Restrictive Lung Disease: Difference between revisions
No edit summary |
No edit summary |
||
| (8 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
| Line 9: | Line 6: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Restrictive lung diseases are a heterogeneous set of [[Respiratory Disorders|pulmonary disorders]] defined by restrictive patterns on [[spirometry]]. These disorders are characterized by a reduced distensibility of the [[Lung Anatomy|lung]]<nowiki/>s, [[Lung Compliance|compromising lung expansion]], and, in turn, reduced [[Lung Volumes|lung volumes]], particularly with reduced total lung capacity (TLC).<ref name=":0">Martinez-Pitre PJ, Sabbula BR, Cascella M. [https://www.ncbi.nlm.nih.gov/books/NBK560880/ Restrictive Lung Disease]. StatPearls [Internet]. 2020 Jul 15.Available from: https://www.ncbi.nlm.nih.gov/books/NBK560880/ (accessed 9.5.2021)</ref> | |||
Restrictive lung diseases are a heterogeneous set of pulmonary disorders defined by restrictive patterns on [[spirometry]]. These disorders are characterized by a reduced distensibility of the [[Lung Anatomy|lung]]<nowiki/>s, [[Lung Compliance|compromising lung expansion]], and, in turn, reduced [[Lung Volumes|lung volumes]], particularly with reduced total lung capacity (TLC).<ref name=":0">Martinez-Pitre PJ, Sabbula BR, Cascella M. [https://www.ncbi.nlm.nih.gov/books/NBK560880/ Restrictive Lung Disease]. StatPearls [Internet]. 2020 Jul 15.Available from: https://www.ncbi.nlm.nih.gov/books/NBK560880/ (accessed 9.5.2021)</ref> | |||
== Etiology == | == Etiology == | ||
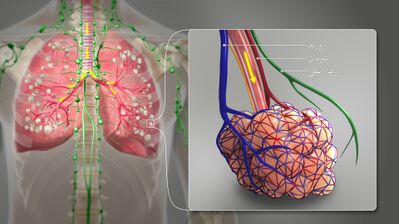
[[File: | [[File:3D Medical Animation Bronchial Airways terminating ends-ar.jpeg|right|frameless|399x399px]] | ||
Its aetiology can be highly variable ranging from | Its aetiology can be highly variable ranging from | ||
* Intrinsic - with lung parenchymal involvement ie Interstitial Lung Disease (ILD): an umbrella term that encompasses a large number of disorders that are characterised by diffuse cellular infiltrates in a periacinar location. The spectrum of conditions included is broad, ranging from occasional self-limited inflammatory processes to severe debilitating [[Pulmonary Fibrosis|pulmonary fibrosis]]<ref>Radiopedia [https://radiopaedia.org/articles/interstitial-lung-disease?lang=gb Interstitial Lung Disease] Available from:https://radiopaedia.org/articles/interstitial-lung-disease?lang=gb (accessed 9.5.2021)</ref>. | * Intrinsic - with lung parenchymal involvement ie Interstitial Lung Disease (ILD): an umbrella term that encompasses a large number of disorders that are characterised by diffuse cellular infiltrates in a periacinar location. The spectrum of conditions included is broad, ranging from occasional self-limited inflammatory processes to severe debilitating [[Pulmonary Fibrosis|pulmonary fibrosis]]<ref>Radiopedia [https://radiopaedia.org/articles/interstitial-lung-disease?lang=gb Interstitial Lung Disease] Available from:https://radiopaedia.org/articles/interstitial-lung-disease?lang=gb (accessed 9.5.2021)</ref>. | ||
'''Image 2''': A 3D Medical illustration showing different terminating ends of Bronchial airways connected to [[Alveoli|alveoili,]] lung parenchyma & [[Lymphatic System|lymphatic vessels]]. | |||
* Extrinsic to the lung - | * Extrinsic to the lung - | ||
** [[obesity]] | **[[obesity]] | ||
** [[Neuromuscular Disorders|neuromuscular disorders]] | **[[Neuromuscular Disorders|neuromuscular disorders]] | ||
** chest wall deformities | ** chest wall deformities | ||
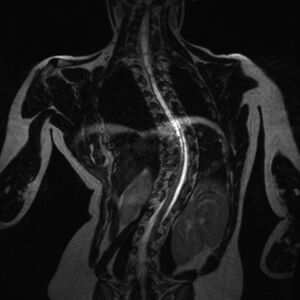
*** [[scoliosis]]: can lead to extrinsic restrictive lung disease from the diminution of lung volume under the convex rib hump and on the concave side, where the ribs impinge on the lung. | ***[[File:Excessive scoliosis.jpeg|right|frameless]][[scoliosis]]: can lead to extrinsic restrictive lung disease from the diminution of lung volume under the convex rib hump and on the concave side, where the ribs impinge on the lung. '''Image 3''': A pronounced C-shaped scoliosis is present, centred in the thoracic spine. | ||
*** excessive [[Thoracic Hyperkyphosis|kyphosis]] | *** excessive [[Thoracic Hyperkyphosis|kyphosis]] | ||
*** kyphoscoliosis | *** kyphoscoliosis | ||
Those with a restrictive lung disease pattern can often have decreased lung volumes, an increased work of breathing, and inadequate ventilation and/or oxygenation. [[Pulmonary Function Test|Pulmonary function tests]] often demonstrate a decrease in the forced vital capacity (FVC)<ref>Radiopedia [https://radiopaedia.org/articles/restrictive-lung-disease Restrictive Lung Disease] Available from:https://radiopaedia.org/articles/restrictive-lung-disease (accessed 9.5.2021)</ref>. | Those with a restrictive lung disease pattern can often have decreased lung volumes, an increased work of breathing, and inadequate ventilation and/or oxygenation. [[Pulmonary Function Test|Pulmonary function tests]] often demonstrate a decrease in the forced vital capacity (FVC)<ref>Radiopedia [https://radiopaedia.org/articles/restrictive-lung-disease Restrictive Lung Disease] Available from:https://radiopaedia.org/articles/restrictive-lung-disease (accessed 9.5.2021)</ref>. | ||
== Examples of ILD == | == Examples of ILD == | ||
[[File:Sarcoidosis-2.jpeg|right|frameless]] | |||
Intrinsic restriction can be caused by intrapulmonary restriction due to inflammatory processes within the lung tissue by diseases categorized under ILD | Intrinsic restriction can be caused by intrapulmonary restriction due to inflammatory processes within the lung tissue by diseases categorized under ILD | ||
*[[Sarcoidosis]]'''Image 4''': Chest x-ray demonstrates upper zone reticulonodular opacities with extensive mediastinal and hilar nodal enlargement. Stage II sarcoidosis with both nodal and parenchymal disease. | |||
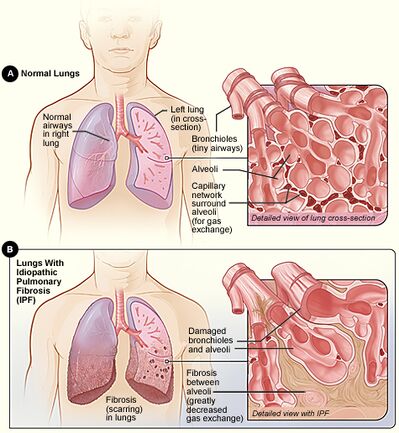
* [[Pulmonary Fibrosis|Idiopathic pulmonary fibrosis]] (IPF) | * [[Pulmonary Fibrosis|Idiopathic pulmonary fibrosis]] (IPF) | ||
* Inorganic dust exposure such as silicosis, asbestosis ([[ | * Inorganic dust exposure such as silicosis, asbestosis ([[Mesothelioma|Mesothelioma]]), talc, pneumoconiosis, berylliosis, hard metal fibrosis, coal worker's pneumoconiosis, chemical worker's lung | ||
* Organic dust exposure such as [[Aspergillosis]], bird fancier's lung, bagassosis, and [[Aspergillosis|mushroom worker's lung]], [[Neonatal Respiratory Distress Syndrome|neonatal respiratory distress syndrome]], hot tub pneumonitis | * Organic dust exposure such as [[Aspergillosis]], bird fancier's lung, bagassosis, and [[Aspergillosis|mushroom worker's lung]], [[Neonatal Respiratory Distress Syndrome|neonatal respiratory distress syndrome]], hot tub pneumonitis | ||
* Non-specific interstitial [[pneumonia]] (NSIP) | * Non-specific interstitial [[pneumonia]] (NSIP) | ||
* Medications such as nitrofurantoin, amiodarone, gold, phenytoin, thiazides, hydralazine, bleomycin, carmustine, cyclophosphamide, methotrexate | * Medications such as nitrofurantoin, amiodarone, gold, phenytoin, thiazides, hydralazine, bleomycin, carmustine, cyclophosphamide, methotrexate | ||
*[[Radiation Side Effects and Syndromes|Radiation Therapy]] | |||
* [[Radiation Side Effects and Syndromes|Radiation Therapy]] | |||
* Acute interstitial pneumonia (AIP)<ref name=":0" /> | * Acute interstitial pneumonia (AIP)<ref name=":0" /> | ||
== Epidemiology == | == Epidemiology == | ||
The overall prevalence of restrictive diseases is difficult to estimate precisely because the groups involve multiple pathological conditions, each of which can occur in numerous clinical stages. | The overall prevalence of restrictive diseases is difficult to estimate precisely because the groups involve multiple pathological conditions, each of which can occur in numerous clinical stages. | ||
[[File:Normal-chest-radiograph-obese-patient.jpeg|right|frameless]] | |||
The populations with higher associations to restrictive lung patterns include: | The populations with higher associations to restrictive lung patterns include: | ||
* [[Older People - Patterns of Illness, Physiological Changes and Multiple Pathology|Older Persons]]- The prevalence of restrictive conditions increases from 2.7 cases per 100,000 persons in individuals aged 35-44 years to over 175 cases per 100,000 in those older than 75 years. | *[[Older People - Patterns of Illness, Physiological Changes and Multiple Pathology|Older Persons]]- The prevalence of restrictive conditions increases from 2.7 cases per 100,000 persons in individuals aged 35-44 years to over 175 cases per 100,000 in those older than 75 years. | ||
* African Americans- Compared to Whites (10.9 cases per 100,000), the prevalence in this group is 35.5 cases per 100,000 persons. | * African Americans- Compared to Whites (10.9 cases per 100,000), the prevalence in this group is 35.5 cases per 100,000 persons. | ||
* Obese individuals- Restrictive patterns are related to an elevated body mass index (BMI) with a decrease in lung volumes attributed to an increased amount of central obesity. | * Obese individuals- Restrictive patterns are related to an elevated body mass index (BMI) with a decrease in lung volumes attributed to an increased amount of central obesity. '''Image 5:''' restrictive lung volumes in an obese individual, Large amount of adipose tissue as demonstrates by the excessive facial/neck fat, pericardial fat and general soft tissue. | ||
* [[Smoking Cessation and Brief Intervention|Smokers.]]<ref name=":0" /> | *[[Smoking Cessation and Brief Intervention|Smokers.]]<ref name=":0" /> | ||
== Diagnosis == | == Diagnosis == | ||
Diagnostic testing for lung disease may include any of the following: | Diagnostic testing for lung disease may include any of the following: | ||
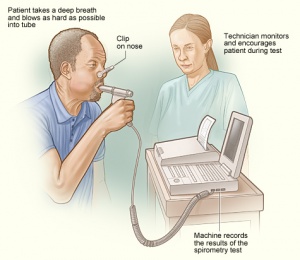
* [[Pulmonary Function Test|Pulmonary function tests]] | *[[File:Spirometry1.jpg|right|frameless]][[Pulmonary Function Test|Pulmonary function tests]](Image 6: [[Spirometry]] is one of the Pulmonary function tests) | ||
* Chest [[X-Rays|X-ray]] | * Chest [[X-Rays|X-ray]] | ||
* [[CT Scans|CT scans]] | *[[CT Scans|CT scans]] | ||
* Bronchoscopy | * Bronchoscopy | ||
* Pulse oximetry<ref name=":1" /> | * Pulse oximetry<ref name=":1" /> | ||
== Treatment == | == Treatment == | ||
[[File:Normal lungs.jpg|right|frameless|433x433px]] | |||
Treatment of lung disease depends on many factors, such as the type and stage of disease, family history, patient’s medical history and the health and age of the patient. Any of the following may be used for treating lung disease: | Treatment of lung disease depends on many factors, such as the type and stage of disease, family history, patient’s medical history and the health and age of the patient. Any of the following may be used for treating lung disease: | ||
| Line 66: | Line 65: | ||
* Expectorants | * Expectorants | ||
* [[Antibiotics]] | * [[Antibiotics]] | ||
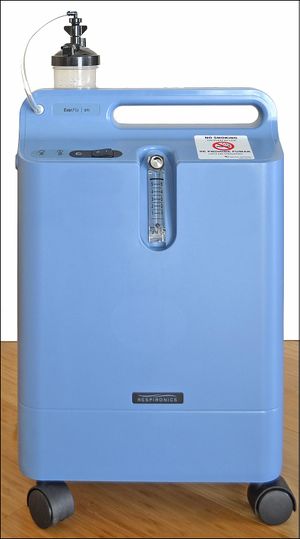
* [[Oxygen Therapy|Oxygen therapy]] | * [[Oxygen Therapy|Oxygen therapy]] : The main treatment for restrictive lung disease is supportive [[Oxygen Therapy|oxygen therapy]]. Oxygen therapy helps people with lung diseases get enough oxygen, even when their lungs cannot fully expand. Some people may need oxygen only at night or after exerting themselves. Others need oxygen all or most of the time. | ||
* [[Chemotherapy Side Effects and Syndromes|Chemotherapy]] | * [[Chemotherapy Side Effects and Syndromes|Chemotherapy]] : may help reduce inflammation caused by a restrictive lung disease. However, chemotherapy also kills healthy cells and can prompt a range of side effects, such as nausea, hair loss, and a weakened immune system. Some studiesTrusted Source have also found a link between chemotherapy and lung damage. As such, it is important to weigh the potential benefits of chemotherapy against its risks. | ||
* [[Heart Lung Transplant|Lung transplantation]]<ref name=":1">John Hopkins [https://www.hopkinsmedicine.org/health/conditions-and-diseases/restrictive-lung-disease Restrictive Lung Disease] Available from:https://www.hopkinsmedicine.org/health/conditions-and-diseases/restrictive-lung-disease (accessed 9.5.2021)</ref> | * [[Heart Lung Transplant|Lung transplantation]]<ref name=":1">John Hopkins [https://www.hopkinsmedicine.org/health/conditions-and-diseases/restrictive-lung-disease Restrictive Lung Disease] Available from:https://www.hopkinsmedicine.org/health/conditions-and-diseases/restrictive-lung-disease (accessed 9.5.2021)</ref>Lung transplants offer a chance of a healthier, longer life, but they are also highly risky. After a lung transplant, a person can develop life-threatening complications, such as organ rejection. After a lung transplant, a recipient must take drugs that suppress the immune system. However, these drugs make transplant recipients more vulnerable to many infections. As a result, most transplant recipients must be closely monitored in hospital for several weeks. | ||
* Stem cell therapy is still an experimental treatment, but for some people with restrictive lung disease, it may offer the chance of a longer life. | |||
* Clinical trials: Treatment for restrictive lung disease is continually evolving. Some people with symptoms of the disease may be eligible for a clinical trial. There is no guarantee that new drugs will work, but many clinical trials have helped people get better<ref name=":2">Medical news today [https://www.medicalnewstoday.com/articles/319012 How to recognize and treat restrictive lung disease] Available from: https://www.medicalnewstoday.com/articles/319012 ( accessed 10.5.2021)</ref>. | |||
* Impairment in pulmonary function in patients with severe scoliosis may be controlled with surgical correction. | * Impairment in pulmonary function in patients with severe scoliosis may be controlled with surgical correction. | ||
* For obese patients, management involves losing weight by a combination of diet and physical exercise. Morbidly obese patients who fail to lose weight by traditional methods should be referred for gastric bypass surgery evaluation.<ref name=":0" /> | * For obese patients, management involves losing weight by a combination of diet and physical exercise. Morbidly obese patients who fail to lose weight by traditional methods should be referred for gastric bypass surgery evaluation.<ref name=":0" /> | ||
[[Ventilation and Weaning|Ventilator therapy]]: A ventilator is a device that helps the lungs take in oxygen. Unlike oxygen therapy that is given through the nose, a ventilator uses a tube in the throat or a high-pressure mask to support breathing. People who have an advanced restrictive lung disease may need a ventilator to be able to breathe.<ref name=":2" /> | |||
For some people, ventilator therapy is unsafe or cannot be used. Hence, in extreme cases, an alternative called extracorporeal membrane oxygenation (ECMO) delivers oxygen directly to the blood. <ref name=":2" />For ECMO, a doctor removes blood through a large vein. The blood is pumped through a membrane that provides it with oxygen, and it is then put back in the body. | |||
== Physiotherapy == | == Physiotherapy == | ||
See[[Pulmonary Rehabilitation]]<nowiki/>and [[ | [[File:Treadmill walk.jpg|right|frameless]] | ||
Pulmonary rehabilitation programs help people better understand their oxygen needs and breathe more efficiently. This input can enable them to cope better with their disease. See[[Pulmonary Rehabilitation]]<nowiki/>and [[Silicosis]] | |||
Diet Education: Some people find that dietary changes, such as eating smaller meals, help with some restrictive lung diseases, including pulmonary fibrosis.<ref name=":2" /> | |||
Also Individual Links above | Also Individual Links above | ||
Clients may need [[Oxygen Therapy]] and[[Oxygen Therapy at Home]] | |||
== End of Life Care == | == End of Life Care == | ||
[[File:Oxygen Concentrator.jpg|right|frameless]] | |||
Many forms of restrictive lung disease are progressive, getting worse over time. As the end of life approaches, there may be changes that happen over days...or weeks. Each person's experience is unique. People with end-stage lung disease often have significant airflow limitations. Even simple tasks like taking a shower, making the bed and cooking a meal become nearly impossible to do. In addition, people with end-stage lung disease often feel exhausted<ref>Lung institute End stage lung disease Available from: https://lunginstitute.com/blog/mean-end-stage-lung-disease/ (accessed 10.5.2021)</ref>. Typically, lung function drops to 30 percent or less during end-stage lung disease. Also, many people have low blood oxygen levels. | |||
Despite increasing mortality due to interstitial lung disease (ILD) the provision of end-of-life care for these conditions is limited. Improving quality of care for patients with advanced ILD or any other progressive respiratory disease requires a paradigm shift. Best supportive care as it is currently experienced is far from best. [[Physiotherapy in Palliative Care|Palliative]] care needs to sit alongside curative intent as an equally legitimate professional goal.<ref>Taylor DR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5709798/ Progressive respiratory disease: the importance of prognostic conversations and advance care planning]. Breathe. 2017 Dec 1;13(4):269-73.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5709798/ (accessed 9.5.2021)</ref> | Despite increasing mortality due to interstitial lung disease (ILD) the provision of end-of-life care for these conditions is limited. Improving quality of care for patients with advanced ILD or any other progressive respiratory disease requires a paradigm shift. Best supportive care as it is currently experienced is far from best. [[Physiotherapy in Palliative Care|Palliative]] care needs to sit alongside curative intent as an equally legitimate professional goal.<ref>Taylor DR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5709798/ Progressive respiratory disease: the importance of prognostic conversations and advance care planning]. Breathe. 2017 Dec 1;13(4):269-73.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5709798/ (accessed 9.5.2021)</ref> | ||
== References == | == References == | ||
Latest revision as of 14:24, 27 October 2022
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Kim Jackson and Vidya Acharya
Introduction[edit | edit source]
Restrictive lung diseases are a heterogeneous set of pulmonary disorders defined by restrictive patterns on spirometry. These disorders are characterized by a reduced distensibility of the lungs, compromising lung expansion, and, in turn, reduced lung volumes, particularly with reduced total lung capacity (TLC).[1]
Etiology[edit | edit source]
Its aetiology can be highly variable ranging from
- Intrinsic - with lung parenchymal involvement ie Interstitial Lung Disease (ILD): an umbrella term that encompasses a large number of disorders that are characterised by diffuse cellular infiltrates in a periacinar location. The spectrum of conditions included is broad, ranging from occasional self-limited inflammatory processes to severe debilitating pulmonary fibrosis[2].
Image 2: A 3D Medical illustration showing different terminating ends of Bronchial airways connected to alveoili, lung parenchyma & lymphatic vessels.
- Extrinsic to the lung -
- obesity
- neuromuscular disorders
- chest wall deformities
Those with a restrictive lung disease pattern can often have decreased lung volumes, an increased work of breathing, and inadequate ventilation and/or oxygenation. Pulmonary function tests often demonstrate a decrease in the forced vital capacity (FVC)[3].
Examples of ILD[edit | edit source]
Intrinsic restriction can be caused by intrapulmonary restriction due to inflammatory processes within the lung tissue by diseases categorized under ILD
- SarcoidosisImage 4: Chest x-ray demonstrates upper zone reticulonodular opacities with extensive mediastinal and hilar nodal enlargement. Stage II sarcoidosis with both nodal and parenchymal disease.
- Idiopathic pulmonary fibrosis (IPF)
- Inorganic dust exposure such as silicosis, asbestosis (Mesothelioma), talc, pneumoconiosis, berylliosis, hard metal fibrosis, coal worker's pneumoconiosis, chemical worker's lung
- Organic dust exposure such as Aspergillosis, bird fancier's lung, bagassosis, and mushroom worker's lung, neonatal respiratory distress syndrome, hot tub pneumonitis
- Non-specific interstitial pneumonia (NSIP)
- Medications such as nitrofurantoin, amiodarone, gold, phenytoin, thiazides, hydralazine, bleomycin, carmustine, cyclophosphamide, methotrexate
- Radiation Therapy
- Acute interstitial pneumonia (AIP)[1]
Epidemiology[edit | edit source]
The overall prevalence of restrictive diseases is difficult to estimate precisely because the groups involve multiple pathological conditions, each of which can occur in numerous clinical stages.
The populations with higher associations to restrictive lung patterns include:
- Older Persons- The prevalence of restrictive conditions increases from 2.7 cases per 100,000 persons in individuals aged 35-44 years to over 175 cases per 100,000 in those older than 75 years.
- African Americans- Compared to Whites (10.9 cases per 100,000), the prevalence in this group is 35.5 cases per 100,000 persons.
- Obese individuals- Restrictive patterns are related to an elevated body mass index (BMI) with a decrease in lung volumes attributed to an increased amount of central obesity. Image 5: restrictive lung volumes in an obese individual, Large amount of adipose tissue as demonstrates by the excessive facial/neck fat, pericardial fat and general soft tissue.
- Smokers.[1]
Diagnosis[edit | edit source]
Diagnostic testing for lung disease may include any of the following:
- Pulmonary function tests(Image 6: Spirometry is one of the Pulmonary function tests)
- Chest X-ray
- CT scans
- Bronchoscopy
- Pulse oximetry[4]
Treatment[edit | edit source]
Treatment of lung disease depends on many factors, such as the type and stage of disease, family history, patient’s medical history and the health and age of the patient. Any of the following may be used for treating lung disease:
- Inhalers
- Expectorants
- Antibiotics
- Oxygen therapy : The main treatment for restrictive lung disease is supportive oxygen therapy. Oxygen therapy helps people with lung diseases get enough oxygen, even when their lungs cannot fully expand. Some people may need oxygen only at night or after exerting themselves. Others need oxygen all or most of the time.
- Chemotherapy : may help reduce inflammation caused by a restrictive lung disease. However, chemotherapy also kills healthy cells and can prompt a range of side effects, such as nausea, hair loss, and a weakened immune system. Some studiesTrusted Source have also found a link between chemotherapy and lung damage. As such, it is important to weigh the potential benefits of chemotherapy against its risks.
- Lung transplantation[4]Lung transplants offer a chance of a healthier, longer life, but they are also highly risky. After a lung transplant, a person can develop life-threatening complications, such as organ rejection. After a lung transplant, a recipient must take drugs that suppress the immune system. However, these drugs make transplant recipients more vulnerable to many infections. As a result, most transplant recipients must be closely monitored in hospital for several weeks.
- Stem cell therapy is still an experimental treatment, but for some people with restrictive lung disease, it may offer the chance of a longer life.
- Clinical trials: Treatment for restrictive lung disease is continually evolving. Some people with symptoms of the disease may be eligible for a clinical trial. There is no guarantee that new drugs will work, but many clinical trials have helped people get better[5].
- Impairment in pulmonary function in patients with severe scoliosis may be controlled with surgical correction.
- For obese patients, management involves losing weight by a combination of diet and physical exercise. Morbidly obese patients who fail to lose weight by traditional methods should be referred for gastric bypass surgery evaluation.[1]
Ventilator therapy: A ventilator is a device that helps the lungs take in oxygen. Unlike oxygen therapy that is given through the nose, a ventilator uses a tube in the throat or a high-pressure mask to support breathing. People who have an advanced restrictive lung disease may need a ventilator to be able to breathe.[5]
For some people, ventilator therapy is unsafe or cannot be used. Hence, in extreme cases, an alternative called extracorporeal membrane oxygenation (ECMO) delivers oxygen directly to the blood. [5]For ECMO, a doctor removes blood through a large vein. The blood is pumped through a membrane that provides it with oxygen, and it is then put back in the body.
Physiotherapy[edit | edit source]
Pulmonary rehabilitation programs help people better understand their oxygen needs and breathe more efficiently. This input can enable them to cope better with their disease. SeePulmonary Rehabilitationand Silicosis
Diet Education: Some people find that dietary changes, such as eating smaller meals, help with some restrictive lung diseases, including pulmonary fibrosis.[5]
Also Individual Links above
Clients may need Oxygen Therapy andOxygen Therapy at Home
End of Life Care[edit | edit source]
Many forms of restrictive lung disease are progressive, getting worse over time. As the end of life approaches, there may be changes that happen over days...or weeks. Each person's experience is unique. People with end-stage lung disease often have significant airflow limitations. Even simple tasks like taking a shower, making the bed and cooking a meal become nearly impossible to do. In addition, people with end-stage lung disease often feel exhausted[6]. Typically, lung function drops to 30 percent or less during end-stage lung disease. Also, many people have low blood oxygen levels.
Despite increasing mortality due to interstitial lung disease (ILD) the provision of end-of-life care for these conditions is limited. Improving quality of care for patients with advanced ILD or any other progressive respiratory disease requires a paradigm shift. Best supportive care as it is currently experienced is far from best. Palliative care needs to sit alongside curative intent as an equally legitimate professional goal.[7]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Martinez-Pitre PJ, Sabbula BR, Cascella M. Restrictive Lung Disease. StatPearls [Internet]. 2020 Jul 15.Available from: https://www.ncbi.nlm.nih.gov/books/NBK560880/ (accessed 9.5.2021)
- ↑ Radiopedia Interstitial Lung Disease Available from:https://radiopaedia.org/articles/interstitial-lung-disease?lang=gb (accessed 9.5.2021)
- ↑ Radiopedia Restrictive Lung Disease Available from:https://radiopaedia.org/articles/restrictive-lung-disease (accessed 9.5.2021)
- ↑ 4.0 4.1 John Hopkins Restrictive Lung Disease Available from:https://www.hopkinsmedicine.org/health/conditions-and-diseases/restrictive-lung-disease (accessed 9.5.2021)
- ↑ 5.0 5.1 5.2 5.3 Medical news today How to recognize and treat restrictive lung disease Available from: https://www.medicalnewstoday.com/articles/319012 ( accessed 10.5.2021)
- ↑ Lung institute End stage lung disease Available from: https://lunginstitute.com/blog/mean-end-stage-lung-disease/ (accessed 10.5.2021)
- ↑ Taylor DR. Progressive respiratory disease: the importance of prognostic conversations and advance care planning. Breathe. 2017 Dec 1;13(4):269-73.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5709798/ (accessed 9.5.2021)