Lung Volumes
Original Editor - Simisola Ajeyalemi Top Contributors - Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Kim Jackson, Adam Vallely Farrell and Joao Costa
Description[edit | edit source]
Lung volumes are also known as respiratory volumes. It refers to the volume of gas in the lungs at a given time during the respiratory cycle. Lung capacities are derived from a summation of different lung volumes. The average total lung capacity of an adult human male is about 6 litres of air. Lung volumes measurement is an integral part of pulmonary function test. These volumes tend to vary, depending on the depth of respiration, ethnicity, gender, age, body composition[1] and in certain respiratory diseases. A number of the lung volumes can be measured by Spirometry- Tidal volume, Inspiratory reserve volume, and Expiratory reserve volume. However, measurement of Residual volume, Functional residual capacity, and Total lung capacity is through body plethysmography, nitrogen washout and helium dilution technique.
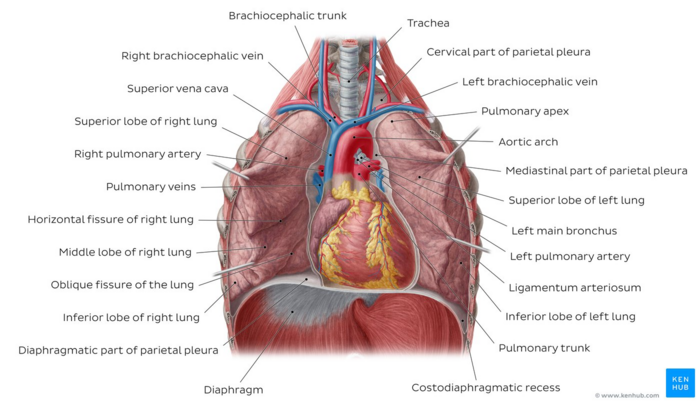
Image: Lungs in situ - anterior view [2]
Lung Volumes[edit | edit source]
- Tidal Volume(TV)
It is the amount of air that can be inhaled or exhaled during one respiratory cycle[3]. This depicts the functions of the respiratory centres, respiratory muscles and the mechanics of the lung and chest wall[4].
The normal adult value is 10% of vital capacity (VC), approximately 300-500ml (6‐8 ml/kg)[4]; but can increase up to 50% of VC on exercise[5]
- Inspiratory Reserve Volume(IRV)
It is the amount of air that can be forcibly inhaled after a normal tidal volume.IRV is usually kept in reserve, but is used during deep breathing. The normal adult value is 1900-3300ml.
- Expiratory Reserve Volume(ERV)
It is the volume of air that can be exhaled forcibly after exhalation of normal tidal volume. The normal adult value is 700-1200ml. ERV is reduced with obesity, ascites or after upper abdominal surgery[4]
- Residual Volume(RV)
It is the volume of air remaining in the lungs after maximal exhalation. Normal adult value is averaged at 1200ml(20‐25 ml/kg) .It is indirectly measured from summation of FRC and ERV and cannot be measured by spirometry.
In obstructive lung diseases with features of incomplete emptying of the lungs and air trapping, RV may be significantly high. The RV can also be expressed as a percentage of total lung capacity and values in excess of 140% significantly increase the risks of barotrauma, pneumothorax, infection and reduced venous return due to high intra thoracic pressures as noticed in patients with high RV who require surgery and mechanical ventilation thus needs high peri-operative inflation pressures. [6]
Lung capacities[edit | edit source]
- Inspiratory capacity(IC)
It is the maximum volume of air that can be inhaled following a resting state. It is calculated from the sum of inspiratory reserve volume and tidal volume. IC = IRV+TV
- Total Lung Capacity(TLC)
It is the maximum volume of air the lungs can accommodate or sum of all volume compartments or volume of air in lungs after maximum inspiration. The normal value is about 6,000mL(4‐6 L). TLC is calculated by summation of the four primary lung volumes (TV, IRV, ERV, RV).
TLC may be increased in patients with obstructive defects such as emphysema and decreased in patients with restrictive abnormalities including chest wall abnormalities and kyphoscoliosis[7].
- Vital Capacity(VC)
It is the total amount of air exhaled after maximal inhalation. The value is about 4800mL and it varies according to age and body size. It is calculated by summing tidal volume, inspiratory reserve volume, and expiratory reserve volume. VC = TV+IRV+ERV.
VC indicates ability to breathe deeply and cough, reflecting inspiratory and expiratory muscle strength.VC should be 3 times greater than TV for effective cough[8]. VC is sometimes reduced in obstructive disorders and always in restrictive disorders[8]
- Function Residual Capacity(FRC)
It is the amount of air remaining in the lungs at the end of a normal exhalation. It is calculated by adding together residual and expiratory reserve volumes. The normal value is about 1800 – 2200 mL. FRC = RV+ERV.
FRC does not rely on effort and highlights the resting position when inner and outer elastic recoils are balanced. FRC is reduced in restrictive disorders. The ratio of FRC to TLC is an index of hyperinflation[9]. In COPD, FRC is upto 80% of TLC[4].
Measurement of Lung Volumes[edit | edit source]
Measurements of lung volume are important for a correct physiological diagnosis, however, its role in the assessment of disease severity, functional disability, the course of disease and response to treatment remains controversial.[10] Measurement can be done using Spirometry see..., Body plethysmography, Nitrogen washout and Helium dilution with the latter three techniques used in measuring static lung volumes[7].
Body Plethysmography[edit | edit source]
Plethysmography is derived from Greek word meaning enlargement . Body plethysmography primarily measures FRC using Boyle's law. It is particularly appropriate for patients who have air spaces within the lung that do not communicate with the bronchial tree.
The person is seated comfortably in an airtight box(Static lung volumes can be obtained either by measuring the changes in pressure in a constant volume box or volume in a constant pressure box) in which changes in pressure and volume can be measured accurately.
Nitrogen Washout[edit | edit source]
This technique is based on washing out the N2 from the lungs, while the patient breathes 100% O2 using dilution properties of gases.
- The patient breathes 100% oxygen, and all the nitrogen in the lungs is washed out.
- The exhaled volume and the nitrogen concentration in that volume are measured.
- The difference in nitrogen volume at the initial concentration and at the final exhaled concentration allows a calculation of intrathoracic volume, usually FRC.
Helium Dilution[edit | edit source]
The method for measuring lung volumes is based on the equilibration of gas in the lung with a known volume of gas containing helium. This technique involves the subject being connected to a spirometer filled with 10% helium in oxygen. After the subject re-breathes the helium–oxygen mixture and equilibrates with the spirometer, the helium concentration in the lungs will become the same as in the spirometer. From the conservation of mass principle, we can write that: C1 × V1 = C2 (V1 + V2) Where C1 equals the initial concentration of helium in the spirometer,
- V1 equals the initial volume of helium–oxygen mixture in the spirometer,
- C2 equals helium concentration after equilibration,
- V2 equals unknown volume in the lungs.
- V2=V1 (C1-C2)/C2
- If the test begins at the end of a normal tidal volume (end of expiration), the volume of air remaining in the lungs represents FRC.
- If the test begins at the end of an FVC, then the test will measure RV.
- Similarly, if the test starts after a maximal inspiration, then V2 would equal Total lung capacity.
To further understand the technique of lung volume estimation, watch the video below
Resources[edit | edit source]
European Respiratory Journal http://erj.ersjournals.com/content/26/3/511
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC32298
Lutfi MF. The physiological basis and clinical significance of lung volume measurements.Multidisciplinary Respiratory Medicine, 2017; 12: 3
Ruppel GL. What Is the Clinical Value of Lung Volumes? Respiratory care, 2012;57(1):126–35.
References[edit | edit source]
- ↑ Maiolo C, Mohamed EI, Carbonelli MG.Body composition and respiratory function. Acta Diabetologica, 2003; 40 Suppl 1(1):S32-8 · DOI: 10.1007/s00592-003-0023-0
- ↑ Lungs in situ image - © Kenhub https://www.kenhub.com/en/library/anatomy/the-lung
- ↑ Guyton C, Hall, E. Test book of medical physiology. Elsevier Inc. Philadelphia, Pennsylvania. 2006; p.475-477.
- ↑ 4.0 4.1 4.2 4.3 Hough, A. Physiotherapy in Respiratory Care; An evidence-based approach to respiratory and cardiac management. 3rd eds. United Kingdom: Nelson Thomes Ltd, 2001 p.69
- ↑ Luce JM, Pierson DJ, Tyler MT. Intensive Respiratory Care, W. B. Saunders, Philadelphia, PA.p.21
- ↑ Wilde M, Nair S, Madden B. Pulmonary function tests-a review. Care of the Critical ill. 2007; Dec 23(6):173-7.
- ↑ 7.0 7.1 Ranu H, Wilde, M, Madden B. Pulmonary Function Test. Ulster Medical Journal, 2011; 80(2): 84–90. PMC3229853
- ↑ 8.0 8.1 Pryor JA, Webber BA. Eds. Physiotherapy for Respiratory and Cardiac problems. 2ndedition. Churchill Livingstone, London. 1998; p53-54
- ↑ Pryor JA, Webber BA. Eds. Physiotherapy for Respiratory and Cardiac problems. 2ndedition. Churchill Livingstone, London. 1998; p52-63
- ↑ Pellegrino R, Viegi G, Enright P, et al. Interpretative strategies for lung function testing. Eur Respir J 2005; (In press).