Thoracic Hyperkyphosis
Original Editors - Bo Hellinckx, Matthias Steenwerckx, Fien Selderslaghs, Mirabella Smolders and Wout Theys
Top Contributors - Lucinda hampton, Bo Hellinckx, Kim Jackson and WikiSysopDefinition/Description[edit | edit source]
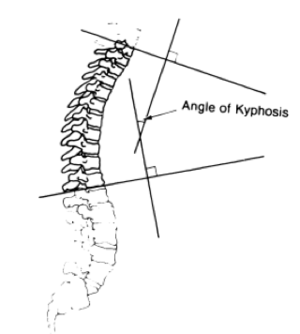
Thoracic hyperkyphosis is described as an excessive antero-posterior curvature of the thoracic spine of greater than 40°.[1]
- Angle increases with age, no uniform accepted thresholds for defining either hyperkyphosis or “normal” thoracic spine changes associated with aging[2]
- More common in females than males
Normal kyphosis angles vary between
- 20° and 40° in the younger public
- 48° to 50° in women and about 44° in men.[2]in older populations
Categories include
- Scheuermann’s Disease[3]: Juvenile form of hyperkyphosis. Defect of the vertebral body growth plate at the cortical level, resulting in weakened vertebral body and causing wedging. Stops at the end of growth (growth cartilage is no longer active).
- Postural Kyphosis[3]: Most frequent form, no vertebrae deformities visible. Result of poor posture, weakened muscles and ligaments of the spine.
- Congenital Kyphosis[3]: Bone defect detected at birth. Kyphosis angle will increase if not treated in time.
- Age-related Hyperkyphosis[4][5]: Kyphosis angle increases with age, resulting in age-related hyperkyphosis. Despite the fact that increased kyphosis is one of the typical results of osteoporosis, up to 70% of patients with age-related hyperkyphosis do not suffer from decreased bone mineral density.[4] The exact prevalence of patients for non-osteoporotic hyperkyphosis is unknown, yet it is estimated that 10% to 45% of the people aged over 50 years are properly diagnosed. Genderwise, thoracic hyperkyphosis increases to 50% in men and 65% in women over the age of 65 years.[6]
Clinically Relevant Anatomy[edit | edit source]
The thoracic part of the spine natural kyphosis. This thoracic curvature is the result of a slight wedging of the vertebrae.
- Normal degree of thoracic convexity (20-40degrees) is measured in the sagittal plane.[1][7]
- Thoracic hyperkyphosis is a defect that is easy to see from the side (lateral view), occurs when the thoracic flexion curve is over 40°.[8]
Line of Gravity
- In standing postures, the gravity line passes ventral to the vertebral bodies.
- The load of the gravity will increase the thoracic kyphosis.
- Bending forces bring anatomical changes.
- Anatomical changes include - passive constraint of the posterior ligaments; contraction of the deep one-joint muscles and thoracic parts of the long extensors.[9]
Epidemiology /Etiology[edit | edit source]
There is no widely accepted definition of hyperkyphosis therefore the prevalence of hyperkyphosis is not precisely known.
- The prevalence of hyperkyphosis increases with age in women and men, with the greatest change in the angle of kyphosis occurring among women age 50 to 59 years.
- Estimates range between 20 and 40 percent among community-dwelling individuals aged ≥60 years.
- Studies have reported kyphosis increases by about 9 degrees per decade[6].
- Level of kyphosis increases with age.[1] Often after the age of 40.[10]
- Difference in gender, namely, hyperkyphosis appears commonly more rapidly in women than in men.[1][10]
- Risk factors also for evolution of thoracic hyperkyphosis include musculoskeletal, neuromuscular and sensory impairments
- Some people have an idiopathic cause.[5][11][12]
- Psychosocial factors play a role ie Depression, Anxiety, Insecurity, Despondency. [1][13]:
Biomechanical Factors in thoracic hyperkyphosis
- Higher spinal loads and trunk muscle force in an upright stance. Accelerate the degenerative process and contribute to dysfunction and pain.[13]
- Daily activities with poor posture eg protruding head positions and loss of shoulder range induced by: slouched sitting; ill-fitting school desks; overloaded backs, and backpacks. [14]
Characteristics/Clinical Presentation[edit | edit source]
Hyperkyphosis of the thoracic spine can be postural or structural. Patients may also present with a combination of both alignment impairments.
1. Postural impairments are flexible and respond to positional changes or cues to change alignment.[7]
2. Structural alignment impairments ie fixed alignments of the bony structures persists regardless of the position of the individual. eg Scheuermann’s disease
When there is a combination of structural and postural alignment impairments, postural correction may only be partially successful. Kyphosis that started as a postural fault may become a structural impairment (commonly is not painful until a severe thoracic kyphosis has developed).[7]
- Most prominent symptom appearance of a rounded back (an exaggerated anterior curvature of the thoracic spine).[5]
- Change in back posture is mostly gradual over time.[15][16]
- Thoracic back pain
- Respiratory compromise.Thoracic hyperkyphosis could have detrimental effects on breathing.[9][17]
- Restricted spinal range of motion
- Osteoporotic fractures.[18]
- Having difficulty getting up from a chair, out of bed, or out of the bathtub
- Walking more slowly
- Feeling "off-balance," and/or losing your balance, or almost falling
- Feeling more tired than usual (fatigue)
- Having difficulty breathing (in more severe cases)[15]
Differential Diagnosis[edit | edit source]
The diagnosis of thoracic hyperkyphosis can be established by clinical examination and can be confirmed by radiologic imaging. Some individuals may develop the same magnitude of hyperkyphosis from different processes, which leads to a common misinterpretation[5]. Some differential diagnosis can be:[5][19]
- Scheuermann’s disease
- Osteoporosis
- Trauma-related spinal changes eg vertebral fracture
- Tumor
- Infection
- Degenerative disc disease
Diagnostic Procedures[edit | edit source]
Starting point of any diagnostic investigation of the thoracic spine - Plain radiography. Anteroposterior and lateral radiographs are always required.[20] [21]
- Anteroposterior radiographs come in very handy for the evaluation of the vertebral bodies, while the lateral radiographs are more helpful in assessing vertebral body height, disk height, endplate irregularity, erosions, and alignment.[20]
- If further investigation needed - Reformatted CT scans and MR images to display the overall curvature of the spine and give clear image of whether there is a kyphosis or not.[21]
Outcome Measures[edit | edit source]
The Visual Analogue Scale is a measurement instrument that measures the intensity of various symptoms (e.g. the amount of pain).[22]
The Quebec Back Pain Disability Scale is a self-administered measurement to evaluate the level of functional disability in individuals with back pain.[23]
Examination[edit | edit source]
Typical signs of age-related hyperkyphosis are:[4]
- Pain and dysfunction of both spine and shoulder[13]
- Loss of range of movement and increased stiffness
- Reduced physical function[24]
- Respiratory compromise
- Increased risk of osteoporotic fracture[25]
- Increased mortality rates in the elderly.
Begins with observing the patient eg abnormalities during gait and undressing can be noticed very quickly.[16]
- Examined in sagittal plane in standing and relaxed position “in order to assess the most affected somatic areas and posture alterations.”
The standing position of the clinical examination needs to be reproducible. - Ankles and toes are placed in a neutral anatomical posture.
- The lower limbs are stretched straight limiting an excessive recurvatum.
- The trunk and upper limbs are relaxed, palms of the hands on the lateral thighs, the eye is looking horizontally”.[3][16]
- Tragus to wall test can be used
When the angle is between 40-45° we consider it as a thoracal hyperkyphosis.
Equipment to measure the thoracic kyphosis angles.
These are:
- Modified Cobb Angle
- The pantograph
- The Debrunner kyphometer: Arms of the kyphometer are placed on C7 and T12, we read the angle from the protractor
- The flexicurve index: Place a marker on C7 and the lumbar-sacral joint space. Then use a flexicurve carefully and place it between C7 and the L-S joint space. When you take the flexicurve away from the back it will conserve the form of the whole back. Then put the flexicurve on a 10x10 paper and draw a vertical line and then the TW and LW lines you need to measure
Functional examination eg eventual rib cage abnormalities such as pectus excavatum or carnatum;
Medical Management[edit | edit source]
Physical management should be considered as a first-line approach. [5]
In terms of medications, antiresorptive or bone-building medications are taken by patients with thoracic hyperkyphosis due to their low bone density or spine fractures. Osteoporosis treatment helps to prevent incident spine fractures, however, no medications have been shown to improve hyperkyphosis.”[5]
There are multiple surgical procedures that can be applied, depending on:
- Flexibility: X-rays will be taken to determine how flexible the spine is. If it’s flexible, a posterior approach may be adequate. If the patient is less flexible, an anterior or combined approach will be needed. These techniques are based on bone fusion with screws and rods.[26]
- The surgeon can also choose for an osteotomy (a surgical operation in which a bone is cut to shorten, lengthen, or change its alignment.). An osteotomy often gives some good results on patients.
- Osteoporosis: An osteoporotic thoracic hyperkyphosis can be caused by a collapsed vertebra. This can be treated with a kyphoplasty, whereby a balloon is inserted into the affected vertebra and filled with liquid that hardens to restore the vertebral height.
Surgical interventions for painful vertebral fractures include vertebroplasty and kyphoplasty ( minimally invasive, gaining their wider acceptance.[5] They even have resulted in a decreased kyphosis angle. reduced pain, improved physical function, vertebral height restoration of up to 90%, and kyphosis angle correction ranging from 8.5° to 14°. Studies are limited however.[2][26]
More invasive surgical interventions for hyperkyphosis are associated with high rates of intra- and perioperative complications (33%). These interventions are normally reserved for patients with documented curve progression, intractable pain, or neurologic compromise.[5]
Physiotherapy Management[edit | edit source]
Physiotherapy for thoracic hyperkyphosis, including manual therapy, taping and bracing, should be implemented in an early stage and is regularly a first-line treatment.[27] The main goal of any therapy for patients with thoracic hyperkyphosis is to reduce the excessive antero-posterior curvature as well as improve the physical function and decrease the pain. Recognition and treatment of hyperkyphosis could contribute to a reduced risk of falls, fractures, and functional limitations.[5]
- Thoracic joint mobilizations are required in patients diagnosed with hyperkyphosis because of the reduced thoracic motion. eg.Scapular, myofascial and spinal mobilization techniques increase postural alignment i[5].
- Self-mobilization techniques e.g. diaphragmatic breathing on foam roller for expanding the rib cage. Additionally, these exercises can be performed at home when properly instructed.[5]
- Stretching. Below are a few stretching exercises with the intention of decreasing the tonus of the muscles involved:[5][28]
- Chest stretching on foam roller: lengthening pectoralis muscles
- Prone hip extension/ knee flexion: lengthening iliopsoas and rectus femoris
- Supine knee extension with hip at 90° flexion: lengthening hamstrings
- Thoracic correction exercises e.g. scapular posturing are effective for patients with thoracic hyperkyphosis. Main goal of these types of exercises correction of the thoracic position as well as improve the structural alignment and stiffness of the thorax.[29][30]
- Pain management using modalities such as heat, ice, and/or electrical stimulation such as transcutaneous electrical nerve stimulation (TENS).Muscle strengthening. Below there are a few examples of muscle strengthening:[5]
- Prone trunk lift to neutral: strengthening spinal extensors, middle- and lower trapezius
- Prone trunk lift to neutral with weighted backpack: strengthening spinal extensors
- Quadruped alternate arm/leg lift: strengthening spinal extensors, scapula and trunk stabilization, reducing anterior tightness
- Breathing exercises to help improve tolerance for physical activity by increasing lung capacity. eg. Diaphragmatic Breathing Exercises
Balance exercises and gait training to increase general fitness and reduce risk of falls This can often be part of an exercise program eg.Pilates
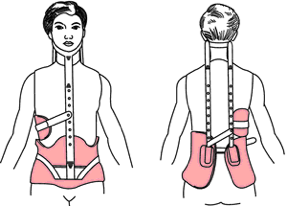
Bracing
Only recommended when the hyperkyphosis is no longer reversible through exercises because it is too stiff or because exercises have already proved insufficient.[16]
Passive bracing without the addition of physical therapy, doesn’t have any effect on the thoracic spine.[27][5][16]
A few types of bracing for thoracic hyperkyphosis are mentioned below:
- A Milwaukee Brace is the most common brace used by patients with a thoracic hyperkyphosis. This brace has posterior pads pushing anteriorly on the kyphosis. The neck and the pelvis are controlled by the other segments of the brace. The patients should wear this brace 23 hours a day for 1-2 years.[16]
- The results of the Lyon Antikyphosis Brace were very satisfactory in most patients with thoracic hyperkyphosis.[27]
- Also a new bracing design called the Kyphologic Brace has been shown to have a good in-brace correction on average.[33]
- Another kind of brace using the two 3-point pressure system is the ‘Gschwend type’ brace. This brace is mostly used in Germany.[28]
Taping
May also reduce kyphosis. Tape from the anterior aspect of the acromioclavicular joint, over the muscle bulk of the upper trapezius, and diagonally over the spinous process of T6. Further investigation is necessary.[5]
Spinal Orthosis
A SpinoMed is a spinal orthosis which can be used for a thoracic hyperkyphosis. There is some evidence found about the use of this device. The patient should wear this for 2 hours a day during 6 months. This will result in a decrease in kyphosis angle, an improvement of standing height, an increase in spinal extensor strength and a decreased postural sway.[5]
Conclusion[edit | edit source]
According to international studies. the conservative treatment for patients with thoracic hyperkyphosis is regarded as being effective.[28]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Fon GT, Pitt MJ, Thies Jr AC. Thoracic kyphosis: range in normal subjects. American Journal of Roentgenology. 1980 May 1;134(5):979-83.
- ↑ 2.0 2.1 2.2 Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Annals of internal medicine. 2007 Sep 4;147(5):330-8.
- ↑ 3.0 3.1 3.2 3.3 de Mauroy JC. Kyphosis physiotherapy from childhood to old age. InPhysical Therapy Perspectives in the 21st Century-Challenges and Possibilities 2012 Apr 5. IntechOpen.
- ↑ 4.0 4.1 4.2 Perriman DM, Scarvell JM, Hughes AR, Lueck CJ, Dear KB, Smith PN. Thoracic hyperkyphosis: a survey of Australian physiotherapists. Physiotherapy Research International. 2012 Sep;17(3):167-78.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 Katzman WB, Wanek L, Shepherd JA, Sellmeyer DE. Age-related hyperkyphosis: its causes, consequences, and management. journal of orthopaedic & sports physical therapy. 2010 Jun;40(6):352-60.
- ↑ 6.0 6.1 Bartynski WS, Heller MT, Grahovac SZ, Rothfus WE, Kurs-Lasky M. Severe thoracic kyphosis in the older patient in the absence of vertebral fracture: association of extreme curve with age. American journal of neuroradiology. 2005 Sep 1;26(8):2077-85.
- ↑ 7.0 7.1 7.2 Sahrmann S. Movement system impairment syndromes of the extremities, cervical and thoracic spines-e-book. Elsevier Health Sciences; 2010 Nov 19.
- ↑ Ackland TR, Elliott B, Bloomfield J. Applied anatomy and biomechanics in sport. Human Kinetics; 2009.
- ↑ 9.0 9.1 Edmondston SJ, Singer KP. Thoracic spine: anatomical and biomechanical considerations for manual therapy. Manual therapy. 1997 Aug 1;2(3):132-43.
- ↑ 10.0 10.1 Nishiwaki Y, Kikuchi Y, Araya K, Okamoto M, Miyaguchi S, Yoshioka N, Shimada N, Nakashima H, Uemura T, Omae K, Takebayashi T. Association of thoracic kyphosis with subjective poor health, functional activity and blood pressure in the community-dwelling elderly. Environmental health and preventive medicine. 2007;12(6):246-50.
- ↑ Negrini S, Aulisa AG, Aulisa L, Circo AB, de Mauroy JC, Durmala J, Grivas TB, Knott P, Kotwicki T, Maruyama T, Minozzi S. 2011 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis. 2012 Dec;7(1):3.
- ↑ Ashton-Miller JA. Thoracic hyperkyphosis in the young athlete: a review of the biomechanical issues. Current sports medicine reports. 2004 Jan 1;3(1):47-52.
- ↑ 13.0 13.1 13.2 Lewis JS, Valentine RE. Clinical measurement of the thoracic kyphosis. A study of the intra-rater reliability in subjects with and without shoulder pain. BMC musculoskeletal disorders. 2010 Dec;11(1):39.
- ↑ Britnell SJ, Cole JV, Isherwood L, Stan MM, Britnell N, Burgi S, Candido G, Watson L. Postural health in women: the role of physiotherapy. Journal of obstetrics and gynaecology Canada. 2005 May 1;27(5):493-500.
- ↑ 15.0 15.1 Zane MK. Physical Therapist’s Guide to Hyperkyphosis (Humpback) in Adults. American Physical Therapy Association. 2014;188.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 Zaina F, Atanasio S, Ferraro C, Fusco C, Negrini A, Romano M, Negrini S. Review of rehabilitation and orthopedic conservative approach to sagittal plane diseases during growth: hyperkyphosis, junctional kyphosis, and Scheuermann disease. Eur J Phys Rehabil Med. 2009 Dec 1;45(4):595-603.
- ↑ Culham EG, Jimenez HA, King CE. Thoracic kyphosis, rib mobility, and lung volumes in normal women and women with osteoporosis. Spine. 1994 Jun;19(11):1250-5.
- ↑ Greendale GA, Nili NS, Huang MH, Seeger L, Karlamangla AS. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the standing radiological Cobb angle. Osteoporosis international. 2011 Jun 1;22(6):1897-905.
- ↑ D'Antoni AV, Terzulli SL. Federico di Montefeltro's hyperkyphosis: a visual-historical case report. Journal of medical case reports. 2008 Dec;2(1):11.
- ↑ 20.0 20.1 El-Khoury GY, Whitten CG. Trauma to the upper thoracic spine: anatomy, biomechanics, and unique imaging features. AJR. American journal of roentgenology. 1993 Jan;160(1):95-102.
- ↑ 21.0 21.1 Naidich TP, Castillo M, Cha S, Raybaud C, Smirniotopoulos JG, Kollias S. Imaging of the Spine: Expert Radiology Series, Expert Consult-Online and Print. Elsevier Health Sciences; 2010 Aug 27.
- ↑ Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. The Journal of pain. 2003 Sep 1;4(7):407-14.
- ↑ Kopec JA, Esdaile JM, Abrahamowicz M, Abenhaim L, Wood-Dauphinee S, Lamping DL, Williams JI. The Quebec Back Pain Disability Scale. Measurement properties. Spine. 1995 Feb;20(3):341-52.
- ↑ Kado DM, Huang MH, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and poor physical functional ability in older community-dwelling men and women: the Rancho Bernardo study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2005 May 1;60(5):633-7.
- ↑ Huang MH, Barrett‐Connor E, Greendale GA, Kado DM. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. Journal of Bone and Mineral Research. 2006 Mar;21(3):419-23.
- ↑ 26.0 26.1 Lundine K, Turner P, Johnson M. Thoracic hyperkyphosis: assessment of the distal fusion level. Global spine journal. 2012 Jun;2(02):065-70.
- ↑ 27.0 27.1 27.2 de Mauroy JC, Vallèse P, Fender P, Lecante C. Historical Lyonaise brace treatment for adolescent hyperkyphosis. Results of 272 cases reviewed 2 years minimum after removal of the brace. Scoliosis. 2010 Sep;5(1):O69.
- ↑ 28.0 28.1 28.2 Weiss H, Turnbull D. Kyphosis (Physical and technical rehabilitation of patients with Scheuermann's disease and kyphosis). International encyclopedia of rehabilitation. 2010.
- ↑ 29.0 29.1 Jang HJ, Kim MJ, Kim SY. Effect of thorax correction exercises on flexed posture and chest function in older women with age-related hyperkyphosis. Journal of physical therapy science. 2015;27(4):1161-4.
- ↑ Wang MY, Greendale GA, Kazadi L, Salem GJ. Yoga improves upper-extremity function and scapular posturing in persons with hyperkyphosis. Journal of yoga & physical therapy. 2012 Jun 1;2(3):117.
- ↑ Greendale GA, Huang MH, Karlamangla AS, Seeger L, Crawford S. Yoga decreases kyphosis in senior women and men with adult‐onset hyperkyphosis: results of a randomized controlled trial. Journal of the American Geriatrics Society. 2009 Sep;57(9):1569-79.
- ↑ Kuo YL, Tully EA, Galea MP. Sagittal spinal posture after Pilates-based exercise in healthy older adults. Spine. 2009 May 1;34(10):1046-51.
- ↑ Weiss HR, Werkmann M, Bohr S. In-brace corrections in patients with kyphosis using the kyphologic® brace. Scoliosis. 2009 Dec 1;4(S2):O61.