Biopsychosocial Model
Introduction[edit | edit source]
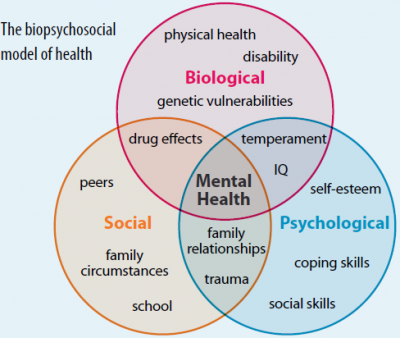
The Biopsychosocial model was first conceptualised by George Engel in 1977, suggesting that to understand a person's medical condition it is not simply the biological factors to consider, but also the psychological and social factors [1].
- Bio (physiological pathology)
- Psycho (thoughts emotions and behaviours such as psychological distress, fear/avoidance beliefs, current coping methods and attribution)
- Social (socio-economical, socio-environmental, and cultural factors suchs as work issues, family circumstances and benefits/economics)
This model is commonly used in chronic pain,[2] with the view that the pain is a psychophysiological behaviour pattern that cannot be categorised into biological, psychological, or social factors alone. There are suggestions that physiotherapy should integrate psychological treatment to address all components comprising the experience of chronic pain.
The diagram below shows an example of this model.
Diagram of the Biopsychosocial model. [3]
Physiotherapists must know how biopsychosocial factors interact in patients with chronic pain to explain the perpetuation of this condition and use it as a basis for planning the intervention program. The evidence has suggested a clinical biopsychosocial assessment for the physiotherapeutic management of patients with chronic pain in order to understand and explain the predominant mechanism of pain and psychosocial factors that may or may not be modified for the patient to improve their condition.[4]
This clinical evaluation is carried out during the data collection at the patient's entrance. A practical guide is proposed to take biopsychosocial data using the PSCEBSM (Pain–Somatic and medical factors–Cognitive factors–Emotional factors–Behavioral factors–Social factors–Motivation) model.[4]
P- Type of pain[edit | edit source]
Clinical identification and differentiation of the dominant pain mechanism:
- nociceptive pain
- neuropathic pain
- non-neuropathic pain of central sensitization.
Using the following tools:
- Classification criteria for differentiating predominant pain proposed by Nijs et al.
- Widespread pain index/Body Diagram : ≥ 7 score suggesting generalized pain, therefore, non-neuropathic pain of central sensitization
- Central Sensitization Inventory (CSI) : 40 score suggesting non-neuropathic pain of central sensitization
S- Somatic and medical factors[edit | edit source]
For physical therapist the physical examination is a very important part of his intervention - essential to:
- Be aware that some findings of clinical examinations such as mobility, strength, neurodynamics, coordination, etc. could be altered because there is greater sensitivity to mechanical stimulation and modified movement patterns in patients with non-neuropathic pain of central sensitization.
- Main goal in this stage is to evaluate the quality of movement, if the pattern of movement causes the pain to persist and if there is kinesiofobia
- Ask about current or previous health conditions, the disuse of body parts, changes in movement patterns, exercise capacity, strength and muscle tone during movement, the action of the drug in the CNS It is useful for data collection
C- Cognition / Perceptions[edit | edit source]
Both influence biologically on hypersensitivity in the brain by activating neuromatrix pain and also influence the emotional and behavioral factors. :
- Ask about perceptions: expectations of the intervention, expectations of the prognosis of their pain, understanding of their situation and the strategies they have available to face their situation, what the pain represents emotionally
- Brief Illness Perception Questionnaire (Brief IPQ)
- Pain Catastrophizing Scale (PCS)
E- Emotional factors[edit | edit source]
Ask if there is fear of specific movements, avoidance behaviors, psychological traumatic appearance of pain, psychological problems at work, family, finances, society, etc. It is also suggested to use the following scales:
- State-Trait Anxiety Inventory (STAI)
- Tampa-Scale of Kinesiophobia (TSK) and Fear Avoidence Belief Questionare
- Injustice Experience Questionnaire (IEQ)
- Patient Health Questionnaire-2 (PHQ-2), or Patient Health Questionnaire-9 (PHQ-9), or Center of Epidemiologic Studies Depression Scale (CES-D)
B- Behavioral factors[edit | edit source]
Can lead to avoid activity or movement due to fear, which in turn is presented as physical inactivity or disuse and, finally, disability. Therefore it is important to evaluate the behavior and adaptations that the patient has made due to the pain.
S- Social factors[edit | edit source]
It refers to the social and environmental factors in which the patient develops, which could be useful and supportive or harmful and stressful for the improvement of the patient's health condition. The data collection can be divided as follows:
- Housing or living situation
- Social environment
- Work
- Relationship with the partner
- Previous interventions
M- Motivation[edit | edit source]
Evaluating the motivation in the patient and his willingness to change is useful to modify his thoughts regarding the relationship pain-kinesiophobia, pain-disability, and acceptance-catastrophism. For this purpose, the following scale can be used:
- Psychology Inflexibility in Pain Scale (PIPS)
- PIPS "evaluates components of psychological inflexibility (avoidance and fusion)"[5]
Clinical Contribution[edit | edit source]
- The use of the biopsychosocial model as a clinical practice guide in physiotherapy allows the physiotherapist to be aware of all the factors that influence the patient's state of health. In addition, it allows laying the foundations of pain neuroscience education
- The psychosocial factors the patient deals with can mean the intervention of other health professionals besides the physiotherapist ie important to take into account the professional limits, as well as the ethical principles that ensure the comprehensive management of the patient.
The following videos emphasise the importance of using the biopsychosocial model to improve patient functionality and the problem that currently exists for physiotherapists in the use of this approach.
Criticisms of the model[edit | edit source]
- There is still minimal use of the biopsychosocial model in education, clinical care, and research. The biopsychosocial model cannot be consistently defined for an individual (data is not obtained systematically, making it untestable and non-scientific).
- Patient centered interview methods have been suggested to be used in practice, such that clinicians can identify a scientific BPS model specific to each patient with an agreed-upon, evidence-based patient-centered interviewing method can be more useful as these are reproducible and can elicit relevant patient information.[6]
Additional Resource[edit | edit source]
Wijma AJ, van Wilgen CP, Meeus M, Nijs J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: The first step in pain neuroscience education. Physiotherapy theory and practice. 2016 Jul 3;32(5):368-84
References[edit | edit source]
- ↑ Gatchel, Robert J., Peng, Yuan Bo, Peters, Madelon, L.; Fuchs, Perry, N.; Turk, Dennis C. 2007 The biopsychosocial approach to chronic pain: Scientific advances and future directionsfckLR Psychological Bulletin, Vol 133(4), 581-624
- ↑ Miaskowski C, Blyth F, Nicosia F, Haan M, Keefe F, Smith A, Ritchie C. A biopsychosocial model of chronic pain for older adults. Pain Med. 2020 Sep 1;21(9):1793-1805.
- ↑ http://savvywillingandable.wordpress.com/2013/09/25/the-biopsychosocial-model-explained/
- ↑ 4.0 4.1 Wijma, A. J., van Wilgen, C. P., Meeus, M., & Nijs, J. 2016 Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: The first step in pain neuroscience education. Physiotherapy theory and practice, 32(5), 368-384.
- ↑ Nagasawa Y, Shibata A, Fukamachi H, Ishii K, Wicksell RK, Oka K. The Psychological Inflexibility in Pain Scale (PIPS): validity and reliability of the Japanese version for chronic low back pain and knee pain. J Pain Res. 2021 Feb 4;14:325-332.
- ↑ Smith, Fortin, Dwamena, & Frankel. 2013. An evidence-based patient-centered method makes the biopsychosocial model scientific. Patient Education and Counseling, 91(3), 265-270.