Hip Anatomy
Top Contributors - Tyler Shultz, Admin, Kim Jackson, Aarti Sareen, Samuel Adedigba, Lucinda hampton, Laura Ritchie, Leana Louw, Rachael Lowe, Scott Buxton, Joao Costa, Ewa Jaraczewska, Ahmed M Diab, Kirenga Bamurange Liliane, Evan Thomas, George Prudden, Priyanka Chugh and WikiSysop
Description[edit | edit source]
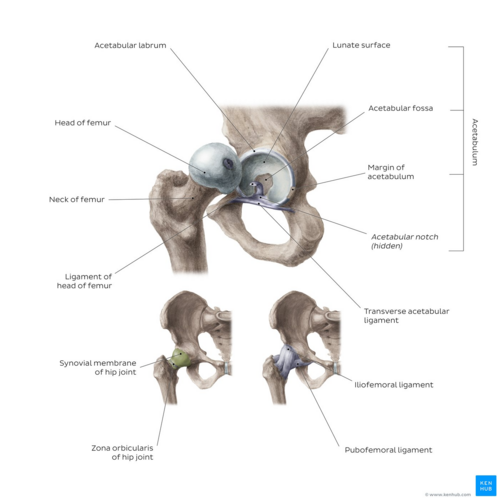
The hip joint is a ball and socket joint that is the point of articulation between the head of the femur and the acetabulum of the pelvis.
Hip Joint
- Diarthrodial joint with its inherent stability dictated primarily by its osseous components/articulations.
- Primary function of the hip joint is to provide dynamic support the weight of the body/trunk while facilitating force and load transmission from the axial skeleton to the lower extremities, allowing mobility[1]
- Typically works in a closed kinematic chain.
Motions Available[edit | edit source]
The hip joint connects the lower extremities with the axial skeleton. The hip joint allows for movement in three major axes, all of which are perpendicular to one another.
- The location of the center of the entire axis is at the femoral head.
- The transverse axis permits flexion and extension movement.
- The longitudinal axis, or vertically along the thigh, allows for internal and external rotation.
- The sagittal axis, or forward to backward, allows for abduction and adduction.
In addition to movement, the hip joint facilitates weight-bearing. Hip stability arises from several factors.
- Shape of the acetabulum - Due to the depth of the acetabulum, it can encompass almost the entire head of the femur.
2. Acetabular labrum (fiibrocartilaginous collar surrounding the acetabulum) which provides the following functions:
- Load transmission
- Negative pressure maintenance (i.e., the "vacuum seal") to enhance hip joint stability
- Regulation of synovial fluid hydrodynamic properties
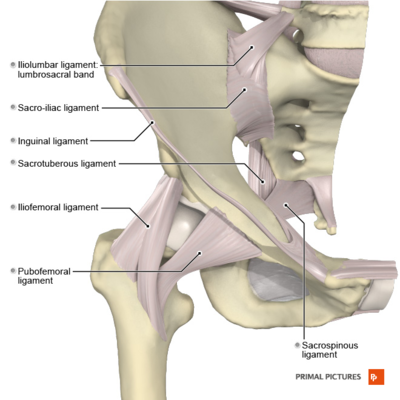
Ligaments & Joint Capsule[edit | edit source]
In general, the hip joint capsule is tight in extension and more relaxed in flexion.
The capsular ligaments include
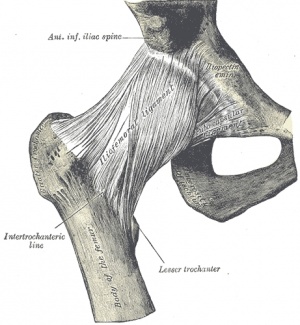
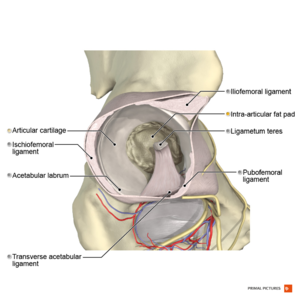
- Iliofemoral ligament (also known as the Y ligament of Bigelow) is the strongest ligament in the body; it lies on the anterior aspect of the hip joint - it prevents hyperextension,
- Pubofemoral lies anteroinferiorly - it prevents excess abduction and extension
- Ischiofemoral ligaments - is the weakest of the three ligaments and consists of a triangular band of fibres that form the posterior hip joint capsule. It attaches to the ischium to behind the acetabulum and it attaches to the base of the greater trochanter - it prevents excess extension
The ligamentum teres (ligament of the head of the femur)
- Located intracapsular and attaches the apex of the cotyloid notch to the fovea of the femoral head.
- Serves as a carrier for the foveal artery (posterior division of the obturator artery), which supplies the femoral head in the infant/pediatric population (vascular contribution to the femoral head blood supply is negligible in adults).
- Injuries to the ligamentum teres can occur in dislocations, which can cause lesions of the foveal artery, resulting in osteonecrosis of the femoral head.[1]
Joint Capsule:
- The hip joint is extremely strong, due to its reinforcement by strong ligaments and musculature, providing a relatively stable joint. Unlike the weak articular capsule of the shoulder, the hip joint capsule is a substantial contributor to joint stability[2]. The capsule is thicker anterosuperiorly where the predominant stresses of weight bearing occur, and is thinner posteroinferiorly.[3]
Labrum[edit | edit source]
The labrum forms a fibrocartilagenous extension of the bony acetabulum, mostly composed of type 1 collagen that is typically between 2-3mm thick. It lines the acetabular socket and attaches to the bony rim of the acetabulum. It has an irregular shape, being wider and thinner anteriorly and thicker posteriorly.[4][5] On the anterior aspect, the labrum is triangular in the radial section. On the posterior aspect, the labrum is dimensionally square but with a rounded distal surface.[6][7]
The labrum has three surfaces:
- Internal articular surface - adjacent to the joint (avascular)
- External articular surface - contacting the joint capsule (vascular)
- Basal surface - attached to the acetabular bone and ligaments
The transverse ligaments surround the hip and help hold it in place while moving.
It is thought that the majority of the labrum is avascular with only the outer third being supplied by the obturator, superior gluteal and inferior gluteal arteries. There is controversy as to whether there is a potential for healing with the limited blood supply and this is an important clinical consideration. The superior and inferior portions are believed to be innervated, containing both free nerve endings and nerve sensory end organs (giving the senses of pain, pressure and deep sensation).[4][5]
The functions of the acetabular labrum are:[4]
- Joint stability - increases the containment of the femoral head, deepening the joint by 21%, increasing the surface area of the joint by 28%, thus allowing a wider area of force distribution and resisting lateral and vertical motion within the acetabulum
- Sensitive shock absorber
- Joint lubricator - sealing mechanism keep the synovial fluid in contact with the articular cartilage
- Pressure distributor - obstructs fluid flow in and out of the joint through a sealing action which is often referred to as a “suction effect” in view of the resistance generated to distraction of the head from the acetabular socket. This sealing function not only enhances joint stability, but is thought to more uniformly distribute compressive loads applied to the articular surfaces, thereby reducing peak cartilage stresses during weight-bearing.[8]
- Decreasing contact stress between the acetabular and the femoral cartilage[9][10]
Image: Hip joint from different perspectives [11]
Nerves[edit | edit source]
The hip joint receives innervations from the femoral, obturator, superior gluteal nerves.
Blood Supply[edit | edit source]
Numerous variations in the blood supply to the hip.
- Most common variant results in blood supply coming from the medial circumflex and lateral circumflex femoral arteries, each of which is a branch of the profunda femoris (deep artery of the thigh).
- The profunda femoris is a branch of the femoral artery which travels posteriorly.
- There is an additional contribution from the foveal artery (artery to the head of the femur), a branch of the posterior division of the obturator artery, which travels in the ligament of the head of the femur.
- The foveal artery helps avoid avascular necrosis with disruption of the medial and lateral circumflex arteries.
- There are two significant anastomoses. The cruciate anastomosis supports the upper thigh and the trochanteric anastomosis, which supports the head of the femur[1].
Muscles[edit | edit source]
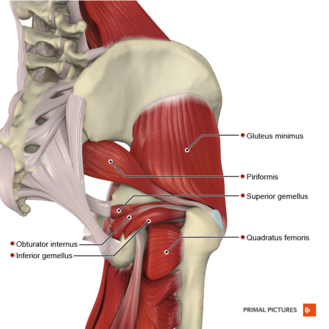
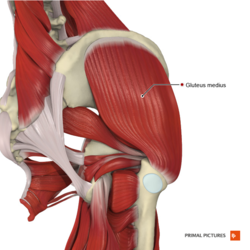
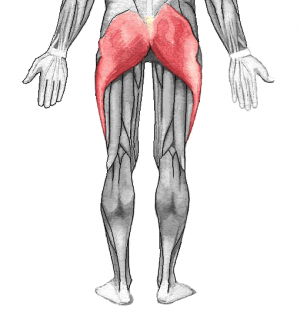
Muscles of the hip joint can be grouped based upon their functions relative to the movements of the hip
Flexors:
Extensors:
Adductors:
- Adductor Magnus
- Adductor Longus
- Adductor Brevis
- Gracilis
- Pectineus
Abductors:
Internal Rotators:
External Rotators:
- Gluteus Maximus
- Gemellus Superior
- Gemellus Inferior
- Obturator Externus
- Obturator Internus
- Quadratus Femoris
- Piriformis
Closed Packed Position[edit | edit source]
Full extension of the hip joint is the closed packed postion because this position draws the strong ligaments of the joint tight, resulting in stability.
Open Packed Position[edit | edit source]
The hip joint is one of the only joints where the position of optimal articular contact (combined flexion, abduction, and external rotation) is the open-packed, rather than closed packed position, since flexion and external rotation tend to uncoil the ligaments and make them slack.[2]
Important Information[edit | edit source]
Total hip arthroplasty (THA)
- Elective procedure for patients with hip pain secondary to degenerative conditions. Highly effective procedure that relieves pain and restores function to improve quality of life.
- Indicated for patients who have failed other conservative methods, including corticosteroid injections, physical therapy, weight reduction, or previous surgical treatments. [12][13]
Femoral Triangle:
- Region defined by the inguinal ligament superiorly, the adductor longus medially, and the sartorius laterally.
- Important because it contains numerous vascular and neural structures, including the femoral vein, artery, and nerve.
Femoral Angle of Inclination:
- The angle resulting from the intersection of a line down the long shaft of the femur and a line drawn through the neck of the femur.
- Typically, the normal adult has an angle of inclination between 120 and 125 degrees, it usually is closer to 125 in the elderly.
- An increase in this angle, greater than 125 degrees, results in coxa valga, and a decrease is called coxa vara.
Femoral Angle of Torsion:
- Formed by looking at the relationship between the axis of the femoral head and neck and the femoral condyles.
- Normal femur has an angle of torsion between 12 and 15 degrees.
- An increase in this angle is termed anteversion, while a decrease in this angle is termed retroversion*.
Applied Anatomy[edit | edit source]
When any of the features of lateral balance control fails, the supporting is upset. The pelvis tends to fall on the unsupported side when the individual stands on the affected limb. This is called Trendelenburg sign. The person walks with a characteristic lurching or waddling gait.
In A: Negative Trendlenburg's sign. The hip abductors are acting normally tilting the pelvis upwards when the opposite leg is raised from the ground.
In B: Positive Trendlenburg's sign. The hip abductors are unable to control the dropping of the pelvis when the opposite leg is raised.
2. Sciatic nerve
- Can be compressed at lower border of gluteus maximus by sitting on a bench with a sharp edge.
- May be injured by misplaced deep intravascular injections. To prevent this, the injection is usually given in the superolateral quadrant.
- May be injured in posterior dislocation of the hip joint.
3. Sciatic Hernia
- Pelvic structures may protrude through the greater sciatic foramen compressing the contents of the foramina and may present with pain, numbness and weakness in the lower limb if sciatic nerve is compressed.
4. Greater Trochanteric Pain Syndrome
5. Snapping hip
6. Slipped disc
- Pain of a prolapsed or strained lumbar intervertebral disc if often referred to the gluteal region or lateral aspect of the thigh.
- Inflammation of the bursa over the ischial tuberosity.
Resources[edit | edit source]
This video covers the anatomy of the hip joint [15]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Gold M, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Hip Joint. Available from:https://www.ncbi.nlm.nih.gov/books/NBK470555/ (last accessed 15.6.2020)
- ↑ 2.0 2.1 Levangie P, Norkin C. Joint structure and function: A comprehensive analysis. 4th ed. Philadelphia: The F.A. Davis Company; 2005.
- ↑ Glenister R, Sharma S. Anatomy, bony pelvis and lower limb, hip. [1]
- ↑ 4.0 4.1 4.2 Groh MM, Herrera J. A comprehensive review of hip labral tears. Current reviews in musculoskeletal medicine 2009;2(2):105-17.
- ↑ 5.0 5.1 Lewis CL, Sahrmann SA. Acetabular labral tears. Physical therapy 2006;86(1):110-21.
- ↑ Narvani AA, Tsiridis E, Tai CC, Thomas P. Acetabular labrum and its tears. British journal of sports medicine 2003;37(3):207-11.
- ↑ Lovell G. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Australian journal of science and medicine in sport 1995;27:76-9.
- ↑ Crawford MJ, Dy CJ, Alexander JW, Thompson M, Schroder SJ, Vega CE, Patel RV, Miller AR, McCarthy JC, Lowe WR, Noble PC. The 2007 Frank Stinchfield Award: the biomechanics of the hip labrum and the stability of the hip. Clinical Orthopaedics and Related Research 2007;465:16-22.
- ↑ Byrd JT. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy: The Journal of Arthroscopic & Related Surgery 1996;12(5):603-12.
- ↑ Martin RL, Enseki KR, Draovitch P, Trapuzzano T, Philippon MJ. Acetabular labral tears of the hip: examination and diagnostic challenges. Journal of Orthopaedic & Sports Physical Therapy 2006;36(7):503-15.
- ↑ Hip joint image - © Kenhub https://www.kenhub.com/en/library/anatomy/hip-joint
- ↑ Karachalios T, Komnos G, Koutalos A. Total hip arthroplasty: survival and modes of failure. EFORT open reviews. 2018 May 21;3(5):232-9.[2]
- ↑ Evans JP. Availability of specific tools to assess patient reported outcomes in hip arthroplasty in Spain. Identifying the best candidates to incorporate in an arthroplasty register. A systematic review and standardized assessment. [3]
- ↑ OG Anatomy. Gluteal region and back of the thigh. Available from http://www.oganatomy.org/projanat/gross/5/clinicalanatomy.htm (accessed 31/05/2020).
- ↑ Hip joint image - © Kenhub https://www.kenhub.com/en/library/anatomy/hip-joint