special tests that provoke specific tissues. On observation, toe deformities and skin health (dryness, sweating, perfusion) should be noted.[2]
Salient Points of Examination include:
- Patients’ self-reported outcomes eg VAS, PSFS
- Static Foot Structure and Alignment eg the Foot Posture Index
- Joint Range of Motion - Quantified using a goniometer, and note position tested in.
- Muscle strength - Decreased toe flexor strength and foot pain are independently associated with fall risk. Strength deficits have also been reported in individuals with foot pain secondary to tibialis posterior tendinopathy[2].
- Footwear assessment - Inspect for fit (length and width) and design features such as the presence of a heel cup, arch support, torsional and toe-break flexibility. Patterns of wear on the sole of the shoe and/or or scuffing should be noted. The Footwear Assessment Form is a simple and well-organized tool with established reliability and face-validity[2].
- Dynamic Assessment of Foot Motion (including Gait Analysis) - Involves an observational or quantitative assessment of foot and lower extremity mechanics during a weight-bearing task (e.g., walking, running, single limb squat, step down). Particularly relevant in a clinical foot exam because evidence indicates that there is only a weak relationship between static and dynamic measures of arch height and large between-person variability[2]
- Dynamic Assessment of Plantar Load Distribution - When performing a clinical assessment, the plantar aspect of the foot should be inspected for patterns of calluses and weight-bearing.
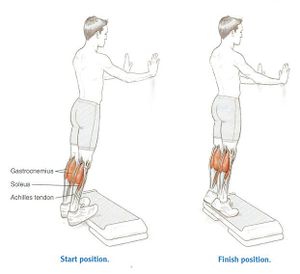
- Provocational Tests - The final part of the clinical examination comprises provocational tests that provoke specific tissues. The Windlass Testtstretcheshe plantar fascia and is considered positive if the patient reports pain when the 1st metatarso-phalanegeal joint is passively dorsiflexed. Limited extensibility in the gastrocnemius-soleus complex or the flexor hallucis longus can be assessed using passive muscle length testing. Symptoms related to the sesamoids may manifest as plantar pain and localized tenderness to palpation.[2]
Medical Treatment[edit | edit source]
Management of ankle and foot arthropathies generally commences with conservative interventions, including analgesic or anti-inflammatory medications, therapeutic injections, physical therapy, footwear modifications and foot orthoses. If these treatments are ineffective, surgical options may be considered.[11]
The medications used to treat arthropathies vary depending on the diagnosis. Commonly used medications include:
- Painkillers eg paracetamol, For more-severe pain, opioids might be prescribed,
- Oral non-steroidal anti-inflammatory drugs (NSAIDs) are the most widely used first-line pharmacological treatment. Some NSAIDs are also available as creams or gels, which can be rubbed on joints.[12]
- Counterirritants. Some varieties of creams and ointments contain menthol or capsaicin, the ingredient that makes hot peppers spicy. Rubbing these preparations on the skin over your aching joint may interfere with the transmission of pain signals from the joint itself.
- Disease-modifying antirheumatic drugs (DMARDs). Often used to treat rheumatoid arthritis, DMARDs slow or stop your immune system from attacking your joints. eg methotrexate (Trexall, Rasuvo, others) and hydroxychloroquine (Plaquenil).
- Biologic response modifiers. Typically used in conjunction with DMARDs, biologic response modifiers are genetically engineered drugs that target various protein molecules that are involved in the immune response. eg Tumor necrosis factor (TNF) inhibitors are commonly prescribed. Other medications target other substances that play a role in inflammation eg interleukin-1 and certain types of white blood cells known as B cells and T cells.
- Corticosteroids. This class of drugs, which includes prednisone (Prednisone Intensol, Rayos) and cortisone (Cortef), reduces inflammation and suppresses the immune system. Corticosteroids can be taken orally or can be injected directly into the painful joint[12].
Therapeutic Injections: Provide an effective alternative financially and some evidence exists that they are effective in pain alleviation (current evidence is limited and the benefit described from injection therapy has been short-lived in most cases)[13].
- The most widely used are: corticosteroid injections and Viscosupplementation, the intra-articular injection of a lubricating fluid (hyaluronan) (aim of restoring the viscoelasticity of the synovial fluid).[11]
- Regenerative Injections are another option 1. Platelet-rich plasma (PRP) injections - these injections use your own blood and platelets to promote healing. Platelets contain growth factors and proteins that aid healing in soft tissues. Research shows PRP injections can alter the immune response to help reduce inflammation; 2. Placental tissue matrix (PTM) injections - injections of placental tissue (obtained after a healthy baby is delivered from a healthy mother), there is a large number of growth factors in placental tissue that promote healing[14]; 3. Mesenchymal Stem Cells (MSC) - Mesenchymal stem cells are usually collected from the patient’s fat tissue, blood, or bone marrow. When administering stem cell injections, many physicians use medical imaging, such as ultrasound, in order to deliver cells precisely to the site of cartilage damage.When administering stem cell injections, many physicians use medical imaging, such as ultrasound, in order to deliver cells precisely to the site of damage[15].
Physiotherapy[edit | edit source]
The primary aim of treatment is to afford pain relief, restore mechanics (alignment, motion and/or load distribution) and return the patient to their desired level of activity participation. Individualised treatment is paramount taking into account clients diagnosis.
The plan of care should be designed with the goal of targeting impairments noted during assessment. Options include (see links also):
- Lifestyle Modifications
- In the early stages of arthritathies, limiting the amount of force being placed on the foot and ankle may relieve pain. For example, low-impact activities such as swimming and yoga can provide cardiovascular benefits without putting stress on the foot or ankle.
- Losing weight may decrease pressure on the joints. The foot and ankle support the entire body every time we stand and move, and being overweight increases this pressure and may cause arthritis to progress more quickly.
3. Manual therapy examples include
- Massage – with sufficient pressure through the superficial tissue to reach the deep lying structures (used to increase blood flow, decrease swelling, reduce muscle spasm and promote normal tissue repair).
- Mobilisation – joint and soft tissues are gently moved to restore normal range, lubricate tissues and relieve pain. eg Talar glides, Maitland mobilisations
4. Stretching and therapeutic exercises, eg Stretches that target hamstrings, calves, foot arch and heel are particularly effective and complete range of motion exercises. Strengthening exercises like "small foot exercise", attempting to pick up pegs with toes, walking bare feet in sand.
5. Cryotherapy or Thermotherapy
6. Ultrasonic Therapy – to reduce tissue spasm, accelerates healing and pain relief.
7. IInterferential Therapy – used for differing treatment effects. E.g. pain relief, muscle or nerve stimulation, promoting blood flow and reducing inflammation.
8. Gait re-education – assess and treat appropriately with eg gait aides
9. Taping
Epidemiology /Etiology[edit | edit source]
- Osteoarthritis - Approximately 1% of the world’s adult population is affected by ankle OA [3]
- Rheumatoid Arthritis - The prevalence of foot pain in patients with RA has been reported at ranges from 60 to 94 % at some stage of the disease. [16][17]
- Diabetic Foot Arthropathy - Charcot neuropathic osteoarthropathy are detected in up to 29% of diabetics, whereas under MRI the detection rate rises to 75%.[18]
- Gout - The global prevalence of gout is substantial and is increasing in many parts of the world over the past 50 years. The distribution of gout is uneven across the globe, with prevalence being highest in Pacific countries. Developed countries tend to have a higher prevalence of gout than that of developing countries and incidence of the disease appears to be on the increase. [19]
- Psoriatic Arthritis - Prevalence of Psoriatic arthritis in psoriasis patients is between 6% and 39%. It is possible that the condition remains generally underdiagnosed, related to lack of awareness by both the patient and physician. [20]
Clinical Bottom Line[edit | edit source]
- Ankle and foot arthropathies covers all joint disease types of the foot and ankle.
- Physical therapy can be effective in all cases of ankle and foot arthropathies
- Accurate differential diagnosis is important so that the most appropriate management protocol is implemented for the specific disease.
- Recent studies show that individuals with foot and ankle pain have multiple co-existing impairments in alignment, motion, load distribution and muscle performance.
- A comprehensive assessment of the foot and ankle should include patients’ self-reported outcomes and measures of alignment, motion, strength and provocative tests.
- Increasing evidence highlights the importance of evaluating dynamic function and regional interdependence (advances in motion capture and plantar load distribution offer exciting opportunities to obtain precise, clinically relevant measures).
Non-surgical interventions are important factors to ease foot pain and slow the disease-related progression of foot and ankle conditions often seen with the rheumatic diseases. Increasingly, studies are showing that orthoses, footwear and other rehabilitation interventions may play an important role in rheumatology-related foot treatment[2].
References[edit | edit source]
- ↑ Stauffer RN: Intra-articular ankle problems. In Evarts CM (ed): surgery of the musculoskeletal system, vol. 4. New York, Churchill-Livingstone, 1990.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Rao S, Riskowski JL, Hannan MT. Musculoskeletal conditions of the foot and ankle: assessments and treatment options. Best Practice & Research Clinical Rheumatology. 2012 Jun 1;26(3):345-68. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3414868/ (last accessed 1.7.2020)
- ↑ 3.0 3.1 Barg, A., et al. Haemophilic arthropathy of the ankle treated by total ankle replacement: a case series. Haemophilia 2010;16(4):647-655.
- ↑ Reactive Arthritis (Reiter’s Syndrome). www.mayoclinic.org. Retrieved May 16, 2011.(accessed 3 december 2016)
- ↑ Björkengren A. G., Resnick D, Sartoris DJ. Enteropathic arthropathies. Radiologic Clinics of North America 1987: 189
- ↑ 6.0 6.1 6.2 Scope heal Arthropathy Available from:https://scopeheal.com/arthropathy/ (last accessed 1.7.2020)
- ↑ McGill, Neil W. Gout and other crystal-associated arthropathies. Best Practice & Research Clinical Rheumatology 2000: 445-460
- ↑ Sanders, L.J., Edmonds, M.E. & Jeffcoate, W.J. Diabetologia (2013) 56: 1873. https://doi.org/10.1007/s00125-013-2961-6
- ↑ Medical dictionary. http://medical-dictionary.thefreedictionary.com/diabetic+arthropathy (Accessed 2 december 2016)
- ↑ Cleveland clinic Foot and ankle arthritis Available from:https://my.clevelandclinic.org/health/diseases/13900-foot-and-ankle-arthritis (last accessed 1.7.2020)
- ↑ 11.0 11.1 Roddy E, Menz HB. Foot osteoarthritis: latest evidence and developments. Therapeutic advances in musculoskeletal disease. 2018 Apr;10(4):91-103. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5871064/ (last accessed 2.7.2020)
- ↑ 12.0 12.1 Mayo clinic Arthritis Available from:https://www.mayoclinic.org/diseases-conditions/arthritis/diagnosis-treatment/drc-20350777 (last accessed 2.7.2020)
- ↑ Urits I, Smoots D, Franscioni H, Patel A, Fackler N, Wiley S, Berger AA, Kassem H, Urman RD, Manchikanti L, Abd-Elsayed A. Injection Techniques for Common Chronic Pain Conditions of the Foot: A Comprehensive Review. Pain and therapy. 2020 Feb 27:1-6. Available from:https://link.springer.com/article/10.1007/s40122-020-00157-5 (last accessed 2.7.2020)
- ↑ Clevelandclinic 4 Therapeutic injections Available from:https://health.clevelandclinic.org/4-injections-that-can-banish-joint-pain-for-months/ (last accessed 2.7.2020)
- ↑ arthritis health SCT Available from: https://www.arthritis-health.com/treatment/injections/stem-cell-therapy-arthritis (last accessed 2.7.2020)
- ↑ Lohkamp M. et al. The prevalence of disabling foot pain in patients with early rheumatoid arthritis. The Foot 2006;16(4):201-207.
- ↑ Brenton-Rule, Angela, et al. Foot and ankle characteristics associated with falls in adults with established rheumatoid arthritis: a cross-sectional study.BMC musculoskeletal disorders 2016;17(1):1.
- ↑ Kucera, Tomas, Haroun Hassan Shaikh, and Pavel Sponer. Charcot Neuropathic Arthropathy of the Foot: A Literature Review and Single-Center Experience. Journal of Diabetes Research 2016
- ↑ Kuo CF, et al. Global epidemiology of gout: prevalence, incidence and risk factors. Nature Reviews Rheumatology 2015;11(11):649-662.
- ↑ Mease P. Psoriatic arthritis update." BULLETIN-HOSPITAL FOR JOINT DISEASES NEW YORK 64.1/2 (2006): 25.