Oxygen Therapy
Original Editor - Uchechukwu Chukwuemeka
Top Contributors - Uchechukwu Chukwuemeka, Kim Jackson, Joseph Ayotunde Aderonmu, Rachael Lowe, George Prudden, Laura Ritchie, Karen Wilson, Claire Knott, Lucinda hampton and Carina Therese Magtibay
Description[edit | edit source]
Oxygen therapy has been in use for centuries. Oxygen)(O2) is gas used as a drug/medication and a such should be prescribed and administered in the right manner with regards to presenting indications for it's use[1]; which is always in the case of hypoxaemia[2]. It has side effects and specific risks, but, with objective monitoring and administration, it is a potent therapy for the patient with respiratory condition[3]. Oxygen is an expensive medication; thus, it's indication must be met before use.
Indications For Oxygen Therapy[edit | edit source]
Oxygen is rarely indicated for any other reason than Hypoxaemia[4].
- Hypoxaemia: Oxygen can be given in high or low concentration in all the conditions associated with hypoxaemia. Hypoxaemia occurs frequently in diseases like lower respiratory tract infection (severe pneumonia or bronchiolitis), upper airway obstruction, severe asthma, common neonatal conditions like birth asphyxia and in respiratory distress syndrome, severe sepsis, heart failure, cardiac arrest, trauma, carbon monoxide poisoning, and obstetric and perioperative emergencies.
Other indications include:
- Increased work of breathing
- Increased myocardial work and/or Myocardial infarction
- Pre-oxygenation in induction and difficult intubation.
- Pre and post suctioning[6]
- Postoperative oxygenation especially in abdominal and chest surgeries[7]
- Hyperbaric oxygen therapy indicated in decompression sickness, gas embolism, gas gangrene and carbon monoxide poisoning.
- Anaemic Hypoxia : it’s benefits is limited due circulatory deficit[8].
- In aerosol drug delivery.
Risks Of Oxygen Therapy[edit | edit source]
1. Depression of ventilation:
It is seen in COPD patients with chronic carbondioxide (CO2)retention who have hypoxic respiratory drive to breath[9]. Increased arterial tension to normal can lose the hypercapnoeic stimulus to maintain ventilation resulting in hypoventilation in these patients[10].
2. Hyperbaric oxygen toxicity:
Long term hyperbaric O2 therapy can lead to pulmonary, optic and central nervous system toxicity[11].
3. Fire hazard:
Oxygen enhance combustion of other fuels. Least level of supplemental oxygen (FiO2 greater than the 21% oxygen in ambient air) should be administratered during laser bronchoscopy to avoid intratracheal ignition[12].
4. Absorption atelectasis:
Given only pure oxygen results in the collapse of the dependent part of the lungs as it quickly taken up from the alveoli. It is also a risk in general anaesthesia induction[7]
5. Retinopathy of prematurity (ROP):
It usually occur in low birth weight, very premature infant. That is why in preterm infants, 50-80 mmHg PaO2 is recommended in infants receiving oxygen[13]
6. Bacterial contamination associated with certain nebulization and humidification systems is a possible hazard[14].
7. Oxygen therapy is contrindicated in patients suffering from paraquat poisoning[15]
8. Pulmonary toxicity:
Patients exposed to high oxygen levels for a prolonged period of time have lung damage[16]. The extent of lung damage is dependent on FiO2 and duration of exposure. It is due to intracellular free radicals (such as superoxide, activated hydroxyl ions, singlet O2 and hydrogen peroxide) formed which can damage alveolar-capillary membrane. It starts with increased permeability of the capillaries with resultant edema, thickened membranes and finally to pulmonary fibrosis.
Care should be taken in the use of oxygen in patients receiving bleomycin or have previously used bleomycin [17].
Precaution for physiotherapy in the use of supplemental oxygen[edit | edit source]
- The use of supplemental oxygen carries important implications for physical therapy in all clinical settings. It is important for the physiotherapist to know that:
- A patient using oxygen at rest, will definitely require it during exertion and all rehabilitation activities.
- The additional demands of rehabilitation activities may cause oxygen desaturation; so, signs and symptoms of hypoxemia should be known by the Physiotherapist
- Patients with a history of lung disease, especially those with a forced expiratory volume in the first second (FEV1) less than 50% or a diffusing capacity for carbon monoxide (DLCO) less than 60% of the predicted normal value, are likely to exhibit oxygen desaturation during exertion and should have their oxygenation status monitored.
- A drop in oxygen saturation to less than 86% to 90% during activity indicates that the patient needs supplemental oxygen; an order to institute oxygen therapy or to increase the oxygen dose during exertion should be requested from the physician.
- Home physical therapists should be aware of the oxygen therapy prescription for their patients and ensure that they are using their oxygen as prescribed.
Delivery Devices for Oxygen Therapy[edit | edit source]
The oxygen delivery devices are grouped into two:
Low flow oxygen delivery system
High flow oxygen delivery system
Low flow oxygen delivery systems are those that the exact fraction of oxygen in the inspired air (FiO2) will be based on the patient's anatomic reservoir and minute ventilation. They are:
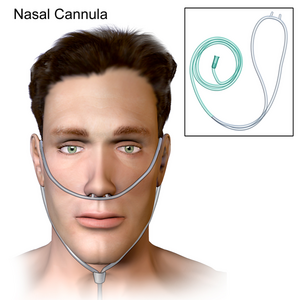
- Nasal Cannula: It can carry upto 1 – 6Litres of O2 Per Minute with FiO2 0.24 – 0.44 (approximate 4% per liter flow)[4] and FiO2 decreases as Ventilation rate increases. It is the recommended device for oxygen delivery in children less than 5years of age (level 1 evidence)[18]. It is ideal for long term oxygen therapy. It does not increase dead space and there is no rebreathing[19]
- Simple Mask: It can carry upto 5 – 10Litres of O2 per Minute with FIO2 0.35 – 0.55 (approximate flowrate of 40%). Flowrates should be set at 5 L/min or more to avoid rebreathing expired CO2 retained in the mask[18]. It slightly increases dead space and there is little rebreathing[19]. It is usually uncomfortable for patients, obstruct eating and drinking and also, muffles speech.
- Partial Rebreather is a simple mask with a reservoir bag. Oxygen flow should always be supplied to maintain the reservior bag on inspiration thus avoiding reservoir bag deflation. At a flow of 6-10 L/min the system can provide 50-70% oxygen[19].
- Non-rebreather: The non-rebreathing mask is similar to the partial rebreathing mask except it has a series of one-way valves. One valve is placed between the bag and the mask to prevent exhaled air from returning to the bag. There should be a minimum flow of 10 L/min. The delivered FiO2 of this system is 7-10%[19].
High flow oxygen delivery systems[20] deliver a prescribed gas mixture (either high or low) at flow rates that exceed patient demand.
- Venturi Mask: the flowrate is at about FiO2 0.24 – 0.50 with variable LPM. Flow and corresponding FiO2 varies by manufacturer
- If air-entrainment masks is available it can be used to accurately deliver preset oxygen concentration to the trachea up to 40% but the inspiratory flowrates is usually inadequate for adults in respiratory distress[20].
- Aerosol masks, tracheostomy collars, T-tube adapters, and face tents can be used with high-flow supplemental oxygen systems but not all aerosol generators can deliver high oxygen concentration at the needed flows rate[4][20].
Oxygen Storage and Source[edit | edit source]
Vacuum insulated evaporator (VIE):
When a gas becomes liquid form, it occupies a much smaller volume. Therefore, a large amount of oxygen can be stored in the form of liquid. A VIE is a container designed to store liquid oxygen. The VIE system is used in large hospitals which have a pipeline system. It is the most economical way to store and supply oxygen.[19][20][4]
Oxygen cylinders: It is expensive, cumbersome, and often unreliable. It usually serve as a backup in large hospitals and used mainly in out of hospital settings.
Oxygen concentrators: It draws air from the atmosphere and extracts nitrogen leaving upto 90-96% concentration of oxygen using zeolite molecular sieve. It is safe, reliable, and cost efficient source of oxygen, and more convenient than oxygen cylinder. It is important to have a backup source of oxygen(Oxygen cylinder), as it needs continuous power source and regular maintenance.
Central piped oxygen: oxygen is distributed via copper pipes circulating from a central source, that is situated outside the building. The source may be liquid oxygen, high-pressure gaseous oxygen cylinders, a large oxygen concentrator or a combination. It has the advantage of reduced risk of fire and obviates handling and transporting heavy cylinders between hospital wards. The high installment and maintenance cost is it’s daunting factor.
Resources[edit | edit source]
References[edit | edit source]
- ↑ Olive S. Practical procedures: oxygen therapy. Nursing times. 2016 Jan 1;112(1-2):12-4.
- ↑ Weekley MS, Bland LE. Oxygen administration. StatPearls [Internet]. 2021 Apr 28.
- ↑ Walsh BK, Smallwood CD. Pediatric oxygen therapy: a review and update. Respiratory care. 2017 Jun 1;62(6):645-61.
- ↑ 4.0 4.1 4.2 4.3 Hough A. Physiotherapy in Respiratory Care; An evidence-based approach to respiratory and cardiac management. 3rd eds. United Kingdom: Nelson Thomes Ltd, 2001 p.208
- ↑ Bazan IS, Fares WH. Pulmonary hypertension: diagnostic and therapeutic challenges. Therapeutics and Clinical Risk Management, 2015; 11: 1221–1233. Doi: 10.2147/TCRM.S74881
- ↑ Pritchard MA, Flenady V, Woodgate P. Systematic review of the role of pre-oxygenation for tracheal suctioning in ventilated newborn infants. Journal of Paediatrics and Child Health, 2003; 39(3):163-5
- ↑ 7.0 7.1 Hedenstierna G, Rothen HU. Atelectasis formation during anesthesia: causes and measures to prevent it. Jornal of clinical medicine and computing, 2000; 16(5-6):329-35.
- ↑ Van Meter KW. The effect of hyperbaric oxygen on severe anemia. Undersea and Hyperbaric Medicine, 2012; 39(5):937-42.
- ↑ Kim V, Benditt JO, Wise RA, Sharafkhaneh A. Oxygen therapy in chronic obstructive pulmonary disease. Proceedings of the American Thoracic Society, 2008; 5(4):513-8. Doi: 10.1513/pats.200708-124ET.
- ↑ Ergan B, Nava S. Long-Term Oxygen Therapy in COPD Patients Who Do Not Meet the Actual Recommendations. COPD, 2017;14(3):351-366. doi: 10.1080/15412555.2017.1319918.
- ↑ Heyboer M, Sharma D, Santiago W, McCulloch N. Hyperbaric Oxygen Therapy: Side Effects Defined and Quantified. Advances in Wound Care, 2017; 6(6): 210–224.
- ↑ Millette BH, Athanassoglou V, Patel A. High flow nasal oxygen therapy in adult anaesthesia. Trends in Anaesthesia and Critical Care, 2018; 18: 29-33
- ↑ Saugstad OD. Oxygenation of the Immature Infant: A Commentary and Recommendations for Oxygen Saturation Targets and Alarm Limits. Neonatology, 2018;114:69–75.DOI: 10.1159/000486751
- ↑ La Fauci V, Costa GB, Facciolà A, Conti A, Riso R, Squeri R. Humidifiers for oxygen therapy: what risk for reusable and disposable devices? Journal of Preventive Medicine and Hygiene, 2017; 58: E161-E165
- ↑ Gawarammana IB, Buckley NA. Medical management of paraquat ingestion. British Journal of clinical pharmacology, 2011; 72(5): 745–757. doi: 10.1111/j.1365-2125.2011.04026.x
- ↑ Mach WJ, Thimmesch AR, Pierce JT, Pierce JD. Consequences of Hyperoxia and the Toxicity of Oxygen in the Lung. Nursing Research and Practice, 2011. http://dx.doi.org/10.1155/2011/260482
- ↑ Debnath J. Supplemental oxygen therapy in bleomycin-induced pulmonary toxicity: REPLY. Medical Journal, Armed forces India, 2011; 67(2): 194–195. doi: 10.1016/S0377-1237(11)60037-3
- ↑ 18.0 18.1 World Health Organisation. Oxygen therapy for children: a manual for health workers. 2016. ISBN 978 92 4 154955 4
- ↑ 19.0 19.1 19.2 19.3 19.4 Htun AT, Thein WM. Oxygen Therapy. International Journal of Novel Research in Healthcare and Nursing, 2016; 3(2):8-14
- ↑ 20.0 20.1 20.2 20.3 Hillegass E. Essentials of Cardiopulmonary Physical Therapy. 3rd ed. Saunders, an imprint of Elsevier Inc. Missouri. 2011.