Coordination Exercises: Difference between revisions
No edit summary |
Joao Costa (talk | contribs) No edit summary |
||
| (35 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox">'''Original Editor '''-[[User:Rewan_Aloush|Rewan Aloush]] | ||
'''Original Editor '''- [[User:Rewan_Aloush|Rewan Aloush]] | '''Top Contributors''' -{{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
==Introduction== | |||
</ | The definition of coordination is the ability to execute smooth, accurate, controlled motor responses (optimal interaction of [[muscle]] function). | ||
* Coordination is the ability to select the right muscle at the right time with proper intensity to achieve proper action.[[File:Cerebellum.gif|right|frameless]] | |||
* Coordinated movement is characterized by appropriate speed, distance, direction, timing and muscular tension. | |||
It is the process that results in activation of motor units of multiple muscles with simultaneous inhibition of all other muscles in order to carry out a desired activity.<ref name=":0">Slide player [http://slideplayer.com/slide/4638093/ Coordination exercises] Available from: http://slideplayer.com/slide/4638093/ (last accessed 11.6.2019)</ref> | |||
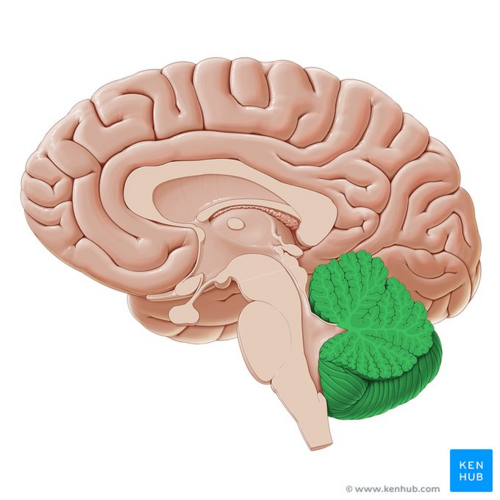
The [[cerebellum]] is the primary centre in the brain for coordination for movement and the ability to execute smooth accurate motor response. | |||
[[ | [[File:Cerebellum - Kenhub.png|alt=Cerebellum (highlighted in green) - sagittal view|right|frameless|500x500px|Cerebellum (highlighted in green) - sagittal view]] | ||
For coordinated movements to occurs all the below systems are involved | |||
* Cerebellum | |||
* [[Vestibular System|Vestibular system]] | |||
* | |||
* Vestibular system | |||
* Motor system. | * Motor system. | ||
* Flexibility and ROM. | * Flexibility and ROM. | ||
* Deep [[Sensation|sensations.]] | |||
* [[Sensation|Vision.]] | |||
Image: Cerebellum (highlighted in green) - sagittal view<ref >Cerebellum (highlighted in green) - sagittal view image - © Kenhub https://www.kenhub.com/en/library/anatomy/cerebellum-and-brainstem</ref> | |||
== Components of Coordinated Movement == | == Components of Coordinated Movement == | ||
Coordinated movement is dependent on: | Coordinated movement is dependent on:[[File:Juggle.gif|right|frameless]] | ||
* Volition: is the ability to initiate, maintain or stop an activity or motion. | * Volition: is the ability to initiate, maintain or stop an activity or motion. | ||
* Perception:in tact proprioception and subcortical centres to integrate motor impulses and the sensory feedback. When proprioception is affected it is compensated with visual feedback. | * Perception: in tact [[proprioception]] and [[Basal Ganglia|subcortical]] centres to integrate motor impulses and the sensory feedback. When proprioception is affected it is compensated with visual feedback. | ||
* | * Engram: A postulated physical or biochemical change in neural tissue that represents a memory<ref>Glosby [https://en.glosbe.com/en/en/Engram Engram in English] Available from: https://en.glosbe.com/en/en/Engram (last accessed 13.6.2019)</ref>. Research proved that high repetitions of precise performance must be performed in order to develop an engram.A 1980 study concluded "Thousands of repetitions are required to begin to form an engram and millions of repetitions are necessary to perfect it. Coordination is developed in proportion to the number of repetitions of an engram practiced just below the maximal level of ability to perform."<ref>Kottke FJ. [https://www.ncbi.nlm.nih.gov/pubmed/7458618 From reflex to skill: the training of coordination.] Archives of physical medicine and rehabilitation. 1980 Dec;61(12):551-61. Available from: https://www.ncbi.nlm.nih.gov/pubmed/7458618 (last accessed 13.6.2019)</ref> | ||
== | ==Types of Coordination== | ||
Motor coordination to complete a task a collaboration of three skills: | Motor coordination to complete a task a collaboration of three skills: | ||
# Fine Motor Skills | # Fine Motor Skills | ||
| Line 38: | Line 42: | ||
== Causes of Coordination Impairments == | == Causes of Coordination Impairments == | ||
Uncoordinated movement or coordination impairment is known medically known as ataxia. There are a number of known causes for [[ataxia]]. They range from chronic conditions to sudden onset. However, most conditions will relate to damage or degeneration of the [[cerebellum]]. | |||
== Examples of Coordination Tests in the | Coordinated movement requires a functioning cerebellum, spinal cord and peripharal nervous system. Diseases and injuries that damage or destroy any of these structures can lead to ataxia'''.''' | ||
These include: | |||
* [[Traumatic Brain Injury|Traumatic brain injury]] | |||
* [[Alcoholism]] | |||
* [[Communicable Diseases|Infection]] | |||
* [[Neuropathies]] | |||
* [[Spinal Cord Injury|Spinal cord injuries]] | |||
* [[Multiple Sclerosis (MS)]] | |||
* [[Parkinson's - Clinical Presentation|Parkinson's]] | |||
* [[Stroke]] | |||
* [[Transient Ischaemic Attack (TIA)|Transient Ischemic Attack (TIA)]] | |||
* Genetic ataxias eg [[Friedreich's Ataxia|Friedreich’s]] ataxia and [[Wilson's Disease|Wilson’s]] disease | |||
* [[Cerebral Palsy Introduction|Cerebral Palsy]] | |||
* [[Brain Tumors]] | |||
'''Toxins can also cause ataxia.''' | |||
These include: | |||
* Alcohol (most common) | |||
* Seizure medications | |||
* [[Chemotherapy Side Effects and Syndromes|Chemotherapy]] drugs | |||
* Lithium | |||
* [[Opiod Use Disorder|Cocaine and heroin]] | |||
* Sedatives | |||
* Mercury, lead, and other [[Heavy Metal Poisoning|heavy metals]] | |||
* Toluene and other types of solvents<ref>Healthline [https://www.healthline.com/health/movement-uncoordinated What is uncoordinated movement] Available from: https://www.healthline.com/health/movement-uncoordinated (last accessed 14.6.2019)</ref> | |||
== Examples of Coordination Tests in the Upper Limb == | |||
In the following tests, you will be looking for signs of Intention tremors and Decomposition of movements or Dysmetria: in the form of hypermetria or hypometria | In the following tests, you will be looking for signs of Intention tremors and Decomposition of movements or Dysmetria: in the form of hypermetria or hypometria | ||
* Finger-to-nose test - The shoulder is abducted to 90<sup>o</sup> with the elbow extended, the patient is asked to bring tip of the index finger to the tip of nose.Finger to therapist finger: the patient and the therapist site opposite to each other, the therapist index finger is held in front of the patient, the patient is asked to touch the tip of the index finger to the therapist index finger. | * Finger-to-nose test - The shoulder is abducted to 90<sup>o</sup> with the elbow extended, the patient is asked to bring tip of the index finger to the tip of nose.Finger to therapist finger: the patient and the therapist site opposite to each other, the therapist index finger is held in front of the patient, the patient is asked to touch the tip of the index finger to the therapist index finger. | ||
| Line 57: | Line 103: | ||
* Buttoning and unbuttoning test. | * Buttoning and unbuttoning test. | ||
== Examples of Coordination Tests in the lower limb == | == Examples of Coordination Tests in the Lower Limb == | ||
* Walking along a straight line. Foot close to foot:In case of cerebellar lesion, there is deviation of gait | |||
* [https://physio-pedia.com/Romberg_Test?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#contents Rom-berg test]: Ask the patient to stand with heels together. Swaying or loss of balance occurs while his eyes are open or closed. | |||
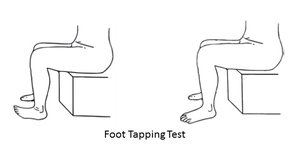
* [https://www.physio-pedia.com/Lower_limb_motor_coordination# Foot tapping test]<ref>Gunzler SA, Pavel M, Koudelka C, Carlson NE, Nutt JG. [https://europepmc.org/article/med/18978495 Foot-tapping rate as an objective outcome measure for Parkinson disease clinical trials]. Clinical Neuropharmacology. 2009 Mar 1;32(2):97-102.</ref> <ref>Enoki H, Tani T, Ishida K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6698509/ Foot tapping test as part of routine neurologic examination in degenerative compression myelopathies: A significant correlation between 10-sec foot-tapping speed and 30-m walking speed]. Spine surgery and related research. 2019:2018-0033.</ref>: The subject sits on a chair with adjustable height so that the bilateral soles made contact with the floor, and the hip and knee joints flexed at approximately 90°. He/She moves his/her toes up and down repeatedly to tap the floor as fast and as vigorously as possible for 10 sec with the heels planted on the floor. The test is performed for both sides separately. The examiner counts the number of taps for each side. | |||
* [https://www.physio-pedia.com/Lower_limb_motor_coordination# Lower Extremity Motor Coordination Test (LEMOCOT)] <ref>Desrosiers J, Rochette A, Corriveau H. [https://www.archives-pmr.org/article/S0003-9993(04)01386-3/fulltext Validation of a new lower-extremity motor coordination test.] Archives of physical medicine and rehabilitation. 2005 May 1;86(5):993-8.</ref>: The subject sits on a height adjustable chair with their feet resting flat on a thin rigid foam, heels on the proximal target, and knees at 90<sup>0</sup> of flexion. Then, after a familiarization trial, he/she is instructed to alternately touch the proximal and distal targets placed 30 cm apart with their big toe for 20sec. The number of touched targets in 20sec is recorded for the motor coordination of the lower limb. | |||
[[File:Foot tapping test 2.png|left|thumb]] | |||
[[File:Lower Extremity Motor Coordination Test.png|thumb|center|Lower Extremity Motor Coordination Test]] | |||
== Coordination Tests for Athletes / Everyday Sports Person == | |||
Many high level tests also exist to help assess and improve an athletes skills and performance e.g. Stick Flip Coordination Test; Wall-Toss Test; Block Transfer; Soda Pop Test; Plate Tapping; Light Board; Test Heel-to-knee test. | |||
The below video shows an athlete going through a series of high end coordination tests | |||
{{#ev:youtube|https://www.youtube.com/watch?v=A711aXacVww|width}}<ref>APA Coordination profile Available from: https://www.youtube.com/watch?v=A711aXacVww (last accessed 13.6.2019)</ref> | |||
== General Principles of Coordination Exercises Involve == | == General Principles of Coordination Exercises Involve == | ||
| Line 73: | Line 127: | ||
# When ever a new movement is trained, various inputs are given, like instruction(auditory), sensory stimulation(touch) ,or positions in which the patient can view the movement (visual stimulation) to enhance motor performance.<ref name=":0" /> | # When ever a new movement is trained, various inputs are given, like instruction(auditory), sensory stimulation(touch) ,or positions in which the patient can view the movement (visual stimulation) to enhance motor performance.<ref name=":0" /> | ||
== Therapeutic Exercises Used to Improve Coordination == | == Physiotherapy - Therapeutic Exercises Used to Improve Coordination == | ||
There are | There are many interventions that can be utilised to improve coordination, such as: | ||
* [[Tai Chi and the Older Person|Tai Chi]] | * [[Tai Chi and the Older Person|Tai Chi]] | ||
* [[Otago Exercise Programme|Otago Exercise Program]] | * [[Pilates]] | ||
* [[Yoga]] | |||
* [[Otago Exercise Programme|Otago Exercise Program]] and use of [[Balance Boards]] | |||
* Neuromuscular coordination exercises. Check out the advanced examples of these below. | * Neuromuscular coordination exercises. Check out the advanced examples of these below. | ||
{{#ev:youtube|https://www.youtube.com/watch?v=ktWVZ1gkW_c|width}}<ref>UEFA Neuromuscular coordination’s exercises Available from: https://www.youtube.com/watch?v=ktWVZ1gkW_c (last accessed 11.6.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=ktWVZ1gkW_c|width}}<ref>UEFA Neuromuscular coordination’s exercises Available from: https://www.youtube.com/watch?v=ktWVZ1gkW_c (last accessed 11.6.2019)</ref> | ||
* Proprioceptive Neuromuscular Facilitation. The below video shows PNF | * Proprioceptive Neuromuscular Facilitation. The below video shows PNF in use | ||
{{#ev:youtube|https://www.youtube.com/watch?v=03YaX9qXtdw|width}}<ref>physio classroom RHYTHMIC INITIATION TECHNIQUE : PNF THERAPY PART-4 Available from: https://www.youtube.com/watch?v=03YaX9qXtdw (last accessed 11.6.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=03YaX9qXtdw|width}}<ref>physio classroom RHYTHMIC INITIATION TECHNIQUE : PNF THERAPY PART-4 Available from: https://www.youtube.com/watch?v=03YaX9qXtdw (last accessed 11.6.2019)</ref> | ||
* Neurophysiological Basis of Developmental Techniques | * Neurophysiological Basis of Developmental Techniques | ||
* Sensory Integrative Therapy | * Sensory Integrative Therapy | ||
* Frenkel’s Exercises | * Frenkel’s Exercises {{#ev:youtube|https://www.youtube.com/watch?v=R83KEKtGcTQ|width}}<ref>Frenkel exercises in rehab Wohl Physiotherapy Available from: https://www.youtube.com/watch?v=R83KEKtGcTQ (last accessed 11.6.2019)</ref> | ||
== | == Evidence == | ||
There is a lot of good evidence for the inclusion of coordination exercises for a whole raft of conditions. | |||
A Cochrane review (2015) into the effectiveness of Pilates in [[Low Back Pain|low back pain]] found low to moderate quality evidence for [[Pilates]] in treating low back pain (being more effective intervention than minimal intervention in the short and intermediate term reducing pain intensity and disability, with most of the effect sizes being considered medium). <ref>Yamato TP, Maher CG, Saragiotto BT, Hancock MJ, Ostelo RW, Cabral CM, Costa LC, Costa LO. Pilates for low back pain. Cochrane Database of Systematic Reviews. 2015(7). Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010265.pub2/media/CDSR/CD010265/CD010265.pdf</ref> | |||
A 2015 study investigating the effect of coordination movement using the Proprioceptive Neuromuscular Facilitation (PNF) pattern underwater on the balance and gait of stroke patients found that coordination movement using the PNF pattern beneficial. It can be an appropriate therapy method for stroke patients who have problems with gait because of declined weight support and balancing ability. Improvements were found in both functional reach and Berg Balance Test (BBT).<ref>Kim K, Lee DK, Jung SI. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713774/ Effect of coordination movement using the PNF pattern underwater on the balance and gait of stroke patients]. Journal of physical therapy science. 2015;27(12):3699-701. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713774/ (last accessed 12.6.2019)</ref> | |||
A 2011 study entitled "Effectiveness of coordination exercise in improving cognitive function in older adults: a prospective study" found that low-intensity level mind-body exercise could be beneficial to the cognitive functioning of older adults.<ref>Kwok TC, Lam KC, Wong PS, Chau WW, Yuen KS, Ting KT, Chung EW, Li JC, Ho FK. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3212417/ Effectiveness of coordination exercise in improving cognitive function in older adults: a prospective study.] Clinical interventions in aging. 2011;6:261. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3212417/ (last accessed 12.6.2019)</ref> | |||
A study onto the effect of coordination training with tennis players found that coordination training program help athletes to learn and perform the forehand and backhand tennis skills better.<ref>Zetou E, Vernadakis N, Tsetseli M, Kampas A, Michalopoulou M. [http://thesportjournal.org/article/the-effect-of-coordination-training-program-on-learning-tennis-skills/ The effect of coordination training program on learning tennis skills]. The Sport Journal. 2012 Jan 1;15(1). Available from: http://thesportjournal.org/article/the-effect-of-coordination-training-program-on-learning-tennis-skills/ (last accessed 13.6.2019)</ref> | |||
A 2015 study into the effectiveness of a sensory integration program in motor skills in children with autism concluded that it was an effective treatment helping autistic children to become more independent and participate in everyday activities.<ref>Karim AE, Mohammed AH. [https://www.sciencedirect.com/science/article/pii/S1110863015000038 Effectiveness of sensory integration program in motor skills in children with autism]. Egyptian Journal of Medical Human Genetics. 2015;16(4):375-80. Available from: https://www.sciencedirect.com/science/article/pii/S1110863015000038 (last accessed 12.6.2019)</ref> | |||
A study into the effects of Tai Chi Chuan (TCC) Coordination exercise on elderly people concluded that " elderly people who regularly practice TCC show better postural stability in the more challenging conditions than those who do not (e.g, conditions with simultaneous disturbance of vision and proprioception). TCC as a coordination exercise may reduce the risk of falling by maintaining the ability of posture control. TCC is strongly recommended as a regimen of coordination exercise to prevent the elderly from falling."<ref>Wong AM, Lin YC, Chou SW, Tang FT, Wong PY. [https://www.archives-pmr.org/article/S0003-9993(01)13337-X/fulltext#s0060 Coordination exercise and postural stability in elderly people: effect of Tai Chi Chuan]. Archives of physical medicine and rehabilitation. 2001 May 1;82(5):608-12. Available from: https://www.archives-pmr.org/article/S0003-9993(01)13337-X/fulltext#s0060 (last accessed 12.6.2019)</ref> | |||
A study involving stroke patients and the effectiveness of Frenkels exercises found significant gains in relation to coordination, balance and functional activities with the inclusion of Frenkel exercises in physical therapy approach. <ref>Pin, Alessandro & Nascimento, Rosiane & Gonçalves da Costa, Jonathas & Bruno Ferro, Sidney & Santos, Marcelo. (2011). [https://www.researchgate.net/publication/259969581_Frenkel_Exercises_in_rehabilitation_after_AVE_hemorrhagic_stroke_with_involvement_cerebellar_a_case_report Frenkel Exercises in rehabilitation after AVE hemorrhagic stroke with involvement cerebellar: a case report.] Fisioterapia Ser. 6. 37 - 40. Available from: https://www.researchgate.net/publication/259969581_Frenkel_Exercises_in_rehabilitation_after_AVE_hemorrhagic_stroke_with_involvement_cerebellar_a_case_report (last accessed 12.6.2019)</ref> | |||
== References: == | == References: == | ||
| Line 146: | Line 167: | ||
[[Category:Exercise Therapy]] | [[Category:Exercise Therapy]] | ||
[[Category:Balance]] | [[Category:Balance]] | ||
[[Category: | [[Category:Older People/Geriatrics - Interventions]] | ||
<references /> | <references /> | ||
Latest revision as of 07:24, 1 April 2022
Top Contributors -Rewan Aloush, Lucinda hampton, Joseph Olamide, Kim Jackson, Rachael Lowe, Joao Costa, Leana Louw, Amanda Ager and Lauren Lopez
Introduction[edit | edit source]
The definition of coordination is the ability to execute smooth, accurate, controlled motor responses (optimal interaction of muscle function).
- Coordination is the ability to select the right muscle at the right time with proper intensity to achieve proper action.
- Coordinated movement is characterized by appropriate speed, distance, direction, timing and muscular tension.
It is the process that results in activation of motor units of multiple muscles with simultaneous inhibition of all other muscles in order to carry out a desired activity.[1]
The cerebellum is the primary centre in the brain for coordination for movement and the ability to execute smooth accurate motor response.
For coordinated movements to occurs all the below systems are involved
- Cerebellum
- Vestibular system
- Motor system.
- Flexibility and ROM.
- Deep sensations.
- Vision.
Image: Cerebellum (highlighted in green) - sagittal view[2]
Components of Coordinated Movement[edit | edit source]
Coordinated movement is dependent on:
- Volition: is the ability to initiate, maintain or stop an activity or motion.
- Perception: in tact proprioception and subcortical centres to integrate motor impulses and the sensory feedback. When proprioception is affected it is compensated with visual feedback.
- Engram: A postulated physical or biochemical change in neural tissue that represents a memory[3]. Research proved that high repetitions of precise performance must be performed in order to develop an engram.A 1980 study concluded "Thousands of repetitions are required to begin to form an engram and millions of repetitions are necessary to perfect it. Coordination is developed in proportion to the number of repetitions of an engram practiced just below the maximal level of ability to perform."[4]
Types of Coordination[edit | edit source]
Motor coordination to complete a task a collaboration of three skills:
- Fine Motor Skills
- Require coordinated movement of small muscles (hands, face).
- Examples: include writing, drawing, buttoning a shirt, blowing bubbles
- Gross Motor Skills
- Require coordinated movement of large muscles or groups of muscles (trunk, extremities).
- Examples: include walking, running, lifting activities.
- Hand-eye Skills
- The ability of the visual system to coordinate visual information. Received and then control or direct the hands in the accomplishment of a task.
- Examples : include catching a ball,sewing,computer mouse use.[1]
Causes of Coordination Impairments[edit | edit source]
Uncoordinated movement or coordination impairment is known medically known as ataxia. There are a number of known causes for ataxia. They range from chronic conditions to sudden onset. However, most conditions will relate to damage or degeneration of the cerebellum.
Coordinated movement requires a functioning cerebellum, spinal cord and peripharal nervous system. Diseases and injuries that damage or destroy any of these structures can lead to ataxia.
These include:
- Genetic ataxias eg Friedreich’s ataxia and Wilson’s disease
Toxins can also cause ataxia.
These include:
- Alcohol (most common)
- Seizure medications
- Chemotherapy drugs
- Lithium
- Sedatives
- Mercury, lead, and other heavy metals
- Toluene and other types of solvents[5]
Examples of Coordination Tests in the Upper Limb[edit | edit source]
In the following tests, you will be looking for signs of Intention tremors and Decomposition of movements or Dysmetria: in the form of hypermetria or hypometria
- Finger-to-nose test - The shoulder is abducted to 90o with the elbow extended, the patient is asked to bring tip of the index finger to the tip of nose.Finger to therapist finger: the patient and the therapist site opposite to each other, the therapist index finger is held in front of the patient, the patient is asked to touch the tip of the index finger to the therapist index finger.
- Finger-to-finger test - Both shoulders are abducted to bring both the elbow extended, the patient is asked to bring both the hand toward the midline and approximate the index finger from opposing hand
- Finger-to-doctor's finger test - the patient alternately touch the tip of the nose and the tip of the therapist's finger with the index finger.
- Adiadokokinesia or dysdiadokokinesia - The patient asked to do rapidly alternating movement e.g. forearm supination and pronation, hand tapping.
- Rebound phenomena - The patient with his elbow fixed, flex it against resistance. When the resistance is suddenly released the patient's forearm flies upward and may hit his face or shoulder.
- Buttoning and unbuttoning test.
Examples of Coordination Tests in the Lower Limb[edit | edit source]
- Walking along a straight line. Foot close to foot:In case of cerebellar lesion, there is deviation of gait
- Rom-berg test: Ask the patient to stand with heels together. Swaying or loss of balance occurs while his eyes are open or closed.
- Foot tapping test[6] [7]: The subject sits on a chair with adjustable height so that the bilateral soles made contact with the floor, and the hip and knee joints flexed at approximately 90°. He/She moves his/her toes up and down repeatedly to tap the floor as fast and as vigorously as possible for 10 sec with the heels planted on the floor. The test is performed for both sides separately. The examiner counts the number of taps for each side.
- Lower Extremity Motor Coordination Test (LEMOCOT) [8]: The subject sits on a height adjustable chair with their feet resting flat on a thin rigid foam, heels on the proximal target, and knees at 900 of flexion. Then, after a familiarization trial, he/she is instructed to alternately touch the proximal and distal targets placed 30 cm apart with their big toe for 20sec. The number of touched targets in 20sec is recorded for the motor coordination of the lower limb.
Coordination Tests for Athletes / Everyday Sports Person[edit | edit source]
Many high level tests also exist to help assess and improve an athletes skills and performance e.g. Stick Flip Coordination Test; Wall-Toss Test; Block Transfer; Soda Pop Test; Plate Tapping; Light Board; Test Heel-to-knee test.
The below video shows an athlete going through a series of high end coordination tests
General Principles of Coordination Exercises Involve[edit | edit source]
- Constant repetition of a few motor activities
- Use of sensory cues (tactile, visual, proprioceptive) to enhance motor performance
- Increase of speed of the activity over time
- Activities are broken down into components that are simple enough to be performed correctly.
- Assistance is provided when ever necessary.
- The patient therefore should have a short rest after two or three repetitions, to avoid fatigue.
- High repetition of precise performance must be performed for the engram to form.
- When ever a new movement is trained, various inputs are given, like instruction(auditory), sensory stimulation(touch) ,or positions in which the patient can view the movement (visual stimulation) to enhance motor performance.[1]
Physiotherapy - Therapeutic Exercises Used to Improve Coordination[edit | edit source]
There are many interventions that can be utilised to improve coordination, such as:
- Tai Chi
- Pilates
- Yoga
- Otago Exercise Program and use of Balance Boards
- Neuromuscular coordination exercises. Check out the advanced examples of these below.
- Proprioceptive Neuromuscular Facilitation. The below video shows PNF in use
- Neurophysiological Basis of Developmental Techniques
- Sensory Integrative Therapy
- Frenkel’s Exercises [12]
Evidence[edit | edit source]
There is a lot of good evidence for the inclusion of coordination exercises for a whole raft of conditions.
A Cochrane review (2015) into the effectiveness of Pilates in low back pain found low to moderate quality evidence for Pilates in treating low back pain (being more effective intervention than minimal intervention in the short and intermediate term reducing pain intensity and disability, with most of the effect sizes being considered medium). [13]
A 2015 study investigating the effect of coordination movement using the Proprioceptive Neuromuscular Facilitation (PNF) pattern underwater on the balance and gait of stroke patients found that coordination movement using the PNF pattern beneficial. It can be an appropriate therapy method for stroke patients who have problems with gait because of declined weight support and balancing ability. Improvements were found in both functional reach and Berg Balance Test (BBT).[14]
A 2011 study entitled "Effectiveness of coordination exercise in improving cognitive function in older adults: a prospective study" found that low-intensity level mind-body exercise could be beneficial to the cognitive functioning of older adults.[15]
A study onto the effect of coordination training with tennis players found that coordination training program help athletes to learn and perform the forehand and backhand tennis skills better.[16]
A 2015 study into the effectiveness of a sensory integration program in motor skills in children with autism concluded that it was an effective treatment helping autistic children to become more independent and participate in everyday activities.[17]
A study into the effects of Tai Chi Chuan (TCC) Coordination exercise on elderly people concluded that " elderly people who regularly practice TCC show better postural stability in the more challenging conditions than those who do not (e.g, conditions with simultaneous disturbance of vision and proprioception). TCC as a coordination exercise may reduce the risk of falling by maintaining the ability of posture control. TCC is strongly recommended as a regimen of coordination exercise to prevent the elderly from falling."[18]
A study involving stroke patients and the effectiveness of Frenkels exercises found significant gains in relation to coordination, balance and functional activities with the inclusion of Frenkel exercises in physical therapy approach. [19]
References:[edit | edit source]
- ↑ 1.0 1.1 1.2 Slide player Coordination exercises Available from: http://slideplayer.com/slide/4638093/ (last accessed 11.6.2019)
- ↑ Cerebellum (highlighted in green) - sagittal view image - © Kenhub https://www.kenhub.com/en/library/anatomy/cerebellum-and-brainstem
- ↑ Glosby Engram in English Available from: https://en.glosbe.com/en/en/Engram (last accessed 13.6.2019)
- ↑ Kottke FJ. From reflex to skill: the training of coordination. Archives of physical medicine and rehabilitation. 1980 Dec;61(12):551-61. Available from: https://www.ncbi.nlm.nih.gov/pubmed/7458618 (last accessed 13.6.2019)
- ↑ Healthline What is uncoordinated movement Available from: https://www.healthline.com/health/movement-uncoordinated (last accessed 14.6.2019)
- ↑ Gunzler SA, Pavel M, Koudelka C, Carlson NE, Nutt JG. Foot-tapping rate as an objective outcome measure for Parkinson disease clinical trials. Clinical Neuropharmacology. 2009 Mar 1;32(2):97-102.
- ↑ Enoki H, Tani T, Ishida K. Foot tapping test as part of routine neurologic examination in degenerative compression myelopathies: A significant correlation between 10-sec foot-tapping speed and 30-m walking speed. Spine surgery and related research. 2019:2018-0033.
- ↑ Desrosiers J, Rochette A, Corriveau H. Validation of a new lower-extremity motor coordination test. Archives of physical medicine and rehabilitation. 2005 May 1;86(5):993-8.
- ↑ APA Coordination profile Available from: https://www.youtube.com/watch?v=A711aXacVww (last accessed 13.6.2019)
- ↑ UEFA Neuromuscular coordination’s exercises Available from: https://www.youtube.com/watch?v=ktWVZ1gkW_c (last accessed 11.6.2019)
- ↑ physio classroom RHYTHMIC INITIATION TECHNIQUE : PNF THERAPY PART-4 Available from: https://www.youtube.com/watch?v=03YaX9qXtdw (last accessed 11.6.2019)
- ↑ Frenkel exercises in rehab Wohl Physiotherapy Available from: https://www.youtube.com/watch?v=R83KEKtGcTQ (last accessed 11.6.2019)
- ↑ Yamato TP, Maher CG, Saragiotto BT, Hancock MJ, Ostelo RW, Cabral CM, Costa LC, Costa LO. Pilates for low back pain. Cochrane Database of Systematic Reviews. 2015(7). Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010265.pub2/media/CDSR/CD010265/CD010265.pdf
- ↑ Kim K, Lee DK, Jung SI. Effect of coordination movement using the PNF pattern underwater on the balance and gait of stroke patients. Journal of physical therapy science. 2015;27(12):3699-701. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713774/ (last accessed 12.6.2019)
- ↑ Kwok TC, Lam KC, Wong PS, Chau WW, Yuen KS, Ting KT, Chung EW, Li JC, Ho FK. Effectiveness of coordination exercise in improving cognitive function in older adults: a prospective study. Clinical interventions in aging. 2011;6:261. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3212417/ (last accessed 12.6.2019)
- ↑ Zetou E, Vernadakis N, Tsetseli M, Kampas A, Michalopoulou M. The effect of coordination training program on learning tennis skills. The Sport Journal. 2012 Jan 1;15(1). Available from: http://thesportjournal.org/article/the-effect-of-coordination-training-program-on-learning-tennis-skills/ (last accessed 13.6.2019)
- ↑ Karim AE, Mohammed AH. Effectiveness of sensory integration program in motor skills in children with autism. Egyptian Journal of Medical Human Genetics. 2015;16(4):375-80. Available from: https://www.sciencedirect.com/science/article/pii/S1110863015000038 (last accessed 12.6.2019)
- ↑ Wong AM, Lin YC, Chou SW, Tang FT, Wong PY. Coordination exercise and postural stability in elderly people: effect of Tai Chi Chuan. Archives of physical medicine and rehabilitation. 2001 May 1;82(5):608-12. Available from: https://www.archives-pmr.org/article/S0003-9993(01)13337-X/fulltext#s0060 (last accessed 12.6.2019)
- ↑ Pin, Alessandro & Nascimento, Rosiane & Gonçalves da Costa, Jonathas & Bruno Ferro, Sidney & Santos, Marcelo. (2011). Frenkel Exercises in rehabilitation after AVE hemorrhagic stroke with involvement cerebellar: a case report. Fisioterapia Ser. 6. 37 - 40. Available from: https://www.researchgate.net/publication/259969581_Frenkel_Exercises_in_rehabilitation_after_AVE_hemorrhagic_stroke_with_involvement_cerebellar_a_case_report (last accessed 12.6.2019)