Pneumonia: Difference between revisions
No edit summary |
No edit summary |
||
| (13 intermediate revisions by the same user not shown) | |||
| Line 7: | Line 7: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Pneumonia | [[File:Respiratory Tract.jpeg|thumb|Increased mucus in lungs]] | ||
Pneumonia, a general term, refers to an [[Infectious Disease|infection]] within the lung. It is caused by a [[Bacterial Infections|bacterial]] or [[Viral Infections|viral]] infection that becomes purulent and filling the [[alveoli]] (may become solid).<ref name=":0">Radiopedia Pneumonia Available: https://radiopaedia.org/articles/pneumonia (accessed 25.5.2021)</ref> | |||
== Aetiology == | == Aetiology == | ||
Pneumonias can be classified by: | |||
Infective Agent: | Infective Agent: | ||
3. | # Bacterial Pneumonia occurs when pneumonia-causing bacteria masses and multiplies in the lungs. The alveoli become inflamed and pus is produced, which spreads around the lungs<ref name=":3">Smith, B., & Ball, V. (1998). Cardiovascular/Respiratory Physiotherapy. Mosby International Limited: Italy</ref> eg Streptococcus pneumonia, Staphylococcus aureus, Haemophilus influenza, legionella pneumophilia and Methicillin resistant staphylococcus aureus (MRSA)<ref name=":2">Healthscout. (2009). ''Health Encyclopedia - Diseases and Conditions: Pneumonia''. Retrieved April 8, 2009 from http://www.healthscout.com/ency/68/205/main.html</ref><ref>Bartleby. ''The Lungs''. Retrieved April 8, 2009 from http://education.yahoo.com/reference/gray/subjects/subject/240</ref> | ||
# Fungal pneumonia This typically occurs in people who have a weakened immune system or other underlying health issues. This is usually inhaled from the environment and does not spread from person to person. eg [[Pneumocystis Jirovecii Pneumonia]].<ref name=":1">Health-cares. (2005). ''What is pneumonia?'' Retrieved February 13, 2009 from http://respiratory-lung.health-cares.net/pneumonia.php</ref> | |||
# Mycobacterial pneumonia | |||
# Viral Pneumonia - believed to be the cause of half of all cases of pneumonia. The viruses invade the lungs and then multiply- causing inflammation. eg [[COVID-19]], Middle East respiratory syndrome coronavirus (MERS-CoV) infection, severe acute respiratory syndrome (SARS)], varicella pneumonia,Influenza type A or B, rhinoviruses adenoviruses, respiratory syncytial virus (more common in infants and children)<ref name=":2" /> | |||
Setting of Infection (how aquired): | Setting of Infection (how aquired): | ||
# Community-acquired pneumonia (CAP): This is the most common form of pneumonia and describes pneumonia that is acquired outside of a hospital the main causes of CAP are bacteria, viruses and less commonly fungi. In most cases pneumonia is not spread from person to person and quite often is transmitted via droplets in the air, touching contaminated objects, poor hygiene and sharing cups or utensil or from the environment<ref name=":4">Koenig, S., & Truwit, J. (2006). ''Ventilator-associated pneumonia: Diagnosis, treatment and prevention''. Clin Microbiol Rev. 2006 October; 19(4): 637–657. Retrieved April 12, 2009 from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1592694</ref>. | |||
#[[Hospital Acquired Pneumonia|Hospital-acquired pneumonia]] (HAP) eg 1. Ventilator-associated pneumonia (VAP) Biofilm formation on endotracheal tubes (ETTs) is an early and frequent event in mechanically ventilated patients. The [[Biofilms Role in Chronic Infections|biofilm]] is believed to act as a reservoir for infecting microorganisms and contributes to development and relapses of ventilator-associated pneumonia<ref>Thorarinsdottir HR, Kander T, Holmberg A, Petronis S, Klarin B. [https://ccforum.biomedcentral.com/articles/10.1186/s13054-020-03092-1 Biofilm formation on three different endotracheal tubes: a prospective clinical trial].Available from:https://ccforum.biomedcentral.com/articles/10.1186/s13054-020-03092-1 (last accessed 30.6.2020)</ref>; 2. Healthcare-associated pneumonia (HCAP)<ref name=":10">Pahal P, Sharma S. [https://www.ncbi.nlm.nih.gov/books/NBK534295/ Typical Bacterial Pneumonia.]Available from:https://www.ncbi.nlm.nih.gov/books/NBK534295/ (last accessed 29.6.2020)</ref> | |||
# Aspiration pneumonia<ref>Radiopedia [https://radiopaedia.org/articles/pneumonia Pneumonia] Available from:https://radiopaedia.org/articles/pneumonia (last accessed 29.6.2020)</ref> This is commonly caused by inhaling a foreign object, vomit, mucous, bodily fluids, or certain chemicals which causes the bronchial tubes and lungs to become inflamed.<ref name=":1" /> It occurs predominantly in the right lung because its total capacity is greater than that of the left lung.<ref name=":1" /> If large amounts of gastric contents can cause acute respiratory distress within 1 hour. In cases of aspiration immediate physiotherapy can help with secretion clearance | |||
Pathological Description: | |||
= | # Bronchopneumonia | ||
# Lobar pneumonia<ref name=":0" /> | |||
The various causes of pneumonia are discussed below. To interact with the screen below, scroll within screen.<primalpictures id="334087" /> | |||
<primalpictures id="334087" /> | |||
== Defence Against Pneumonia == | |||
The overall function of the immune system is to prevent or limit [[Infectious Disease|infection]]. The Immune response is the body's ability to stay safe by affording protection against harmful agents and involves lines of defense against most microbes as well as specialized and highly specific response to a particular offender. See [[Immune System|here]] for more. | |||
== Epidemiology == | == Epidemiology == | ||
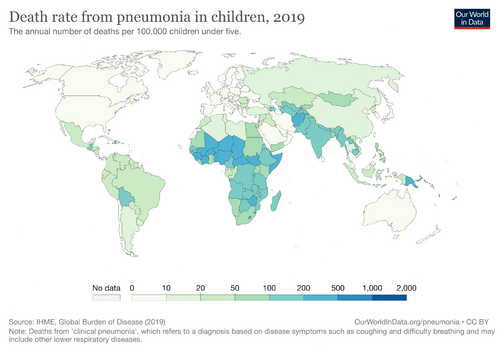
[[File:Pneumonia-death-rates-in-children-under-5.png|right|frameless|499x499px]] | [[File:Pneumonia-death-rates-in-children-under-5.png|right|frameless|499x499px]] | ||
2.5 million people died from pneumonia in 2019, with roughly 33% of these being children younger than 5 years (the leading cause of death for children under 5).<ref>Dadonaite B, Roser M. [https://ourworldindata.org/pneumonia Pneumonia. Our World in Data; 2020] [updated Nov 2019; cited 11 May 2020].Available:https://ourworldindata.org/pneumonia (accessed 24.12.2022)</ref><ref>World health organisation Pneumonia Available:https://www.who.int/health-topics/pneumonia/#tab=tab_1 (accessed 18.12.2022)</ref> | |||
Risk factors include: | |||
# Elderly, infants, young children and those with a weakened [[Immune System|immune system]] . | |||
# Frequent exposure to asbestos and cigarette smoke. | |||
# Developing nations where the medical care may be suboptimal, sanitation is poor, and poverty is prevelent.<ref>news Medical [https://www.news-medical.net/health/Pneumonia-Epidemiology.aspx Pneumonia Epidemiology] Available:https://www.news-medical.net/health/Pneumonia-Epidemiology.aspx (accessed 24.12.2022)</ref> | |||
== Stages of Pneumonia == | == Stages of Pneumonia == | ||
| Line 108: | Line 89: | ||
**[[Auscultation]]- Bronchial breath sounds or fine cracks over the affected area | **[[Auscultation]]- Bronchial breath sounds or fine cracks over the affected area | ||
**Pleural friction rub - an adventitious breath sound heard during auscultation. The sound is caused by the movement of inflamed and roughened pleural surfaces<ref>Adderley N, Sharma S. [[Pleural Friction Rub]]. Accessed 16 March 2020</ref> | **Pleural friction rub - an adventitious breath sound heard during auscultation. The sound is caused by the movement of inflamed and roughened pleural surfaces<ref>Adderley N, Sharma S. [[Pleural Friction Rub]]. Accessed 16 March 2020</ref> | ||
*[[X-Rays|Chest X-rays]] often lag behind the clinical presentation.The X-ray will show decreased lung expansion and patchy opacity on the affected side with ill defined margins<ref>Klein, J. (2008). ''Pneumonia''. Retrieved February 13, 2009 from http://kidshealth.org/PageManager.jsp?dn=KidsHealth&lic=1&ps=107&cat_id=20043&article_set=23001</ref><ref name=":5">Torpy, J. (2007). ''Ventilator associated pneumonia''. Retrieved April 12, 2009 from http://jama.ama-assn.org/cgi/content/full/297/14/1616</ref> | *[[X-Rays|Chest X-rays]] often lag behind the clinical presentation.The X-ray will show decreased lung expansion and patchy opacity on the affected side with ill defined margins<ref>Klein, J. (2008). ''Pneumonia''. Retrieved February 13, 2009 from http://kidshealth.org/PageManager.jsp?dn=KidsHealth&lic=1&ps=107&cat_id=20043&article_set=23001</ref><ref name=":5">Torpy, J. (2007). ''Ventilator associated pneumonia''. Retrieved April 12, 2009 from http://jama.ama-assn.org/cgi/content/full/297/14/1616</ref> | ||
*Sputum samples and blood tests | |||
*Sputum samples and blood tests | |||
== Complications == | == Complications == | ||
Include: [[Pleural Effusion|Pleural effusion]]; Empyema; Lung abscess; Bacteremia; [[Sepsis]]; [[Meningitis]]; [[Septic (Infectious) Arthritis|Septic arthritis]]; [[Endocarditis]] or pericarditis <ref name=":1" /> | |||
== Treatment == | == Treatment == | ||
Pneumonia may be treated with antibiotics, if it is bacterial, preferably amoxicillin dispersible tablets. Most cases of pneumonia require oral antibiotics. Hospitalization is recommended only for severe cases of pneumonia.<ref name=":11" /><primalpictures id="B7FBA8" /> | Pneumonia may be treated with [[antibiotics]], if it is bacterial, preferably amoxicillin dispersible tablets. Most cases of pneumonia require oral antibiotics. Hospitalization is recommended only for severe cases of pneumonia.<ref name=":11">World Health Organisation [https://www.who.int/news-room/fact-sheets/detail/pneumonia Pneumonia] Available from:https://www.who.int/news-room/fact-sheets/detail/pneumonia (last accessed 30.6.2020)</ref><primalpictures id="B7FBA8" /> | ||
== Physiotherapy Management == | == Physiotherapy Management == | ||
[[ | [[Respiratory Physiotherapy|Respiratory physiotherapy]] is a core specialty within the physiotherapy profession and occupies a key role in the management and treatment of patients with [[Respiratory Disorders|respiratory diseases]]. It aims to unclog the patient’s [[Respiratory System|airways]] and help them return to [[Physical Activity|physical activity]] and exertion. The respiratory physiotherapist employs many diverse interventions, including [[Pulmonary Rehabilitation|pulmonary rehabilitation]], [[Early Mobilization in the ICU|early mobilisation]], and airway clearance techniques, all having beneficial effects on the symptoms associated with in this case pneumonia<ref>[[Respiratory Physiotherapy]]</ref>. | ||
Watch this videos (10 minutes) titled "Community Acquired Pneumonia Overview"{{#ev:youtube|4c_ECpAfdSs}} | |||
== Children and Pneumonia == | |||
Children whose immune systems are compromised are at higher risk of developing pneumonia. | |||
Risk Factors: | |||
* Malnutrition/undernourishment; infants who are not exclusively breastfed; immunocompromised children. | |||
* indoor air pollution caused by cooking and heating with biomass fuels (such as wood or dung) | * Environmental: indoor air pollution caused by cooking and heating with biomass fuels (such as wood or dung); living in crowded homes; parental smoking.<ref name=":11" /> | ||
'''Signs and Symptoms in Children:''' the signs and symptoms are similar to that of adults. | |||
*If pneumonia is caused by bacteria, the infected child becomes sick relative quickly and is prone to developing a high fever and rapid breathing. | |||
*If pneumonia is caused by viruses, symptoms may appear gradually and less severe than bacterial pneumonia.<ref name=":8">Kids Health. (2009). ''Pneumonia''. Retrieved April 11, 2009 from http://kidshealth.org/parent/infections/lung/pneumonia.html</ref> | |||
*Increased breath rate: > 60 breaths/min for newborns up to 2 months; > 50 breaths/min for 2 months to 12 months; > 40 breaths/min for a child older than 1 year of age<ref>Drugs information online. (2009). ''Pneumonia in children care Guidelines information''. Retrieved April 11, 2009 from http://www.drugs.com/cg/pneumonia-in-children.html</ref> | |||
'''Prevention:''' Vaccines are usually administered to prevent infection by viruses and bacteria. Kids usually receive routine immunisation against Haemophilus Influenzae and Pertussis at the age of 2 months of age. Some vaccines are also administered against pneumococcus organism, a common cause of pneumonia<ref name=":8" /> | |||
== References == | == References == | ||
<references /> | <references /> | ||
Latest revision as of 07:23, 24 December 2022
Original Editor - The Open Physio project.
Top Contributors - Lucinda hampton, Kim Jackson, Admin, Tony Lowe, Nikhil Benhur Abburi, Adam Vallely Farrell, Vidya Acharya, Rachael Lowe, Evan Thomas, Karen Wilson, Rishika Babburu, Naomi O'Reilly, George Prudden and WikiSysop
Introduction[edit | edit source]
Pneumonia, a general term, refers to an infection within the lung. It is caused by a bacterial or viral infection that becomes purulent and filling the alveoli (may become solid).[1]
Aetiology[edit | edit source]
Pneumonias can be classified by:
Infective Agent:
- Bacterial Pneumonia occurs when pneumonia-causing bacteria masses and multiplies in the lungs. The alveoli become inflamed and pus is produced, which spreads around the lungs[2] eg Streptococcus pneumonia, Staphylococcus aureus, Haemophilus influenza, legionella pneumophilia and Methicillin resistant staphylococcus aureus (MRSA)[3][4]
- Fungal pneumonia This typically occurs in people who have a weakened immune system or other underlying health issues. This is usually inhaled from the environment and does not spread from person to person. eg Pneumocystis Jirovecii Pneumonia.[5]
- Mycobacterial pneumonia
- Viral Pneumonia - believed to be the cause of half of all cases of pneumonia. The viruses invade the lungs and then multiply- causing inflammation. eg COVID-19, Middle East respiratory syndrome coronavirus (MERS-CoV) infection, severe acute respiratory syndrome (SARS)], varicella pneumonia,Influenza type A or B, rhinoviruses adenoviruses, respiratory syncytial virus (more common in infants and children)[3]
Setting of Infection (how aquired):
- Community-acquired pneumonia (CAP): This is the most common form of pneumonia and describes pneumonia that is acquired outside of a hospital the main causes of CAP are bacteria, viruses and less commonly fungi. In most cases pneumonia is not spread from person to person and quite often is transmitted via droplets in the air, touching contaminated objects, poor hygiene and sharing cups or utensil or from the environment[6].
- Hospital-acquired pneumonia (HAP) eg 1. Ventilator-associated pneumonia (VAP) Biofilm formation on endotracheal tubes (ETTs) is an early and frequent event in mechanically ventilated patients. The biofilm is believed to act as a reservoir for infecting microorganisms and contributes to development and relapses of ventilator-associated pneumonia[7]; 2. Healthcare-associated pneumonia (HCAP)[8]
- Aspiration pneumonia[9] This is commonly caused by inhaling a foreign object, vomit, mucous, bodily fluids, or certain chemicals which causes the bronchial tubes and lungs to become inflamed.[5] It occurs predominantly in the right lung because its total capacity is greater than that of the left lung.[5] If large amounts of gastric contents can cause acute respiratory distress within 1 hour. In cases of aspiration immediate physiotherapy can help with secretion clearance
Pathological Description:
- Bronchopneumonia
- Lobar pneumonia[1]
The various causes of pneumonia are discussed below. To interact with the screen below, scroll within screen.
Defence Against Pneumonia[edit | edit source]
The overall function of the immune system is to prevent or limit infection. The Immune response is the body's ability to stay safe by affording protection against harmful agents and involves lines of defense against most microbes as well as specialized and highly specific response to a particular offender. See here for more.
Epidemiology[edit | edit source]
2.5 million people died from pneumonia in 2019, with roughly 33% of these being children younger than 5 years (the leading cause of death for children under 5).[10][11]
Risk factors include:
- Elderly, infants, young children and those with a weakened immune system .
- Frequent exposure to asbestos and cigarette smoke.
- Developing nations where the medical care may be suboptimal, sanitation is poor, and poverty is prevelent.[12]
Stages of Pneumonia[edit | edit source]
Pneumonia has four stages, namely consolidation, red hepatization, grey hepatization and resolution. (may be Lobar Pneumonia or bronchopneumonia, see image R)
- Consolidation
- Occurs in the first 24 hours
- Cellular exudates containing neutrophils, lymphocytes and fibrin replaces the alveolar air
- Capillaries in the surrounding alveolar walls become congested
- The infection spreads to the hilum and pleura fairly rapidly
- Pleurisy occurs
- Marked by coughing and deep breathing[13][14]
- Red Hepatization
- Occurs in the 2-3 days after consolidation
- At this point, the consistency of the lungs resembles that of the liver
- The lungs become hyperaemic
- Alveolar capillaries are engorged with blood
- Fibrinous exudates fill the alveoli
- This stage is "characterized by the presence of many erythrocytes, neutrophils, desquamated epithelial cells, and fibrin within the alveoli"[13][14]
- Grey Hepatization
- Occurs in the 2-3 days after Red Hepatization
- This is an avascular stage
- The lung appears "grey-brown to yellow because of fibrinopurulent exudates, disintegration of red cells, and hemosiderin"
- The pressure of the exudates in the alveoli causes compression of the capillaries
- "Leukocytes migrate into the congested alveoli"[13][14]
- Resolution
- This stage is characterized by the "resorption and restoration of the pulmonary architecture"
- A large number of macrophages enter the alveolar spaces
- Phagocytosis of the bacteria-laden leucocytes occurs
- "Consolidation tissue re-aerates and the fluid infiltrate causes sputum"
- "Fibrinous inflammation may extend to and across the pleural space, causing a rub heard by auscultation, and it may lead to resolution or to organization and pleural adhesions"[13][14]
Signs and Symptoms[edit | edit source]
The signs and symptoms vary according to disease severity. Common symptoms include fever, cough, sputum production (may or may not be present). The color and quality of sputum provide the clue to microbiological etiology.
- Pleuritic chest pain due to localized inflammation of pleura can be seen with any kind of pneumonia but, is more common with lobar pneumonia. Constitutional symptoms such as fatigue, headache, myalgia, and arthralgias can also be seen.
- Severe pneumonia can lead to dyspnea and shortness of breath. In severe cases, confusion, sepsis, and multi-organ failure can also manifest.
- Tachypnea, increased vocal fremitus, egophony (E to A changes), dullness to percussion are the major clinical signs depending on the degree of consolidation and presence/absence of pleural effusion. Chest auscultation reveals crackles, rales, bronchial breath sounds.
- The respiratory rate closely correlates with the degree of oxygenation and, therefore essential in determining the severity. Hypoxia is seen in severe pneumonia, which leads to hyperventilation.[8]
Diagnosis[edit | edit source]
There are several ways to diagnose pneumonia:
- Physical examination
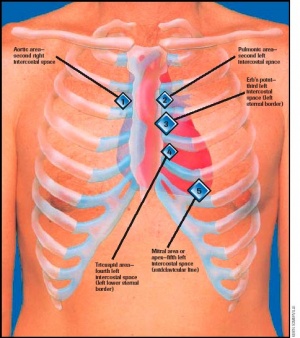
- Auscultation- Bronchial breath sounds or fine cracks over the affected area
- Pleural friction rub - an adventitious breath sound heard during auscultation. The sound is caused by the movement of inflamed and roughened pleural surfaces[15]
- Chest X-rays often lag behind the clinical presentation.The X-ray will show decreased lung expansion and patchy opacity on the affected side with ill defined margins[16][17]
- Sputum samples and blood tests
Complications[edit | edit source]
Include: Pleural effusion; Empyema; Lung abscess; Bacteremia; Sepsis; Meningitis; Septic arthritis; Endocarditis or pericarditis [5]
Treatment[edit | edit source]
Pneumonia may be treated with antibiotics, if it is bacterial, preferably amoxicillin dispersible tablets. Most cases of pneumonia require oral antibiotics. Hospitalization is recommended only for severe cases of pneumonia.[18]
Physiotherapy Management[edit | edit source]
Respiratory physiotherapy is a core specialty within the physiotherapy profession and occupies a key role in the management and treatment of patients with respiratory diseases. It aims to unclog the patient’s airways and help them return to physical activity and exertion. The respiratory physiotherapist employs many diverse interventions, including pulmonary rehabilitation, early mobilisation, and airway clearance techniques, all having beneficial effects on the symptoms associated with in this case pneumonia[19].
Watch this videos (10 minutes) titled "Community Acquired Pneumonia Overview"
Children and Pneumonia[edit | edit source]
Children whose immune systems are compromised are at higher risk of developing pneumonia.
Risk Factors:
- Malnutrition/undernourishment; infants who are not exclusively breastfed; immunocompromised children.
- Environmental: indoor air pollution caused by cooking and heating with biomass fuels (such as wood or dung); living in crowded homes; parental smoking.[18]
Signs and Symptoms in Children: the signs and symptoms are similar to that of adults.
- If pneumonia is caused by bacteria, the infected child becomes sick relative quickly and is prone to developing a high fever and rapid breathing.
- If pneumonia is caused by viruses, symptoms may appear gradually and less severe than bacterial pneumonia.[20]
- Increased breath rate: > 60 breaths/min for newborns up to 2 months; > 50 breaths/min for 2 months to 12 months; > 40 breaths/min for a child older than 1 year of age[21]
Prevention: Vaccines are usually administered to prevent infection by viruses and bacteria. Kids usually receive routine immunisation against Haemophilus Influenzae and Pertussis at the age of 2 months of age. Some vaccines are also administered against pneumococcus organism, a common cause of pneumonia[20]
References[edit | edit source]
- ↑ 1.0 1.1 Radiopedia Pneumonia Available: https://radiopaedia.org/articles/pneumonia (accessed 25.5.2021)
- ↑ Smith, B., & Ball, V. (1998). Cardiovascular/Respiratory Physiotherapy. Mosby International Limited: Italy
- ↑ 3.0 3.1 Healthscout. (2009). Health Encyclopedia - Diseases and Conditions: Pneumonia. Retrieved April 8, 2009 from http://www.healthscout.com/ency/68/205/main.html
- ↑ Bartleby. The Lungs. Retrieved April 8, 2009 from http://education.yahoo.com/reference/gray/subjects/subject/240
- ↑ 5.0 5.1 5.2 5.3 Health-cares. (2005). What is pneumonia? Retrieved February 13, 2009 from http://respiratory-lung.health-cares.net/pneumonia.php
- ↑ Koenig, S., & Truwit, J. (2006). Ventilator-associated pneumonia: Diagnosis, treatment and prevention. Clin Microbiol Rev. 2006 October; 19(4): 637–657. Retrieved April 12, 2009 from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1592694
- ↑ Thorarinsdottir HR, Kander T, Holmberg A, Petronis S, Klarin B. Biofilm formation on three different endotracheal tubes: a prospective clinical trial.Available from:https://ccforum.biomedcentral.com/articles/10.1186/s13054-020-03092-1 (last accessed 30.6.2020)
- ↑ 8.0 8.1 Pahal P, Sharma S. Typical Bacterial Pneumonia.Available from:https://www.ncbi.nlm.nih.gov/books/NBK534295/ (last accessed 29.6.2020)
- ↑ Radiopedia Pneumonia Available from:https://radiopaedia.org/articles/pneumonia (last accessed 29.6.2020)
- ↑ Dadonaite B, Roser M. Pneumonia. Our World in Data; 2020 [updated Nov 2019; cited 11 May 2020].Available:https://ourworldindata.org/pneumonia (accessed 24.12.2022)
- ↑ World health organisation Pneumonia Available:https://www.who.int/health-topics/pneumonia/#tab=tab_1 (accessed 18.12.2022)
- ↑ news Medical Pneumonia Epidemiology Available:https://www.news-medical.net/health/Pneumonia-Epidemiology.aspx (accessed 24.12.2022)
- ↑ 13.0 13.1 13.2 13.3 Atkuri, L.V., & King, B.R. (2006). Pediatrics, Pneumonia. Retrieved April 10, 2009, from http://emedicine.medscape.com/article/803364-overview
- ↑ 14.0 14.1 14.2 14.3 Steyl, T. (2007). Applied Physiotherapy 403 notes: Intensive Care Notes. University of the Western Cape.
- ↑ Adderley N, Sharma S. Pleural Friction Rub. Accessed 16 March 2020
- ↑ Klein, J. (2008). Pneumonia. Retrieved February 13, 2009 from http://kidshealth.org/PageManager.jsp?dn=KidsHealth&lic=1&ps=107&cat_id=20043&article_set=23001
- ↑ Torpy, J. (2007). Ventilator associated pneumonia. Retrieved April 12, 2009 from http://jama.ama-assn.org/cgi/content/full/297/14/1616
- ↑ 18.0 18.1 World Health Organisation Pneumonia Available from:https://www.who.int/news-room/fact-sheets/detail/pneumonia (last accessed 30.6.2020)
- ↑ Respiratory Physiotherapy
- ↑ 20.0 20.1 Kids Health. (2009). Pneumonia. Retrieved April 11, 2009 from http://kidshealth.org/parent/infections/lung/pneumonia.html
- ↑ Drugs information online. (2009). Pneumonia in children care Guidelines information. Retrieved April 11, 2009 from http://www.drugs.com/cg/pneumonia-in-children.html