Types of Rheumatic Disease
Original Editor - Khloud Shreif
Top Contributors - Khloud Shreif, Lucinda hampton and Vidya Acharya
Introduction[edit | edit source]
Historically, "rheumatism" was a term used to describe a range of painful conditions affecting muscles, tendons, joints, and bones. Nowadays, we prefer the more precise term "rheumatic disease." which are a group of inflammatory, often autoimmune, conditions that affect joints, muscles, bones, and organs.[1] Osteoarthritis and rheumatoid arthritis are the most common of the rheumatic diseases but the group of diseases is much more, encompassing over 200 different conditions.
Rheumatic diseases can be divided into subsets:
- Autoimmune disease.
- Autoinflammatory disease.
- Degenerative.
- Metabolic disorders.
Pathogenesis of Rheumatic Disease[edit | edit source]
The pathogenesis of rheumatic disease is still under debate and not totally understood, it is suggested that complex interactions between genetic and environmental. One environmental factor considered is infection, long considered as an important risk and causative factor for rheumatic disease. eg this Epstein-Barr virus (EBV) and the development of systemic lupus erythematosus (SLE).[1] It is postulated that our immune response gets confused and our immune system and inflammation responses get mixed up.
A Little Background (see more details here immune system)
There are different immune types of cells in our body, like T and B cells, monocytes/macrophages, to name a few.
- T cells especially (CD4+ T cells have subsets like Th1, Th2, Th17, and T regulatory cells which are a type of immune cell that plays a crucial role in coordinating the body's immune response. These subsets have distinct functions and are characterized by the specific proteins and molecules they produce and the roles they play in maintaining immune balance [2][3].
- B cells assume a crucial role in the pathogenesis of several rheumatic and immune disorders their primary function involves the production of antibodies (immunoglobulins) in response to pathogens, and their function in these conditions extends beyond antibody generation[4]. These cells have special receptors on their surfaces, these receptors act like switches. When they come into contact with certain things, like antigens or other cells, they turn on and become active..
Hyperactive Immune System
In autoimmune and inflammatory rheumatic conditions, the immune system's cells become hyperactive, releasing a multitude of signaling molecules. These molecules not only summon more immune cells but also trigger inflammation and potential tissue damage. T cells, distributed throughout the body, can become autoreactive, meaning they mistakenly attack the body's own tissues. This can also disrupt the function of regulatory T cells, which normally help keep the immune system in check[2].
In addition to T cells, B cells play a significant role in these conditions. They produce autoantibodies, which erroneously target the body's tissues, leading to inflammation and tissue damage. Furthermore, B cells can produce cytokines, act as antigen-presenting cells to activate other immune cells, and create immune complexes. All of these actions contribute to the immune response and the associated inflammatory processes in these disorders. Picture it as a chain reaction: one switch activates another, setting off a series of events that ultimately impact our genes and drive the development and progression of these conditions.[4].
Targeting B cells directly is a promising approach to treat immune and rheumatic diseases. B-cell depletion therapies have shown success in reducing disease activity by modulating the immune response. Understanding the complex role of B cells in immune regulation and dysregulation is essential for managing these conditions, leading to targeted therapies and ongoing research in the field[4][5].
General Classification Criteria of Rheumatic Diseases[edit | edit source]
There are still no accurate solo diagnostic procedures to diagnose or confirm Rheumatic Diseases, the Classification criteria will help to distinguish between similar diseases and confirm or exclude a specific disease based on specific factors. These criteria are guidelines, not the only way to diagnose. Diagnosis of rheumatic disease can be challenging, it relies on clinical assessment, gathering complete patient history, and carefully evaluating the musculoskeletal system is very important, hence match the findings during clinical examination with lab, X-ray, and sometimes tissue samples to confirm the diagnosis[6].
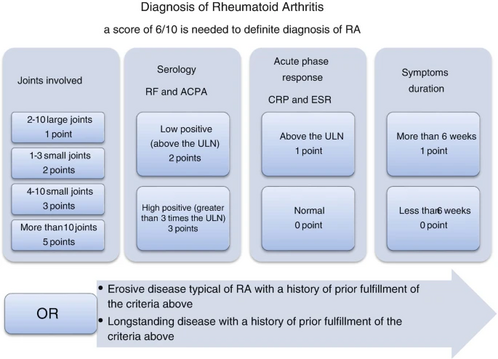
Rheumatoid arthritis classification criteria
In 1987, the American College of Rheumatology (ACR) introduced the initial classification criteria for RA, which required meeting 4 out of 7 criteria for over 6 weeks. Subsequently, a new classification criteria set was developed jointly by ACR/ EULAR in 2010. These updated criteria take into consideration the prognostic markers while maintaining high specificity and sensitivity. This allows for early patient identification and timely treatment with disease-modifying antirheumatic drugs DMARDs or inclusion in clinical trials for new therapies, enhancing care for those with early arthritis and enabling personalized treatment strategies[7].
Systemic Lupus Erythematosus Classification Criteria
In 2012, International Collaborating Clinics (SLICC) improved the 1997 criteria for categorizing lupus patients. These criteria help in research but aren't perfect for diagnosing patients. The new criteria are more sensitive (better at finding lupus cases) but less specific (may include some false positives). To be classified with lupus, a person must meet at least 4 out of 17 criteria, including one clinical and one immunologic sign. If a biopsy confirms lupus in the kidneys and there are positive autoantibodies, that's enough for classification[8].
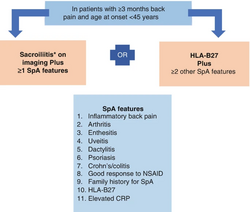
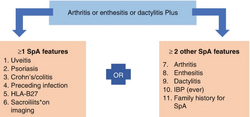
Spondyloarthritis (SpA) includes diseases like ankylosing spondylitis (AS), psoriatic arthritis (PsA), reactive arthritis, enteropathic-related spondylitis. There are different criteria for diagnosing SpA, mainly used in research, but the latest from the Assessment of SpondyloArthritis International Society suggests MRI is better for detecting early disease in the spine and sacroiliac area. They also defined inflammatory back pain and criteria for diagnosing axial and peripheral spondyloarthritis in early phases. ASAS introduced non-radiographic axial spondyloarthritis, which is similar to the radiographic form but lacks findings on plain X-rays and shows less ossification and inflammation on MRIs[9].
Psoriatic arthritis classification criteria
Psoriatic arthritis (PsA) is an inflammatory joint condition with diverse clinical subcategories. Various classification criteria have been proposed but lack widespread validation, complicating the diagnosis, particularly for patterns like seronegative polyarthritis and psoriasis[6].
| Inflammatory articular disease (joint, spine, or entheseal) with ≥ 3 of the following: | ||
|---|---|---|
| 1. Evidence of psoriasis:
(one of a,b,c) |
a. Current psoriasis | Psoriatic skin or scalp disease present today as judged by a rheumatologist or dermatologist |
| b. Personal history of psoriasis | A history of psoriasis that may be obtained from the patient, family doctor, dermatologist, rheumatologist, or other qualified healthcare provider | |
| c. Family history | A history of psoriasis in a first or second-degree relative according to the patient’s reporting. | |
| 2. Psoriatic nail dystrophy | Typical psoriatic nail dystrophy including onycholysis, pitting, and hyperkeratosis observed on current physical examination | |
| 3. A negative rheumatoid factor | By any method except latex but preferably by ELISA or nephelometry, according to the local laboratory reference range | |
| 4. Dactylitis (a or b) | a. Current swelling of entire digit
b. A history of dactylitis recorded by a rhematologist | |
| 5. Radiological evidence of juxta-articular new bone formation | III-defined ossification near joint margins (but excluding osteophyte formation) on plain X-rays of hands or feet | |
Systemic Sclerosis classification criteria
For sclerosis, ACR created criteria for diagnosing systemic sclerosis (SSc) based on skin symptoms. These criteria lacked accuracy for early disease diagnosis. In 2013, the ACR and EULAR collaborated to develop improved criteria to enhance early SSc and limited cutaneous SSc diagnosis, mainly for use in SSc trials, although they may be less suitable for scleroderma-like syndromes.
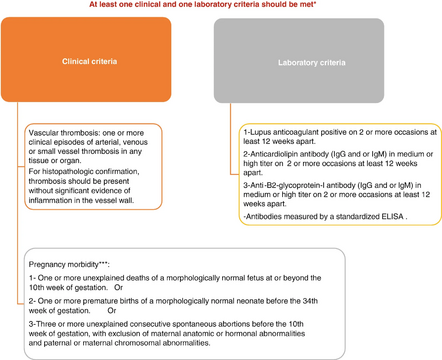
Antiphospholipid syndrome classification criteria
Antiphospholipid syndrome (APS) is an autoimmune disease known for causing blood clots in arteries and veins, as well as adverse pregnancy outcomes, associated with the presence of antiphospholipid antibodies (aPL), these antibodies can also be found in healthy individuals[10]. The first classification criteria for APS were proposed in 1998 in Japan, involving positive antibody testing and at least one clinical manifestation of the disease. Due to its limitation in 2006, the criteria were modified in Sydney to address these limitations and improve accuracy in diagnosing APS, however, we need more understanding of the pathogenesis, and there i a need to detect laboratory studies to detect who are at risk[11].
Differences between autoimmune, autoinflammatory, metabolic, and anti-inflammatory disorders[edit | edit source]
- Autoimmune Disorders: characterized by the immune system mistakenly identifying the body's own tissues and cells as foreign invaders, resulting in an abnormal and overactive immune response against self-antigens. This immune dysregulation leads to chronic inflammation and damage to various organs and tissues. Examples of autoimmune disorders include rheumatoid arthritis, systemic lupus erythematosus (SLE) and dermatomyositis[12].
- Autoinflammatory disorders: characterized by recurrent episodes of inflammation, typically without a clear autoimmune or infection-triggered cause, many of autoinflammatory disorders have a genetic basis and tend to run in families, they result from a dysregulation of the immune response itself. Examples of autoinflammatory disorders include Familial Mediterranean fever (FMF).
- Metabolic disorders: involve disruptions in the body's normal metabolic processes. They affect functions such as energy production, nutrient storage, and hormone regulation, but they are not primarily related to immune responses. However metabolic disorders can indirectly impact the immune system due to imbalances in biochemical pathways, they are distinct from autoimmune disorders. Diabetes, both type 1 and type 2, is an example of metabolic disorder[13].
- Anti-inflammatory disorders: characterized by chronic inflammation even when there's no infection or injury. Normally, inflammation helps us fight infections and heal wounds, but in these disorders, the immune system gets confused and keeps causing inflammation that can harm the body. For example asthma, crohn's disease, and psoriasis.
| Autoimmune | Autoinflammatory | Degenerative and metabolic disorders |
|---|---|---|
|
|
|
Rheumatoid Arthritis and Osteoarthritis[edit | edit source]
| Rheumatoid Arthritis | Osteoarthritis |
|---|---|
|
|
| N.B: Arthritis is a common feature in many rheumatic conditions, but it is not synonymous with rheumatic disease.
Rheumatic diseases are a group of conditions that can involve arthritis as a symptom, while arthritis is a more specific term describing joint inflammation that can occur in various rheumatic diseases. | |
References[edit | edit source]
- ↑ 1.0 1.1 Dong L, Umehara H, Zhong J. Rheumatic Diseases and Infection. Frontiers in Medicine. 2022 Jun 1;9:941678.Available:https://www.frontiersin.org/articles/10.3389/fmed.2022.941678/full (accessed 13.9.2023)
- ↑ 2.0 2.1 Milojevic D, Nguyen KD, Wara D, Mellins ED. Regulatory T cells and their role in rheumatic diseases: a potential target for novel therapeutic development. Pediatric Rheumatology. 2008 Dec;6(1):1-3.
- ↑ Skapenko A, Leipe J, Lipsky PE, Schulze-Koops H. The role of the T cell in autoimmune inflammation. Arthritis research & therapy. 2005 Mar;7(2):1-1.
- ↑ 4.0 4.1 4.2 Wu F, Gao J, Kang J, Wang X, Niu Q, Liu J, Zhang L. B Cells in Rheumatoid Arthritis: Pathogenic Mechanisms and Treatment Prospects. Frontiers in Immunology. 2021 Sep 28;12:750753.
- ↑ Merino‐Vico A, Frazzei G, van Hamburg JP, Tas SW. Targeting B cells and plasma cells in autoimmune diseases: From established treatments to novel therapeutic approaches. European journal of immunology. 2023 Jan;53(1):2149675.
- ↑ 6.0 6.1 Hassan R, Faruqui H, Alquraa R, Eissa A, Alshaiki F, Cheikh M. Classification criteria and clinical practice guidelines for rheumatic diseases. Skills in Rheumatology. 2021:521.
- ↑ Britsemmer K, Ursum J, Gerritsen M, van Tuyl L, van Schaardenburg D. Validation of the 2010 ACR/EULAR classification criteria for rheumatoid arthritis: slight improvement over the 1987 ACR criteria. Annals of the rheumatic diseases. 2011 Aug 1;70(8):1468-70.
- ↑ Petri M, Orbai AM, Alarcon GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg DA, Wallace DJ, Nived O, Sturfelt GK. Derivation and validation of systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. In2011 ACR/ARHP Annual Meeting 2011 Nov 4 (pp. S669-S670). WILEY-BLACKWELL.
- ↑ Rudwaleit MV, van der Heijde D, Landewé R, Akkoc N, Brandt J, Chou CT, Dougados M, Huang F, Gu J, Kirazli Y, Van den Bosch F. The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Annals of the rheumatic diseases. 2011 Jan 1;70(1):25-31.
- ↑ Gómez-Puerta JA, Cervera R. Diagnosis and classification of the antiphospholipid syndrome. Journal of autoimmunity. 2014 Feb 1;48:20-5.
- ↑ Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera RH, Derksen RH, de Groot PG, Koike T, Meroni PL, Reber G. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). Journal of thrombosis and haemostasis. 2006 Feb 1;4(2):295-306.
- ↑ Davidson A, Diamond B. Autoimmune diseases. New England Journal of Medicine. 2001 Aug 2;345(5):340-50.
- ↑ American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes care. 2014 Jan 1;37(Supplement_1):S81-90.