Diaphragmatic Breathing Exercises
Introduction[edit | edit source]
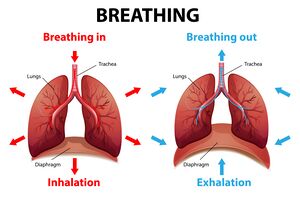
Diaphragmatic breathing is a type of breathing exercise that helps strengthen your diaphragm, an important muscle that helps you breathe as it represents 80% of breathing. This breathing exercise is also sometimes called belly breathing or abdominal breathing.
When the diaphragm is functioning effectively in its role as the primary muscle of inspiration, ventilation is efficient and the oxygen consumption of the muscles of ventilation is low during relaxed (tidal) breathing. When a patient relies substantially on the accessory muscles of inspiration, the mechanical work of breathing (oxygen consumption ) increases and the efficiency of ventilation decreases.[1]
Controlled breathing techniques, which emphasise diaphragmatic breathing are designed to improve the efficiency of ventilation, decrease the work of breathing, increase the excursion of the diaphragm, and improve gas exchange and oxygenation. Also breathing from the diaphragm generate intra-abdominal pressure for control of posture and you can accomplish slow respiration.[2]
Aims[edit | edit source]
- To mobilize secretions and teach breathing control.[3]
- To teach effective coughing and remove secretions.[3]
- To teach relaxation.[4]
- To teach postural awareness.[2]
- To mobilize thorax and shoulder girdle.[2]
Physiological Effect[edit | edit source]
Diaphramatic breathing have many physiological effects.
Its effect on the respiratory system is:
- Using the diaphragm consciously during respiration increases the lung capacity
- Improve the efficacy of oxygen ventilation through decreasing the respiratory rate and increasing the tidal volume
- Improving alveolar ventilation by reducing alveolar dead space and increasing the arterial oxygen saturation
- Improving blood oxygen levels[5]
Other physiological effects include:
- Activating the parasympathetic nervous activity while suppressing the sympathetic nervous activity [5]
- Improving core muscle stability.[6]
- Helps with relaxation, lowering the harmful effects of the stress hormone cortisol on your body.[4]
- Increased efficiency of venous return[1]
- Lower your blood pressure[1]
- Coping with the symptoms of post-traumatic stress disorder (PTSD)[7].
Positioning[edit | edit source]
Supine position[edit | edit source]
- Lie on your back on a flat surface (or in bed) with your knees bent. You can use a pillow under your head and your knees for support if that's more comfortable.
- Place one hand on your upper chest and the other on your belly, just below your rib cage.
- Breathe in slowly through your nose, letting the air in deeply, towards your lower belly. The hand on your chest should remain still, while the one on your belly should rise.
- Tighten your abdominal muscles and let them fall inward as you exhale through pursed lips. The hand on your belly should move down to its original position.[8]
You can also practice this sitting in a chair, with your knees bent and your shoulders, head, and neck relaxed. Practice for five to 10 minutes, several times a day if possible.
Sitting position[edit | edit source]
- Sit up straight in a chair lengthen the distance between your navel and sternum.
- Keep your shoulders relax.
- Keep the pelvis in neutral position (Sit on your sitting bones).
- Place your hands at either side of your lower ribs.
Breath in slowly through your nose. As you inhale feel your ribs expanding outwards and upwards. During inhalation is generated expansion of the trunk in three directions front , sides and back.
Breath out from your nose. As you exhale feel your lower ribs moving inwards.[2]
Precautions[edit | edit source]
- Never allow a patient to force expiration. Expiration should be relaxed or lightly controlled. Forced expiration only increases turbulence in the airways, leading to bronchospasm and increased airway restriction.
- Do not allow a patient to take a highly prolonged expiration. This causes the patient to gasp with the next inspiration. The patient's breathing pattern then becomes irregular and insufficient.
- Do not allow the patient to initiate inspiration with accessory muscles and upper chest.
- Allow the patient to perform deep breathing for only three or four inspirations and expirations at a time to avoid hyperventilation.
Indication[edit | edit source]
- Post -operative pain
- Airway obstruction (COPD, asthma)[10]
- Sleep apnea[11]
- Atelectasis[12]
- Restriction of breathing due to musculoskeletal abnormality or obesity
- Central nervous system deficit
- Neurological patient with muscle weakness.
- Surgical procedure such as thoracic or abdominal surgeries.[13]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Russo MA, Santarelli DM, O’Rourke D. The physiological effects of slow breathing in the healthy human. Breathe. 2017 Dec 1;13(4):298-309.
- ↑ 2.0 2.1 2.2 Patrick Mckeown. The breathing cure. City of Publication: OxyAt Books, Year.2021
- ↑ 3.0 3.1 Zisi D, Chryssanthopoulos C, Nanas S, Philippou A. The effectiveness of the active cycle of breathing technique in patients with chronic respiratory diseases: A systematic review. Heart & Lung. 2022 May 1;53:89-98.
- ↑ 4.0 4.1 Örün D, Karaca S, Arıkan Ş. The Effect of Breathing Exercise on Stress Hormones. BibTeXEndNoteRefManRefWorks
- ↑ 5.0 5.1 Hamasaki H. Effects of diaphragmatic breathing on health: a narrative review. Medicines. 2020 Oct 15;7(10):65.
- ↑ Hsu SL, Oda H, Shirahata S, Watanabe M, Sasaki M. Effects of core strength training on core stability. Journal of physical therapy science. 2018;30(8):1014-8.
- ↑ Guitonneau J, Jouvion AX, Paul F, Trappier T, De Brier G, Thefenne L. Is Physiotherapy useful for post-traumatic stress disorder in military personnel?. Annals of Physical and Rehabilitation Medicine. 2017 Sep 1;60:e55.
- ↑ Yokogawa M, Kurebayashi T, Ichimura T, Nishino M, Miaki H, Nakagawa T. Comparison of two instructions for deep breathing exercise: non-specific and diaphragmatic breathing. Journal of physical therapy science. 2018;30(4):614-8. BibTeXEndNoteRefManRefWorks
- ↑ jivan sharma. Diaphragmatic Breathing Technique. Available from: http://www.youtube.com/watch?v=0Ua9bOsZTYg [last accessed 3/4/2020]
- ↑ Mendes LP, Moraes KS, Hoffman M, Vieira DS, Ribeiro-Samora GA, Lage SM, Britto RR, Parreira VF. Effects of diaphragmatic breathing with and without pursed-lips breathing in subjects with COPD. Respiratory care. 2019 Feb 1;64(2):136-44.
- ↑ Courtney R. Breathing retraining in sleep apnoea: A review of approaches and potential mechanisms. Sleep and Breathing. 2020 Dec;24:1315-25.
- ↑ Westerdahl E, Lindmark B, Eriksson T, Hedenstierna G, Tenling A. Deep-breathing exercises reduce atelectasis and improve pulmonary function after coronary artery bypass surgery. Chest. 2005 Nov 1;128(5):3482-8.[1]
- ↑ Chuter TA, Weissman C, Mathews DM, Starker PM. Diaphragmatic breathing maneuvers and movement of the diaphragm after cholecystectomy. Chest. 1990 May 1;97(5):1110-4. •