Pulmonary Function Test
Original Editor - Uchechukwu Chukwuemeka
Top Contributors - Lucinda hampton, Kim Jackson and Admin
Description[edit | edit source]
Pulmonary function tests, or PFTs, measure how well the lungs work. For some of the test measurements, the client can breathe normally and quietly. Other tests require forced inhalation or exhalation after a deep breath. Sometimes, they will be asked to inhale a different gas or a medicine to see how it changes test results.
PFTs can be used in a variety of settings, and they are generally ordered to:
- Look for evidence of respiratory disease when patients present with respiratory symptoms (e.g. dyspnea, cough, cyanosis, wheezing, etc.)
- Assess for any progression of lung disease
- Monitor the efficacy of a given treatment
- Evaluate patients pre-operatively
- Monitor for potentially toxic side effects of certain drugs (e.g. amiodarone, an antiarrhythmic drug)[1]
Different Pulmonary Function Tests[edit | edit source]
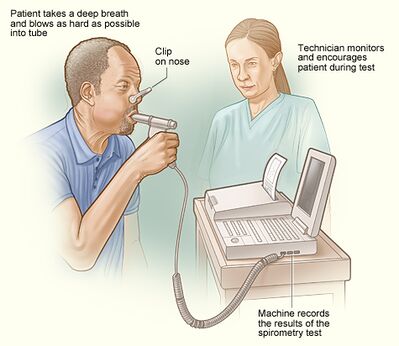
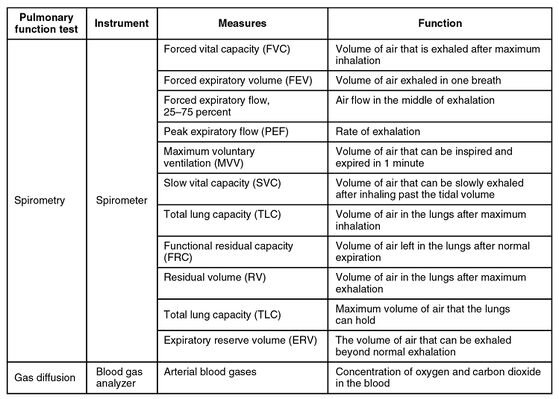
1.Spirometry Measures the rate of air flow and estimates lung size. For this test, client will breathe multiple times, with regular and maximal effort, through a tube that is connected to a computer. Some people feel lightheaded or tired from the required breathing effort.
- Data obtained from spirometry
- The most commonly used measures include the forced vital capacity (FVC), the forced expiratory volume in one second (FEV1), and the ratio of the two (FEV1/FVC), which should be about 80% in normal patients
- An FEV1/FVC <80% suggests obstructive lung disease, while restrictive lung disease typically has normal or increased FEV1/FVC
- Other useful data from spirometry include measures of flow, eg peak inspiratory flow (PIF) and peak expiratory flow (PEF)
Lung volume tests are the most accurate way to measure how much air the lungs can hold. Lung volume measurement can be done in two ways: 1.The most accurate way is called body plethysmography. You sit in a clear airtight box that looks like a phone booth. The technologist asks you to breathe in and out of a mouthpiece. Changes in pressure inside the box help determine the lung volume. 2.Lung volume can also be measured when you breathe nitrogen or helium gas through a tube for a certain period of time. The concentration of the gas in a chamber attached to the tube is measured to estimate the lung volume.[2]
Image 3: Flow Volume Curve during a spirometry test from a normal subject
Lung diffusion capacity assesses how well oxygen gets into the blood from the air you breathe. Client breathes a harmless gas, called a tracer gas, for a very short time, often for only one breath. The concentration of the gas in the air you breathe out is measured. The difference in the amount of gas inhaled and exhaled measures how effectively gas travels from the lungs into the blood. This test provides an estimate how well the lungs move oxygen from the air into the bloodstream.
Oximetry: the measuring of the percentage of oxygen-saturated hemoglobin in the blood by means of an oximeter. Readings below 90 percent may be indicative of impaired lung function or infection. In noninvasive pulse oximetry , a small device placed on a fingertip or earlobe uses light waves to measure the oxygen saturation in arterial blood.[3] For this test, a probe will be placed on the finger or another skin surface such as the ear. It causes no pain and has few or no risks.
Arterial blood gas tests directly measure the levels of gases, such as oxygen and carbon dioxide, in your blood. Arterial blood gas tests are usually performed in a hospital, but may be done in a doctor’s office. For this test, blood will be taken from an artery, usually in the wrist.
Fractional exhaled nitric oxide tests measure how much nitric oxide is in the air that you exhale. For this test, client will breathe out into a tube that is connected to the portable device. It requires steady but not intense breathing. It has few or no risks.
Other tests may be needed to assess lung function including:
Diffusing Capacity of Carbon monoxide (DLCo) Oxygen. Diffusing capacity is a measure of the ability of the lungs to transfer gas into the blood. Diffusion of gas to blood in the lungs is the most efficient when there is a high surface area for transfer, and when the blood is able to accept the gas being transferred. The diffusing capacity is helpful primarily in distinguishing between types of obstructive lung disease. For example, the diffusing capacity will generally be normal or increased in asthma, while it will be decreased in emphysema[1].
Bronchodilator Test. A bronchial challenge test measures how sensitive the airways in your lungs are. It’s used to help make a diagnosis in people who may have asthma. The bronchial challenge test is sometimes called an airway provocation test. It involves breathing in gradually increasing doses of a medication that can irritates the airways and cause them to get narrower. People with sensitive lungs will be affected by a much lower dose of this medication than people with healthy lungs. The test is done carefully to make sure it is safe. One of the defining characteristics of asthma is an increase in the responsiveness of the airways to a number of stimuli. If lung function is normal but the patient experiences intermittent episodes of cough, dyspnea, or wheezing, the demonstration of bronchial hyper-responsiveness may be useful in establishing a diagnosis of asthma, exercise-induced[4] asthma or eucapnic voluntary hyperpnea[5].
Cardiorespiratory Exercise Test [6] Lung problems can make it harder to do day-to-day activities. Exercise capacity tests can be used to measure what people are able to do. If someone’s exercise capacity is reduced, the tests may help to explain why. Exercise capacity tests are also sometimes used to tell anaesthetic teams how fit a person is (important when assessing people for major surgery). Walking tests can measure how effective pulmonary rehabilitation has been and whether client needs oxygen when you are walking (called an ambulatory oxygen assessment).
Respiratory Muscle Function Test. Respiratory muscle tests measure how much pressure the breathing muscles can generate when client breathes in or out. Maximal inspiratory and expiratory pressures (MIP/MEPs) are measured by having the patient perform maximal inspiratory and expiratory efforts against a closed valve and measuring the static pressures that are generated. The lung specialist may also ask client to do a spirometry test lying down, to see if this makes lung capacity fall by more than 30% when moving from an upright position to lying down. This is a sign of muscle weakness.[1][5].
Calculation of body mass index (BMI). Being overweight or underweight can affect your breathing, lung function and general health. Being overweight can cause breathlessness[5].
Patterns of Respiratory Diseases[edit | edit source]
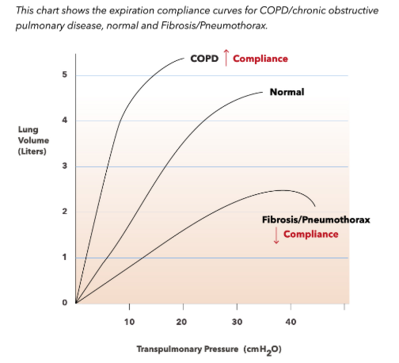
Obstructive pattern
- Decreased FEV1, normal or decreased FVC, and decreased FEV1/FVC
- Classically, these are the patients with asthma, chronic bronchitis, or emphysema
- PFTs can help further distinguish between the above three:
- Bronchodilator responsiveness - an increase in the FEV1 by 12% following bronchodilator use suggests asthma
- Bronchial provocation - inducing asthmatic obstruction of reactive lower airways by administering methacholine, histamine, or adenosine monophosphate
- DLCO will be decreased in patients with emphysema, and can be normal or increased in patients with asthma
- PFTs can help further distinguish between the above three:
- Lower airway obstruction vs. upper airway obstruction
- Lower airway obstruction typically displays impaired expiratory capacity (see image below), while upper airway obstruction has impaired inspiratory capacity, which can be evident on the flow volume loop (seen as flattening of the inspiratory arm)
- Restrictive pattern
- Decreased TLC, FEV1, and FVC with a normal FEV1/FVC, and a low DLCO
- Typically these are patients with interstitial lung disease, severe skeletal abnormalities, or diaphragmatic paralysis
- The flow volume loop is generally normal in appearance, but has low lung volumes
Radiology[edit | edit source]
Pulmonary function tests (PFTs) provide important quantitative information about lung function and can be used to elucidate pathologic conditions responsible for respiratory symptoms, assess the severity and course of disease, and evaluate the patient for suitability and timing for lung transplantation. They are typically used in tandem with chest imaging, along with other ancillary data, to arrive at a specific diagnosis. PFTs may provide the radiologist with clues to the diagnosis and grading of a wide variety of pulmonary diseases[7].
Indication[edit | edit source]
- Investigation of a patient with sign/symptoms that shows respiratory problems. e.g. wheezing, coughing, crackles and abnormal chest xray e.t.c.
- Monitoring of patients with respiratory condition for disease progression and response to treatment.
- Evaluation of degree of cardio-respiratory disability
- Preoperative evaluation for patient that will undergo thoracic and abdominal surgery
- Montoring of patients at risk of pulmonary complications
- Routine assessment for individual with high exposure to pulmonary toxic agent e.g abestos, dust and fumes
Contraindication[edit | edit source]
- Myocardial Infarction in the last month
- Unstable Angina
- Recent thoracic and abdominal surgeries
- Recent Opthalmic surgery
- Abdominal, thoracic and cerebral Aureysms
- Active Hemoptysis
- Pneumothorax
The Future for PFTs[edit | edit source]
Pulmonary function testing is an important diagnostic specialty, particularly with regard to diseases such as COPD, asthma, and interstitial lung disease. As new and better therapies for a wide array of pulmonary disorders become available, pulmonary function testing should play an increasing role in identifying and quantifying the physiologic changes attributable not just to the disease, but to the treatment as well. This will require attention to the details of laboratory quality assurance, highly motivated and well-trained physicians and technologists, and a willingness to explore new and better ways of improving patient outcomes.[8]
Interpretation[edit | edit source]
Step 1: FEV1/FVC ratio
- FEV1/FVC <70% (or less than the Lower limit of normal) : Obstructive Pattern (COPD, Asthma)
- ≥70%: Normal or Restrictive disease
Step 2: Severity of obstruction (GOLD Criteria for COPD)
- FEV1 80-100% predicted: Mild (Stage 1)
- FEV1 50- 80% predicted: Moderate (Stage 2)
- FEV1 30- <50% predicted: Severe (Stage 3)
- FEV1 <30% predicted: Very severe (Stage 4)
- FEV1 <50% with right side heart failure: Very severe (Stage 4)
Severity of obstruction (ATS General Criteria)
- FEV1 over 70% predicted: MILD
- FEV1 60-70%predicted: MODERATE
- FEV1 50-60% predicted: MODERATELY SEVERE
- FEV1 35-50% predicted: SEVERE
- FEV1 <35% predicted: VERY SEVERE
Step 3
- ≥12% increase AND an absolute improvement of at least 200ml after inhaling a beta agonist.
- FEV1, OR FVC is considered a significant response.
Step 4: Total Lung Capacity (TLC) (Normal range: 80-120% of predicted)
- TLC >120 = Hyperinflation
- TLC <80% = Restrictive disease (ATS criteria for severity)
- 70-80% predicted: MILD
- 60-70% predicted: MODERATE
- 50-60% predicted: MODERATELY SEVERE
- <50% predicted: SEVERE
Step 5: RV/TLC ratio (Normal range: <35% or < predicted)
- RV/TLC >35% or > predicted indicates Air trapping
Step 6: DLCO (Normal range: 80-120% of predicted)
- In obstructive disease:
- Decreased in Emphysema
- Normal in chronic bronchitis
- Normal or increased in Asthma
- In restrictive disease:
- Decreased in parenchymal disease
- Normal in non-parenchymal (e.g. chest wall) restriction[9]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 University of Iowa Head and neck protocols Available from: https://medicine.uiowa.edu/iowaprotocols/pulmonary-function-testing-pft-made-simple (accessed 15.5.21)
- ↑ medlineplus PFT Available from:https://medlineplus.gov/ency/article/003853.htm (accessed 15.5.2021)
- ↑ Dictionary.com Oximetry Available from: https://www.dictionary.com/browse/oximetry (accessed 15.5.21)
- ↑ Pulmonary Advisor PFT Available from: https://www.pulmonologyadvisor.com/home/decision-support-in-medicine/pulmonary-medicine/pulmonary-function-testing/ (accessed 15.5.21)
- ↑ 5.0 5.1 5.2 British lung foundation Lung function tests Available from: https://www.blf.org.uk/support-for-you/breathing-tests/tests-to-measure-breathing (accessed 15.5.2021)
- ↑ Guazzi M, Bandera F, Ozemek C, Systrom D, Arena R.Cardiopulmonary Exercise Testing; What Is its Value?Journal of the American College of Cardiology. 2017;70(13) DOI: 10.1016/j.jacc.2017.08.012
- ↑ Tseng HJ, Henry TS, Veeraraghavan S, Mittal PK, Little BP. Pulmonary function tests for the radiologist. Radiographics. 2017 Jul;37(4):1037-58.Available from:https://pubmed.ncbi.nlm.nih.gov/28598732/ (accessed 15.5.2021)
- ↑ Ruppel GL, Enright PL. Pulmonary function testing. Respiratory care. 2012 Jan 1;57(1):165-75.Available from:http://rc.rcjournal.com/content/57/1/165.short#sec-1 (accessed 15.5.2021)
- ↑ Dweik AR. Interpretation of Common Lung Function Tests.Cleveland Clinic. 2011.https://www.clevelandclinicmeded.com/live/owork/us-state/MDpres2/16.0830.Dweik.Pulm.A.PFTs.CME.v2.pdf