Hospital Acquired Pneumonia
Original Editors - Students from Glasgow Caledonian University's Cardiorespiratory Therapeutics Project.
Top Contributors - Bertie Elles, Lucinda hampton, Kim Jackson, Adam Vallely Farrell, 127.0.0.1, Admin, Michelle Lee, Karen Wilson and Lauren Lopez
Introduction[edit | edit source]
Hospital-acquired pneumonia (HAP) is defined as pneumonia that occurs 48 hours or more after hospital admission and is not incubating at hospital admission.
- Early-onset (occurring within 4 days of admission) HAP is usually caused by the same bacteria and viruses as community-acquired pneumonia and has a good prognosis.
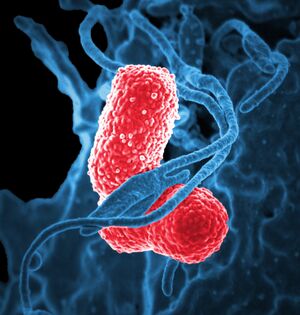
- Late-onset (starting 5 days or more after admission) HAP has a worse prognosis and is usually caused by micro-organisms that are acquired from the hospital environment. MRSA, Pseudomonas aeruginosa and other non-pseudomonal Gram-negative bacteria are the most common causes."[1]
HAP is the second most common hospital acquired infection (see Healthcare-Associated Infections), catheter-associated urinary tract infections being the most common.[2]
Epidemiology[edit | edit source]
- HAP is a common cause of pneumonia in those admitted to intensive care units (ICU) or on mechanical ventilation. 9/10 cases of HAP develope in ICUs occur in patients who are intubated and mechanically ventilated.
- The elderly are more are risk of developing HAP.[3]
Clinical Manifestations[edit | edit source]
- Symptoms of HAP: includes cough, expectoration, a rise in body temperature, chest pain or dyspnea.
- Signs include of HAP include: fever, tachypnea, consolidations or crackles.[4]
For more see Pneumonia
Physiotherapy and Other Management[edit | edit source]
Other health professionals will be treating your patient. What is their input? When addressing HAP, respiratory physiotherapy interventions should be individually tailored around the patient’s symptoms, observing aspects such as degree of pain, mobility capabilities and an array of complex factors[5].
Substantial evidence supports the role of physiotherapy in the respiratory managing HAP, demonstrating both short-term and longer term benefits[5].
Techniques may be found here Respiratory Physiotherapy and Respiratory Physiotherapy for ICU Patients Examples include:
- Manual hyperinflation
- Percussion, shaking, vibrations,
- Suctioning (if huffing or cough promoting techniques are proving ineffective in regards to sputum extraction),
- Breathing exercises
- Mobilization[5].
Prognosis[edit | edit source]
HAP is linked with increased death rates. The death rates associated with VAP ranges from 20% to 50% in different studies.[4]
Prevention[edit | edit source]
Several basic nursing interventions are associated with reducing HAP risk—
- Following infection prevention standards
- Elevating the head of the bed 30 to 45 degrees to prevent aspiration
- Seeing to good oral hygiene (cleaning teeth, gums, tongue, dentures)
- Increasing patient mobility with ambulation to eg three times a day (as appropriate)
- Educating patient re coughing and deep breathing, and use of incentive spirometry.[2]
For more see Infection Prevention and Control
References[edit | edit source]
- ↑ NICE Hospital-acquired pneumonia caused by methicillin-resistant Staphylococcus aureus: telavancin Available:http://www.nice.org.uk/advice/esnm44/chapter/full-evidence-summary (accessed 25.12.2022)
- ↑ 2.0 2.1 American Nurse Preventing hospital-acquired pneumoniaAvailable:https://www.myamericannurse.com/preventing-hospital-acquired-pneumonia/ (accessed 25.12.20220
- ↑ Radiopedia Hospital-acquired pneumonia Available:https://radiopaedia.org/articles/hospital-acquired-pneumonia-1?lang=us (accessed 24.12.2022)
- ↑ 4.0 4.1 Shebl E, Gulick PG. Nosocomial Pneumonia. InStatPearls [Internet] 2021 Jul 21. StatPearls Publishing.Available;https://www.ncbi.nlm.nih.gov/books/NBK535441/#!po=22.7273 (accessed 25.12.2022)
- ↑ 5.0 5.1 5.2 Denehy L, Berney S. Physiotherapy in the intensive care unit. Physical Therapy Reviews. 2006;11(1):49. Available: https://www.researchgate.net/publication/233585155_Denehy_L_Berney_S_Physiotherapy_in_the_intensive_care_unit_Phys_Ther_Rev_20061149-56 (accessed 25.12.2022)