Muscular Dystrophy
lOriginal Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Jess Bell, Robin Tacchetti, Vidya Acharya, Rucha Gadgil, Shreya Pavaskar, Olajumoke Ogunleye, Tarina van der Stockt, Kim Jackson, Uchechukwu Chukwuemeka and Kehinde Fatola
Introduction[edit | edit source]
Muscular dystrophy refers to a group of hereditary disorders that cause progressive, generalised muscle weakness and atrophy. Muscular dystrophy is a non-communicable disorder and has many variations - each variation has a specific inheritance pattern, time of onset and rate of muscle loss.[1]
Aetiology[edit | edit source]
In most cases, muscular dystrophy is caused by absent or defective glycoproteins in the muscle membrane. In each type of muscular dystrophy, different genes are deleted or mutated. These changes can impact various enzymatic or metabolic functions.
The gene that causes Duchenne muscular dystrophy was discovered in 1986.[2] The muscle protein associated with this gene was named "dystrophin".[3] Dystrophin forms an integral part of a muscle's cytoskeleton - it links the contractile apparatus to the sarcolemma. "Absence or reduced expression of dystrophin or many of the [dystrophin protein complex] components cause the muscular dystrophies."[3]
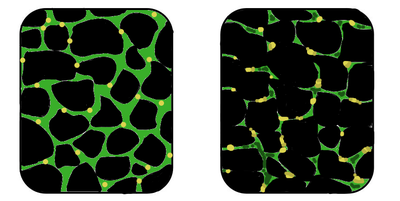
The image on the right shows muscle tissue in an individual with muscular dystrophy. The tissue in this image is disorganised, and there is a reduced concentration of dystrophin (the area shown in green).[4]
- The dystrophin gene is the largest gene in the human genome.[1] Because of its large size, it is prone to high rates of spontaneous mutations.[1]
- Duchenne muscular dystrophy (DMD) occurs when the dystrophin gene stops making dystrophin.[2]
- Becker muscular dystrophy is associated with a different mutation on the dystrophin gene, causing it to no longer make enough dystrophin (or the quality is low).[2]
- Most muscular dystrophies are X-linked recessive disorders, so muscular dystrophy is more common in biological males.[2][5]
Epidemiology[edit | edit source]
Overall prevalence:[6]
- Muscular Dystrophy: 3.6 per 100,000 people
- Duchenne Muscular Dystrophy: 4.6 per 100,000 people
- Becker Muscular Dystrophy: 1.6 per 100,000 people
The highest prevalence is in the Americas, with 5.1 per 100,000 people. The lowest prevalence is in Africa, with 1.7 per 100,000.[6]
Management[edit | edit source]
There is no cure for muscular dystrophy, but appropriate treatment can help manage symptoms and improve quality of life.
1. Medical interventions include:[1]
- anti-arrhythmic drugs
- anti-epileptic drugs
- anti-myotonic drugs
- non-steroidal anti-inflammatory drugs (NSAIDs)
- steroids
2. Surgical interventions include:[1]
- placement of defibrillator or pacemaker
- release of contractures
- spinal correction
3. Other interventions can include:[1]
- supportive physiotherapy
- supportive bracing
- supportive counselling
- genetic counselling
Physiotherapy[edit | edit source]
The goal of physiotherapy is to improve strength in the large muscle groups and prevent scoliosis and contractures.
According to the literature, the role of strengthening exercises for muscular dystrophy is controversial for two reasons:[7]
- since muscular dystrophy results in a progressive loss of muscle mass and strength, exercise may be considered harmful because it can induce damage, inflammation, and failure of the muscles to repair themselves - there is a risk it could have negative effects, including overwork weakness after supramaximal, high-intensity exercise[8]
- a lack of physical activity may lead to functional loss, weight gain, fatigue, and an exacerbation / acceleration of the effects of muscular dystrophy.
A systematic review and meta-analysis by Gianola et al.[8] explored the evidence for muscular exercise in patients with muscular dystrophy. They found that muscular exercise resulted in some modest improvements in endurance while walking in individuals with muscular dystrophy, but that it could not be "recommended for strength improvement, management of motor abilities or fatigue reduction".[8]
It has also been found that eccentric exercises and resistive / high-load exercises are worse for muscles, causing more muscle breakdown. Isometric activities or body weight resisted activities, that are appropriately graded to avoid excessive fatigue are more beneficial.[5]
Therapy for muscular dystrophy focuses on:[1][2][5]
- Maintaining ambulation / independent mobility for as long as possible
- Range of motion exercises and stretching, focusing on joints that tend to develop contractures sooner
- Low-impact workouts, such as stationary cycling, swimming / aquatic exercise
- Supportive bracing - to help maintain function for as long as possible
- Moulded ankle-foot orthoses - used to help with gait in individuals with foot drop to prevent tripping or to provide support and comfort
- Lightweight plastic ankle-foot orthoses (AFOs) are considered very useful for foot-drop
- Appropriate wheelchair seating or other assistive technology devices
- Non-invasive ventilation
Complications[edit | edit source]
The complications of muscular dystrophy depend on the type. Progressive muscle weakness can affect an individual's ability to walk, breathe, swallow, and speak. Complications can include but are not limited to:[2]
- Breathing problems. Progressive weakness in the respiratory muscles affects respiration - this increases the risk for respiratory infections like pneumonia.
- Scoliosis.
- Cardiovascular issues, including arrhythmias, congestive heart failure and dilated cardiomyopathy.[1] Many individuals with muscular dystrophy die before the age of 30 years due to cardiopulmonary failure.[1]
- Swallowing difficulties. Weakness of the muscles of the oesophagus impacts chewing and swallowing and can result in choking.
- Contractures. Most individuals with muscular dystrophy develop joint contractures at the elbow, hip, knee, and ankle.[1]
- Cataracts.[9][10]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 LaPelusa A, Kentris M. Muscular Dystrophy. StatPearls [Internet]. 2020 Jul 21.Available from: https://www.ncbi.nlm.nih.gov/books/NBK560582/(accessed 24.2.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 WebMD MD Available from: https://www.webmd.com/children/understanding-muscular-dystrophy-basics?page=-1281(accessed 24.2.2021).
- ↑ 3.0 3.1 Allen DG, Whitehead NP, Froehner FC. Absence of Dystrophin Disrupts Skeletal Muscle Signaling: Roles of Ca2+, Reactive Oxygen Species, and Nitric Oxide in the Development of Muscular Dystrophy. Physiol Rev. 2016; 96(1): 253–305.
- ↑ Muscular dystrophy. Wikimedia. Available from: https://commons.wikimedia.org/wiki/File:MuscularDystrophy.png (last accessed 21 April 2023).
- ↑ 5.0 5.1 5.2 Eskay K. Paediatric Conditions – Down Syndrome, Duchenne Muscular Dystrophy, Osteogenesis Imperfecta and Arthrogryposis Multiplex Congenita Course. Plus, 2023.
- ↑ 6.0 6.1 Salari N, Fatahi B, Valipour E, Kazeminia M, Fatahian R, Kiaei A, Shohaimi S, Mohammadi M. Global prevalence of Duchenne and Becker muscular dystrophy: A systematic review and meta-analysis. Journal of orthopaedic surgery and research. 2022 Dec;17(1):1-2.
- ↑ Physiospot. Exercise for Muscular Dystrophy | Apply Caution| Article of The Week #20.December 14, 2020 by Scott Buxton
- ↑ 8.0 8.1 8.2 Gianola S, Castellini G, Pecoraro V, Monticone M, Banfi G, Moja L. Effect of muscular exercise on patients with muscular dystrophy: a systematic review and meta-analysis of the literature. Frontiers in neurology. 2020:958.
- ↑ Kidd A, Turnpenny P, Kelly K, Clark C, Church W, Hutchinson C et al. Ascertainment of myotonic dystrophy through cataract by selective screening. J Med Genet. 1995; 32:519–23.
- ↑ Kang MJ, Yim HB, Hwang HB. Two cases of myotonic dystrophy manifesting various ophthalmic findings with genetic evaluation. Indian J Ophthalmol. 2016; 64(7):535-7.