Scoliosis
Definition/Description[edit | edit source]
Scoliosis is an abnormal lateral curvature of the spine. It is most often diagnosed in childhood or early adolescence.
The spine's normal curves occur at the cervical, thoracic and lumbar regions in the so-called “sagittal” plane. These natural curves position the head over the pelvis and work as shock absorbers to distribute mechanical stress during movement. Scoliosis is often defined as spinal curvature in the “coronal” (frontal) plane. While the degree of curvature is measured on the coronal plane, scoliosis is actually a more complex, three-dimensional problem which involves the following planes:
- Coronal plane
- Sagittal plane
- Axial plane
The coronal plane is a vertical plane from head to foot and parallel to the shoulders, dividing the body into anterior (front) and posterior (back) sections. The sagittal plane divides the body into right and left halves. The axial plane is parallel to the plane of the ground and at right angles to the coronal and sagittal planes.[1]
- Scoliosis is defined by the Cobb's angle of spine curvature in the coronal plane and is often accompanied by vertebral rotation in the transverse plane and hypokyphosis in the sagittal plane.
- These abnormalities in the spine, costal-vertebral joints, and the rib cage produce a ‘convex’ and ‘concave’ hemithorax.
- The rotation component starts when the scoliosis becomes more pronounced. This is called a torsion-scoliosis, causing a gibbus.[2][3]
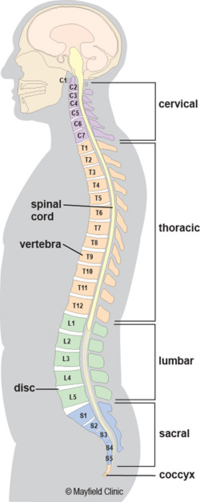
Clinically Relevant Anatomy[edit | edit source]
The vertebral column normally consists of 24 separate bony vertebrae, together with 5 fused vertebrae that form the sacrum, and usually, 4 fused vertebrae that form the coccyx
Variations can occur such as hemi-vertebrae and fused vertebrae.
When viewed from the side, the vertebral column displays five curves in the upright posture:[4]
- Cervical curves
2 normally occurring curves in the cervical spine: the upper cervical curve extending from the occiput to the axis, and the longer lordotic curve of the lower cervical spine extending from the axis to the second thoracic vertebrae. The upper cervical curve is convex forwards and is the reverse of the lower cervical curve. - Thoracic curve
Concave forwards, extending from T2 to T12. The concavity is due to the greater depth of the posterior parts of the vertebral bodies in this region. In the upper part there is often a slight lateral curve with the convexity directed to either the right or left. - Lumbar curve
Convex forwards and extends from L1 to the lumbosacral junction. - Sacral curve
Extends from the lumbosacral junction to the coccyx, anterior concavity faces downwards and forwards.
Epidemiology[edit | edit source]
- Scoliosis affects 2-3 percent of the population, or an estimated six to nine million people in the United States.
- Scoliosis can develop in infancy or early childhood.
- The primary age of onset for scoliosis is 10-15 years old, occurring equally among both genders.
- Females are eight times more likely to progress to a curve magnitude that requires treatment.
- Every year, scoliosis patients make more than 600,000 visits to private physician offices, an estimated 30,000 children are fitted with a brace and 38,000 patients undergo spinal fusion surgery (US figures)[1]
Etiology[edit | edit source]
Scoliosis can be classified by etiology: idiopathic, congenital or neuromuscular.
- The diagnosis when all other causes are excluded and comprises about 80 percent of all cases.
- Adult scoliosis has a prevalence of more than 8 % in adults over the age of 25 and rises up 68 % in the age of over 60 years, caused by degenerative changes in the aging spine.[5] and a prevalence of 2,5 % in the general population with a Cobb angle larger than 10 degrees[2].
- Adolescent idiopathic scoliosis is the most common type of scoliosis and is usually diagnosed during puberty.
Classified into the following subgroups:
- Infantile scoliosis: Infantile scoliosis develops at the age of 0–3 years and shows a prevalence of 1 %.
- Juvenile scoliosis: Juvenile scoliosis develops at the age of 4–10 years, comprises 10–15 % of all idiopathic scoliosis in children, untreated curves may cause serious cardiopulmonary complications, and curves of 30 and more tend to progress, 95 % of these patients need a surgical procedure.
- Adolescent scoliosis: Adolescent scoliosis develops at the age of 11–18 years, accounts for approximately 90 % of cases of idiopathic scoliosis in children.
- Results from embryological malformation of one or more vertebrae and may occur in any location of the spine.
- The vertebral abnormalities cause curvature and other deformities of the spine because one area of the spinal column lengthens at a slower rate than the rest.
- The geometry and location of the abnormalities determine the rate at which scoliosis progresses in magnitude as the child grows
- As these abnormalities are present at birth, congenital scoliosis is usually detected at a younger age than idiopathic scoliosis.
Neuromuscular scoliosis
- Encompasses scoliosis that is secondary to neurological or muscular diseases.
- Includes scoliosis associated with cerebral palsy, spinal cord trauma, muscular dystrophy, spinal muscular atrophy and spina bifida.
- This type of scoliosis generally progresses more rapidly than idiopathic scoliosis and often requires surgical treatment.[1]
Injuries and infections to the spine can also contribute to the cause of scoliosis
Characteristics/Clinical Presentation[edit | edit source]
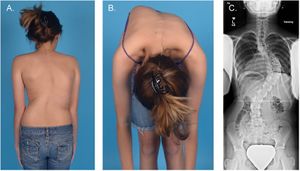
There are several signs that may indicate the possibility of scoliosis.
- Sideways curvature of the spine
- Sideways body posture
- One shoulder raised higher than the other
- Clothes not hanging properly
- Local muscular aches
- Local ligament pain
- Decreasing pulmonary function, major concern in progressive severe scoliosis.
In one study, about 23 percent of patients with idiopathic scoliosis presented with back pain at the time of initial diagnosis. Ten percent of these patients were found to have an underlying associated condition such as spondylolisthesis, syringomyelia, tethered cord, herniated disc or spinal tumor. If a patient with diagnosed idiopathic scoliosis has more than mild back discomfort, a thorough evaluation for another cause of pain is advised.
Due to changes in the shape and size of the thorax, idiopathic scoliosis may affect pulmonary function. Recent reports on pulmonary function testing in patients with mild to moderate idiopathic scoliosis showed diminished pulmonary function. Impairment of function was seen in more severe cases of spinal deformity, proximally-located curvature and older patients.[6][1]
Diagnosis[edit | edit source]
- Scoliosis is usually confirmed through a physical examination, an x-ray, spinal radiograph, CT scan or MRI.
- The curve is measured by the Cobb Method and is diagnosed in terms of severity by the number of degrees. See link
- .A standard exam that is sometimes used by pediatricians and in grade school screenings is called the Adam's Forward Bend Test. See link.[1]
Outcome Measures[edit | edit source]
Evaluation of scoliosis treatment should include the patient’s perspective, obtained with the use of patient-reported outcome measures.
- SF-36 questionnaire and the EuroQol5D instrument[7].
- SRS-22 Patient Questionnaire and the quality of life profile for spinal deformities (QLPSD).
- The perception of the trunk deformity and body image according to the patient can be assessed by several instruments eg Walter-Reed Visual Assessment Scale (WRVAS)[8], Spinal Appearance Questionnaire (SAQ)[9],Trunk Appearance Perception Scale (TAPS)[10].
- The impacts of the brace use can be measured with specific scales: Bad Sobernheim Stress Questionnaire (BSSQ) & Brace Questionnaire (BrQ).
NB available instruments to evaluate the treatment for non-idiopathic scoliosis have not been sufficiently validated and analysed.[11]
Examination[edit | edit source]
The aim of the functional examination is to distinguish between faulty posture and actual idiopathic scoliosis
- Examination of the active movements(flexion, extension and side flexion) of the spine in the cervical, thoracic and lumbar segment.
2. The Adam forward bend test can be used to make a distinction between structural scoliosis or non-structural scoliosis of the cervical to lumbar spine. The test can be performed in the standing and sitting position. See image R
.3. The Cobb angle is a standard measurement to determine and track the progression of scoliosis: see lower image R
.4. The scoliometer is an inclinometer designed to measure trunk asymmetry, or axial trunk rotation. It’s used at three areas:
- Upper thoracic (T3-T4)
- Middle thoracic (T5-T12)
- Thoraco-lumbar area (T12-L1 or L2-L3)
If the measurement is equal to 0°, there is a symmetry at the particular level of the trunk. An asymmetry at the particular level of the trunk is found, if the scoliometer measurement is equal to any other value.[12]
5. Pulmonary function testing is useful in the preoperative evaluation of patients.[6]
Spirometer
- FVC gives an assessment of lung volume
- FEV1 provides an assessment of flow function.
Medical Management[edit | edit source]
Patients with early-onset scoliosis, defined as a lateral curvature of the spine under the age of 10 years, are offered surgical treatment when the major curvature remains progressive despite conservative treatment (Cobb angle 50 degrees or more). Spinal fusion is not recommended in this age group, as it prevents spinal growth and pulmonary development.[13]
Conservative Treatment[edit | edit source]
Most people with scoliosis have mild curves and probably won't need treatment with a brace or surgery. Children who have mild scoliosis may need regular checkups to see if there have been changes in the curvature of their spines as they grow.
Braces[edit | edit source]
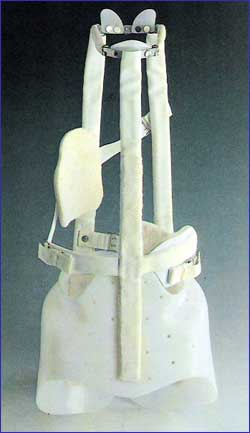
When children's bones are still growing and he or she has moderate scoliosis, the doctor may recommend a brace. Wearing a brace won't cure scoliosis or reverse the curve, but it usually prevents further progression of the curve.
- The most common type of brace is made of plastic and is contoured to conform to the body. This brace is almost invisible under the clothes, as it fits under the arms and around the rib cage, lower back and hips. eg Milwaukee brace
- Most braces are worn day and night. A brace's effectiveness increases with the number of hours a day it's worn. Children who wear braces can usually participate in most activities and have few restrictions. If necessary, kids can take off the brace to participate in sports or other physical activities.
Braces are discontinued after the bones stop growing. This typically occurs:
- About two years after girls begin to menstruate
- When boys need to shave daily
- When there are no further changes in height[14]
In general, most congenital scoliotic curves are not flexible and therefore are resistant to repair with bracing. For this reason, the use of braces mainly aims to prevent the progression of secondary curves that develop above and below the congenital curve, causing imbalance. In these cases, they may be applied until skeletal maturity[15].
Surgical Treatment[edit | edit source]
Severe scoliosis typically progresses with time
A specialist may suggest scoliosis surgery to reduce the severity of the spinal curve and to prevent it from getting worse.
- The most common type of scoliosis surgery is spinal fusion.
- In spinal fusion two or more of the vertebrae are fused together, so they can't move independently. Pieces of bone or a bone-like material are placed between the vertebrae. Metal rods, hooks, screws or wires typically hold that part of the spine straight and still while the old and new bone material fuses together.
- If the scoliosis is progressing rapidly at a young age, surgeons can install a rod that can adjust in length as the child grows. This growing rod is attached to the top and bottom sections of the spinal curvature, and is usually lengthened every six months.
- Complications of spinal surgery may include bleeding, infection, pain or nerve damage. Rarely, the bone fails to heal and another surgery may be needed.[14]
Physical Therapy Management[edit | edit source]
- Physical therapy and bracing are used to treat milder forms of scoliosis to maintain cosmesis and avoid surgery.[16]
- Scoliosis is not just a lateral curvature of the spine, it’s a three dimensional condition.
- To manage scoliosis work in three planes: the sagittal, frontal and transverse.[15]
Conservative therapy consists of:
- physical exercises
- bracing
- manipulation
- electrical stimulation
- insoles.[17]
The physical therapist has three important tasks
Inform, advise and instruct.
- Important to do the correct exercises
- Inform the patient &/or parents about his/her situation.
- Some physical therapists recommend a brace to prevent the worsening of scoliosis. eg Milwaukee brace. Nevertheless, the evidence for bracing is controversial.[18]
- There is evidence that exercises have beneficial effects on patients with idiopathic scoliosis.[19]
- Physiotherapists may also address biopsychosocial factors.
- Adolescents who are presenting with idiopathic scoliosis and chronic low back pain symptoms may also have other factors such as insomnia, depression, anxiety and stress, and daytime sleepiness that need to be assessed and addressed as contributing factors to a chronic low back pain experience.[20]
Aims[edit | edit source]
The aims of physical therapy are: [21] [19]
- Autocorrection 3D
- Coordination
- Equilibrium
- Ergonomical corrections
- Muscular endurance/ strength
- Neuromotor control of the spine
- Increase of ROM
- Respiratory capacity/ education
- Side-shift
- Stabilization
Exercises[edit | edit source]
The Schroth Method is a nonsurgical option for scoliosis treatment.
It uses exercises customized for each patient to return the curved spine to a more natural position. The goal of Schroth exercises is to de-rotate, elongate and stabilize the spine in a three-dimensional plane. This is achieved through physical therapy that focuses on:
- Restoring muscular symmetry and alignment of posture
- Breathing into the concave side of the body
- Teaching you to be aware of your posture[22]
- The purpose of these exercises is to derotate, deflex and to correct the spine in the sagittal plane while elongating the spine.[15]
Image at R - Patient with right thoracic scoliosis (functional 3-curve pattern as seen on the left) performing the 'Door handle exercise' according to the new 'Power Schroth' principles. The corrected head alignment is not yet achieved but correction of the sagittal profile is already visible.
Patient with right thoracic scoliosis (functional 3-curve pattern as seen on the left) performing the exercise 'Frog at the pond' according to the new 'Power Schroth' principles (right). The corrected head alignment is not yet achieved but correction of the sagittal profile is already visible.
- The patient needs to be focused about re-establishing spinal symmetry.
- The key to a successful therapy is to work consistently to correct the spine.
- A difficult part of the therapy is to learn to shorten the muscles on the convex side of the spine and lengthen the muscles on the concave side of the side (muscles become imbalanced on opposite sides.[23])
- The exercise position approaches the functional/structural threshold.
- Schroth therapy takes advantage of the overcorrected positions.
- Basic corrections are reviewed by using mirrors in front and at the back of the patient.
- This posture requires concentration and coordination, applying the correct breathing, and well-adapted muscle length and tension.[17]
There are also other exercises that have been found effective eg Scientific Exercises Approach to Scoliosis (SEAS) exercises.
- Effective in reducing the rate of progression of scoliosis compared with usual care and help to avoid brace prescription. Evidence also supports that SEAS is found to be effective in reducing spinal deformities compared with control groups.[19] [25] [26]
- The SEAS exercises are, according to the Italian Scientific Spine Institute (ISICO), based on a specific form of Active Self-correction (ASC), that is taught individually to each single patient.
- This is to achieve the maximum possible correction. ASC is then associated with stabilizing exercises that include neuromotor control, proprioceptive training and balance.
- The exercises are also incorporated into their daily living activities.
- SEAS approach involves the parents getting together with the child on a cognitive-behavioral approach to maximize compliance to treatment.[19] [21]
Klapp Exercises are another exercise program. It was a nonsurgical method established with the aim of correcting the spinal curvature by stretching and strengthening the back muscles.[27] See link.
Breathing exercises combined with the thoracic active mobilisations are another important aspect of physiotherapy.
- The severity of the curvature can cause a pressure on airways and lungs.
- The patient can experience trouble while breathing.
- If the risk of pulmonary dysfunction (as a result of the pressure of the spine) is too high, surgery is indicated.[18]
A study into the effectiveness of a respiratory rehabilitation program in children with scoliosis that included:
- Respiratory education techniques (abdominal-diaphragmatic ventilation, thoracic mobilisation, ventilation at rest and during activities of daily living) for mobilisation and prevention of stiffness of chest and skeletal muscles.
- Postural drainage and vibration to evacuate mucus and decrease the resistance of the airways.
- Relaxation techniques to make sure that the patients would have better control of respiration (to counteract dyspnea).
It found that the respiratory rehabilitation had a positive effect on increasing pulmonary function of children with scoliosis.[21]
Management of Non–Structural scoliosis[edit | edit source]
The management of non-structural scoliosis include:[19]
Pilates: This intervention was divided into three parts:
Preparation (warm up + stretch)
Warm-up consisted of eight minutes walking on a treadmill or an elliptical machine. After the warm-up each patient had to do some stretching exercises:
- Spine forward stretching: The patient sits on the floor with a straight back and the legs stretched. The patient has to bring the trunk forwards. Goal: Stretching the posterior muscle chain and mobilizing the vertebral spine
- Upper rolling: The patient lies supine with the arms besides the body. The patient has to raise both legs till the toes touches the floor. Then, unroll spine slowly (vertebra by vertebra) Goal: stretching the posterior chain, mobilizing the spine and strengthen the abdomen.
- Child position: The patient sits in a four support position and has to stretch the spine, arms and push the hands against the floor. Then lower the spine. Goal: Stretching the thoracic paravertebral, lumbar and gluteal regions and mobilizing the vertebral spine
- Forward leg pull: The patient sits in a four support position. Then raises the right arm and leg while the spine stays aligned. Than the same exercise but change arm and leg. Goal: Stretching the concavity of the vertebral spine.
Specific exercises: For these exercise Swiss balls, FlexBall Quarks are used. It’s important that the patients learn to breath right during exercise.
- Hip movements with a large ball (65 cm diameter). Goal: Strengthening the gluteal muscles and developing the equilibrium.
- Inverted abdominal skills with a ball (55 cm diameter). Goal: Strengthening the infraabdominal region and the ischiotibial muscles.
- Rising into a seated position. Goal: Strengthening the M. rectus abdominis.
- Lateral spine movement on a step chair with a spring of 0.1410 kg positioned in the rings to provide major resistance. Goal: Stretching the lateral muscle chain according to the direction of convexity of the scoliosis.
- Lateral spine movement. Goal: Stretching the lateral muscle chain according to the direction of convexity of the scoliosis.
- Flexibility on the step chair with a spring of 0,1410 kg positioned in the rings to provide major resistance. Goal: Mobilize the spine and stretch the paravertebral thorax and lumbar muscles.
Returning to a relaxed position (relaxation) :It consist of three movements, the patient has to repeat each exercise three times for five minutes. All exercises has to be performed rapidly. The purpose of these exercises are metabolic recovery and relaxation of the used muscles.
Clinical Bottom Line[edit | edit source]
In conclusion it’s important to make a good diagnosis about the kind of scoliosis and the cause of the scoliosis.
- Management interventions should be weighed with the choices and complaints of the patient and the kind of scoliosis the patient is suffering from.
- It’s important to note that not all patients with scoliosis are actually suffering from this spine deformation.
- Every patient is different and deserves attention to deploy the appropriate treatment
- Coping with scoliosis is difficult for a young person in an already complicated stage of life. Teens are bombarded with physical changes and emotional and social challenges. With the added diagnosis of scoliosis, anger, insecurity and fear may occur.
- A strong, supportive peer group can have a significant impact on a child's or teen's acceptance of scoliosis, bracing or surgical treatment. Encourage the child to talk to his or her friends and ask for their support.[14]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 ANNS Scoliosis Available from:https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Scoliosis Last accessed 18.4.2020
- ↑ 2.0 2.1 Anwer S, Alghadir A, Shaphe A, Anwar D. Effects of exercise on spinal deformities and quality of life in patients with adolescent idiopathic scoliosis. BioMed research international. 2015;2015.
- ↑ Hacquebord JH, Leopold SS. In brief: The Risser classification: a classic tool for the clinician treating adolescent idiopathic scoliosis. Clin Orthop Relat Res. 2012;470(8):2335–2338.
- ↑ Alison Middleditch et al., Functional Anatomy of the Spine 2005 2-6p.
- ↑ Konieczny MR, Senyurt H, Krauspe R. Epidemiology of adolescent idiopathic scoliosis. J Child Orthop. 2012;7(1):3–9.
- ↑ 6.0 6.1 Johari J, Sharifudin MA, Ab Rahman A, Omar AS, Abdullah AT, Nor S, Lam WC, Yusof MI. Relationship between pulmonary function and degree of spinal deformity, location of apical vertebrae and age among adolescent idiopathic scoliosis patients. Singapore medical journal. 2016 Jan;57(1):33.
- ↑ Balestroni G, Bertolotti G. EuroQol-5D (EQ-5D): an instrument for measuring quality of life. Monaldi Archives for Chest Disease. 2015 Dec 1;78(3).
- ↑ Pineda S, Bago J, Gilperez C, Climent JM. Validity of the Walter Reed Visual Assessment Scale to measure subjective perception of spine deformity in patients with idiopathic scoliosis. Scoliosis. 2006 Dec;1(1):18.
- ↑ Carreon LY, Sanders JO, Polly DW, Sucato DJ, Parent S, Roy-Beaudry M, Hopkins J, McClung A, Bratcher KR, Diamond BE, Spinal Deformity Study Group. Spinal appearance questionnaire: factor analysis, scoring, reliability, and validity testing. Spine. 2011 Aug 15;36(18):E1240-4.
- ↑ Bago J, Sanchez-Raya J, Perez-Grueso FJ, Climent JM. The Trunk Appearance Perception Scale (TAPS): a new tool to evaluate subjective impression of trunk deformity in patients with idiopathic scoliosis. Scoliosis. 2010 Dec;5(1):6.
- ↑ Juan Bago´ et al., Outcome instruments to assess scoliosis surgery, Eur Spine J (2013) 22 (Suppl 2):S195–S202.
- ↑ Patias P, Grivas TB, Kaspiris A, Aggouris C, Drakoutos E. A review of the trunk surface metrics used as Scoliosis and other deformities evaluation indices. Scoliosis. 2010 Dec;5(1):12.
- ↑ Helenius IJ. Treatment strategies for early-onset scoliosis. EFORT open reviews. 2018 May;3(5):287-93.
- ↑ 14.0 14.1 14.2 Mayo Clinic Scoliosis Available from:https://www.mayoclinic.org/diseases-conditions/scoliosis/diagnosis-treatment/drc-20350721 (last accessed 18.4.2020)
- ↑ 15.0 15.1 15.2 Kaspiris A, Grivas TB, Weiss HR, Turnbull D. Surgical and conservative treatment of patients with congenital scoliosis: α search for long-term results. Scoliosis. 2011 Dec;6(1):12.
- ↑ Jonathan A. et al., A comprehensive review of thoracic deformity parameters in scoliosis, Eur Spine J (2014) 23:2594–2602.
- ↑ 17.0 17.1 Fusco C, Zaina F, Atanasio S, Romano M, Negrini A, Negrini S. Physical exercises in the treatment of adolescent idiopathic scoliosis: an updated systematic review. Physiotherapy theory and practice. 2011 Jan 1;27(1):80-114.
- ↑ 18.0 18.1 Maruyama T, Grivas TB, Kaspiris A. Effectiveness and outcomes of brace treatment: a systematic review. Physiotherapy theory and practice. 2011 Jan 1;27(1):26-42.
- ↑ 19.0 19.1 19.2 19.3 19.4 Negrini S, Zaina F, Romano M, Negrini A, Parzini S. Specific exercises reduce brace prescription in adolescent idiopathic scoliosis: a prospective controlled cohort study with worst-case analysis. Journal of rehabilitation medicine. 2008 Jun 5;40(6):451-5.
- ↑ Wong AY, Samartzis D, Cheung PW, Cheung JP. How Common Is Back Pain and What Biopsychosocial Factors Are Associated With Back Pain in Patients With Adolescent Idiopathic Scoliosis?. Clinical Orthopaedics and Related Research®. 2019 Apr 1;477(4):676-86.
- ↑ 21.0 21.1 21.2 Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, Diers H, Grivas TB, Knott P, Kotwicki T, Lebel A. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis and spinal disorders. 2018 Dec;13(1):3.
- ↑ John Hopkins Schroth Method for Scoliosis. Available from:https://www.hopkinsmedicine.org/health/conditions-and-diseases/scoliosis/schroth-method-for-scoliosis (last accessed 18.4.2020)
- ↑ Schreiber S, Parent EC, Moez EK, Hedden DM, Hill DL, Moreau M, Lou E, Watkins EM, Southon SC. Schroth physiotherapeutic scoliosis-specific exercises added to the standard of care lead to better Cobb angle outcomes in adolescents with idiopathic scoliosis–an assessor and statistician blinded randomized controlled trial. PloS one. 2016 Dec 29;11(12):e0168746.
- ↑ Scoliosis Systems LLP Powered by Scoli-Fit. Scoli-Fit Exercises for Scoliosis. Available from: https://www.youtube.com/watch?v=JUXcQvzx2H0 [last accessed 31/10/2021]
- ↑ Negrini S, Negrini A, Romano M, Verzini N, Negrini A, Parzini S. A controlled prospective study on the efficacy of SEAS. 02 exercises in preventing progression and bracing in mild idiopathic scoliosis. Studies in health technology and informatics. 2006;123:523.
- ↑ Negrini A, Parzini S, Negrini MG, Romano M, Atanasio S, Zaina F, Negrini S. Adult scoliosis can be reduced through specific SEAS exercises: a case report. Scoliosis. 2008 Dec;3(1):20.
- ↑ Orthopedics: A History and Iconography- Leonard Peltier