Amputations
Original Editor - The Open Physio project.
Top Contributors - Niha Mulla, Cornelia Barth, Laura Ritchie, Admin, Rachael Lowe, Saeed Dokhnan, Adam Vallely Farrell, Tony Lowe, WikiSysop, Kim Jackson, Shaimaa Eldib, Lauren Lopez, Tarina van der Stockt and Sai Kripa
Definition[edit | edit source]
Amputation is defined as surgical removal or loss of body part such as arms or limbs in part or full. It is usually distinguished from disarticulation where a part is removed through a joint[1][2][3]
Prevalence[edit | edit source]
One million limb amputations are reported globally each year. And as of 2017, 57.7 million people across the globe have been living with traumatic amputation. Approximately 185,000 amputations occur in United States each year according to the amputee coalition. And also, as of April 2021, United states has over 2 million Americans living with amputation, and another 28 million at a risk of surgical amputation due to underlying causes.[3][4][5][6]
Data from Stanford Healthcare shows 49% rise in total number of amputations during the time of COVID-19 pandemic, during March 2020 to February 2021.[7][8]
Causes of Amputations[edit | edit source]
There are several conditions that can lead to amputation.[1] [2][3]
- Severe infection with extensive tissue damage
- Gangrene
- Trauma resulting from accident or injury, such as crush or blast wound
- Congenital/ Paediatric limb deficiency undergoing conversion amputation
- Congenital deformities of digits or limbs
- Congenital extra digits or limbs
- Necrosis or Necrotizing Fasciitis
- Cellulitis
- Peripheral Arterial Disease
- Frostbite
- Malignant/ cancerous tumor in bone or muscle of the limb e.g. Osteosarcoma
- Conditions that affect blood flow for example Diabetes [9]
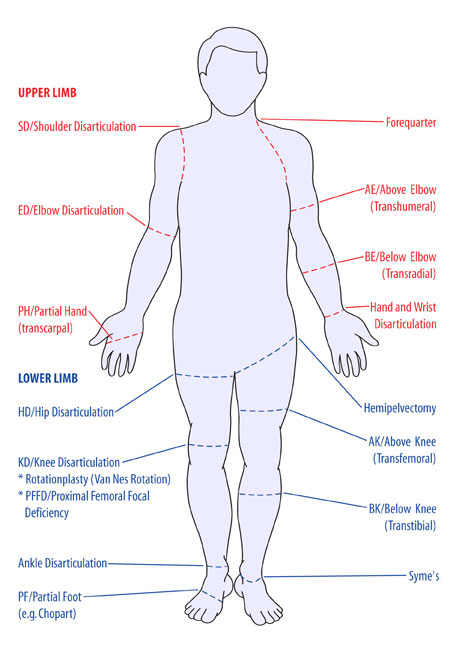
Levels of Amputation[edit | edit source]
Upper Limb [10][11][edit | edit source]
- Forequarter
- Shoulder Disarticulation (SD)
- Transhumeral (Above Elbow AE)
- Elbow Disarticulation (ED)
- Transradial (Below Elbow BE)
- Hand/ Wrist Disarticulation
- Transcarpal (Partial Hand PH)
- Transmetacarpal
Forequarter amputation- In this type of amputation, scapula, lateral 2/3rd of clavicle and whole of upper limb are removed.
Shoulder disarticulation- Removal through shoulder joint. Disarticulation is generally not so popular in the upper limb except at shoulder. Even in disarticulation of the shoulder, the head of humerus is preserved wherever possible to maintain the contour of the shoulder for cosmosis.
Above elbow amputation- Amputation above elbow through the arm.
Elbow disarticulation- Removal through elbow joint
Below elbow amputation- Amputation through the forearm bones
Wrist disarticulation- Amputation through radiocarpal joint
Ray amputation- Removal of a finger with respective metacarpal from carpo-metacarpal joint
Krukenburg's amputation- This is a below elbow amputation done usually on both sides. The forearm is split between radius and ulna. This can be used as a fork and it provides a pincer grip. Making 'forceps' with two forearm bones amputation
Lower Limb[10][11][edit | edit source]
- Hemicorporectomy
- Hemipelvectomy/ Hindquarter amputation
- Hip Disarticulation
- Short transfemoral(above knee)
- Transfemoral (above Knee)
- Long transfemoral (above knee)
- Knee Disarticulation
- Short transtibial (below knee)
- Transtibial (below knee)
- Long transtibial (below knee)
- Ankle Disarticulation (Symes)
- Tansmetatarsal
- Partial Foot/ray resection
- Toe disarticulation
- Partial Toe
Hind quarter amputation- In this amputation, part of the pelvis is removed along with lower extremity.
Hip disarticulation-Amputation through the hip joint
Above knee amputation- Amputation through the femur
Knee disarticulation- Amputation through the knee
Below knee amputation-Most commonly performed amputation, severe trauma to foot and leg. Amputation is performed through the leg bones
Syme’s amputation- Amputation through the ankle joint. Intact skin over the heel is attached back to the end of the stump with or without a part of calcaneum. Because of the intact heel, it becomes an end bearing stump and the patients generally manage very well walking even bare foot after this type of amputation
Chopart's amputation- Through talo-navicular joint amputation
Lisfranc's amputation- Through inter-tarsal joints amputation
Pre-Surgical Evaluation[edit | edit source]
- General system review- Cardiovascular & Respiratory[1]
- Nutritional status[1]
- Diabetes Control if appropriate
- Bowel & Bladder Function
- Past medical history
- Social history[1]
- Pre-morbid mobility[1]
- Strength & Condition of Healthy limb
- Psychological assessment to access emotion impact of amputation
- Home & work place assessment to make sure, everything is in accordance for patients maximal self reliance
- Explanation of post-operative regimen.[1]
Surgery for Amputation[edit | edit source]
Anesthesia is the first step to any surgery. During amputation, choice of anesthesia depends on the type of amputation, described above on levels of amputation. Two option of anesthesia for amputation are general anesthesia or epidural anesthesia.
While performing amputation, special care is to be taken to make sure the procedure does not hamper the functioning of remaining limb. It is vital to condition, shorten & smoothen the remaining bone, so there is a healthy stump that in future can take the load of a prosthetic limb and reduce complication risk.
Muscle is sutured to the bone at the distal residual bone so maximal strength of the remaining limb can be retained. This procedure is known as myodesis.
Distal stabilization of the muscles is always recommended, allowing for effective muscle contraction and reduced atrophy. This in turn allows for a greater functional use of the stump and maintains soft tissue coverage of the remnant bone. As the procedure for amputation is completed, the wound us sealed by performing myoplasty: suture to opposite muscle in the residual limb to to each other and to the periosteum or to the distal end of the cut bone for weight bearing purposes; and is covered with a bandage. A drainage tube might be placed to drain all excess fluid. Hence, every possible measure is taken to reduce risk of infection.[1]
Ideal Stump[edit | edit source]
- Skin flaps: skin should be mobile, sensation intact, no scars
- Muscles are divided 3 to 5 cm distal to the level of bone resection
- Nerves are gently pulled and cut cleanly, so that they retract well proximal to the bone level to reduce the complication of neuroma
Stump care[edit | edit source]
| [12] |
- For hygiene and skin care see handout on amputations
- A hip flexion contracture may develop because of elevation to reduce swelling
- Stump bandaging is done to ‘cone’ the stump, thereby preventing oedema, which occurs because there is no muscle pump and the stump hangs
- Swelling must be prevented to allow proper attachment of the prosthesis, and the prevention of pressure sores
- The stump sock is put on first, then the prosthesis
- The prosthesis must be cleaned and maintained (children who are still growing, grow out of their prostheses)
Complications of Amputation[edit | edit source]
- Edema & Swelling
- Wounds Infection
- Pain (phantom limb)
- Muscle weakness
- Muscle Tightness & contractures
- Joint Instability
- Autonomic dysfunction
- Somatosensory impairment[13]
See here, for more detailed information on post-operative complications following an amputation.
Post Surgical Evaluation[edit | edit source]
- General system review- Cardiovascular & Respiratory[11]
- Nutritional status
- Diabetes Control if appropriate
- Bowel & Bladder Function
- Strength & Condition of Healthy limb
- Psychological assessment to access emotion impact of amputation
- Signs of Infection
- Type of pain(Incisional, phantom, other)[11]
- Level of Pain(VAS 1 - 10)
- Functional status (Bed mobility, transfers, sitting, standing, walking, balance)[11]
- Strength and/or pain of the un-amputated limb
Post-operative Care[edit | edit source]
- Maintain function in the remaining leg and stump to maintain peripheral circulation
- Maintain respiratory function (important with smokers and those patients under general anaesthesia)
- Prepare for mobility rehabilitation
Pain in Amputation[edit | edit source]
Residual Limb pain and phantom limb pain are the two essential types of pain, post amputation.[10]
Residual Limb Pain[edit | edit source]
Residual limb pain has three main cause:
- Very likely post operative pain
- Peripheral nerve neuroma formation at the end of cut peripheral nerve
- Prosthetic pain caused by ill fitting prosthesis
Phantom Limb Pain[edit | edit source]
Phantom limb pain is defined as "pain that is localized in the region of the removed body part." Cause of Phantom limb pain is not fully understood , but it is distressing and has a significant impact on patients life.
Psychological Implications of Amputation[edit | edit source]
- Loss of limb has a huge psychological impact on ones mental health, as if the person has lost a loved one. It is difficult to cope with loss of sensation and function from the amputated limb. It also changes your (patients) and other peoples perception of your (patients) body image, which can lead to depression and anxiety as negative thoughts are very common.
- Psychological well being of the patient is vital to a good rehabilitation process. Hence, it is the duty of a physiotherapist/ physical therapist to acknowledge patients concerns with good knowledge of natural grieving process.[1][2]
Fall Risk Post Amputation[edit | edit source]
- Patient undergone amputation is at a higher risk of fall especially when they try to get up from the bed or chair and they have forgotten about the absence of the limb. These falls can cause injury to the surgical site, leading to prolonged healing.[1]
- To deal with the risk of fall, it is mandatory to place a walker besides the patient. This reminds the patient to use assistance for transfers.
Goals of Post-operative Physiotherapy Management[edit | edit source]
- Patient education on amputation and rehabilitation post amputation.
- Maintenance of respiratory & cardiovascular status both pre- & post- surgery
- Proper positioning of amputated limb to maintain the limb in right anatomical position.[11]
- Maintaining/improving strength of unamputated limb
- Residual Limb care
- Balance training
- Transfer Training
- Mobility Training
- Prosthetic training
Post-operative Physiotherapy Management[edit | edit source]
- Start with respiratory maintenance with pain control for amputated limb. Also start strengthening the unamputated limb to maintain its strength.[10]
- Teach the patient to wrap the residual limb correctly.
- Prevent hip flexion contracture by avoiding prolonged sitting & guiding patient to spend more time in prone position.[11]
- For proper positioning avoid side lying position, maintain the residual limb in extension at hip & knee.
- Start balance training
- Procced to mobility training initially with a walker followed by crutches.
- Start strengthening of the residual limb before proceeding to prosthetic training[10]
Pre- Prosthetic Evaluation[edit | edit source]
- Social History of patient
- Financial status
- Cause of amputation
- Cardiopulmonary status examination[11]
- Scar healing assessment
- Sensory assessment
- Residual limb length & shape
- Emotional status of patient for acceptance of amputation and body image
- Vascularity (pulse, color of limb, temperature, edema/swelling, pain & tropic changes[11]
- Range of motion
- Muscle strength
- Pain (residual & phantom)
- Functional status ( transfers, mobility, activities of daily living)
Please find below links to more detailed pages on the management of amputees
- Pain Management
- Pre-Fitting Management of the Patient with a Lower Limb Amputation
- Post-fitting Management
- Prosthetic Rehab
- High level Rehab
- Clinical Guidelines: Mental Health Amputees
More to do with patients with amputation[edit | edit source]
- Buerger's Exercises
| [14] |
- Stimulates collateral blood flow in the patient’s leg
- It is performed for 20 min.
- The leg is elevated until the toes go white, then lowered, then level
- Repeat 2-3 times to improve collateral circulation
2. Connective Tissue Massage
3. Dynamic Stump Exercises
4. Balance and Gait Retraining
- Improve static and dynamic balance
- Use parallel bars, walking frame then Crutches (in that order)
- Therapist stands on the amputation side, using a belt around the patient’s waist to support
- Rest if the patient feels tired
| [15] |
5. Short Wave Diathermy (SWD)
Through the pelvis to warm the arteries (contraindicated in patients with arterial insufficiency because the warmth leads to increased metabolism, causing a greater demand for nutrients, which are not available)
Walking Again Post Amputation/ Mobility Aids[edit | edit source]
- The choice of mobility aids depends on the level of fitness, strength, balance skills of the individual:
- For bilateral lower limb amputees a wheelchair is often indicated (high energy expenditure during gait with prostheses)
Prosthetic Training[edit | edit source]
Prosthetic training is vital for smooth and energy efficient living, while performing all of daily living activities.
Below is step by step guidance to prosthetic training:[11]
- Accepting weight of the body on each leg is vital to prosthetic training
- work on strengthening unamputated limb along with residual limb
- Teach the patient to balance on both legs and than on one leg
- Teach walking with prosthetic first with use of walker followed by crutches and stick
- Further proceed to independent prosthetic training.
- Teach the patient to adapt to environmental demands while walking
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Shores JT, M.D. Health and Amputation by John Hopkins Medicine. Available from: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/amputation
- ↑ 2.0 2.1 2.2 NHS choices. NHS on Amputation. 2019 August 12 Available from: https://www.nhs.uk/conditions/amputation/
- ↑ 3.0 3.1 3.2 Dunkin MA. Limb Amputation overview: Reasons, procedure, recovery. WebMD; 2020 February 05 Available from: https://www.webmd.com/a-to-z-guides/definition-amputation
- ↑ McDonald CL, Westcott-McCoy S, Weaver MR, Haagsma J, Kartin D. Global prevalence of traumatic non-fatal limb amputation. Prosthetics and orthotics international. 2020 Dec 4:0309364620972258
- ↑ 15 Limb Loss Statics by Access Prosthetics. 2017 October 18. Available from: https://accessprosthetics.com/15-limb-loss-statistics-may-surprise/#:~:text=There%20are%20more%20than%201,%2D%E2%80%94one%20every%2030%20seconds.
- ↑ Hanger Clinic blog: Limb Loss And Limb Difference: Facts, Statistics & Resources. Hanger Clinic. 2021 April 30 Available from: https://hangerclinic.com/blog/prosthetics/limb-loss-and-limb-difference-facts-statistics-resources/
- ↑ Cahan E. Unsalvageable: Preventable Amputations Rise During Covid-19. WebMD; 2021October 7 Available from: https://www.webmd.com/lung/news/20211007/preventable-amputations-rise-during-pandemic#:~:text=And%2C%20experts%20fear%2C%20with%20more,borne%20by%20patients%20of%20color
- ↑ Spector J. Studies Note Increase in Amputations after Arrival of Covid-19 Pandemic. Podiatry Today. 2020 Oct;33(10):10-1.
- ↑ Casciato DJ, Yancovitz S, Thompson J, Anderson S, Bischoff A, Ayres S, Barron I. Diabetes-related major and minor amputation risk increased during the COVID-19 pandemic. Journal of the American Podiatric Medical Association. 2023 Mar 1;113(2).
- ↑ 10.0 10.1 10.2 10.3 10.4 Stuart Porter. Tidy’s Physiotherapy, Chapter 22 “Physiotherapy for Amputees". 2003. Edition 13
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 11.8 11.9 O'Sullivan at.al, Physical Rehabilitation, Chapter 22 “Amputation”. Edition 6
- ↑ Richard Major. Physiotherapy Stump or Residual Limb Wrapping. Available from: http://www.youtube.com/watch?v=T1SA_6hzTxQ[last accessed 08/12/12]
- ↑ Petersen BA, Sparto PJ, Fisher LE. Clinical measures of balance and gait cannot differentiate somatosensory impairments in people with lower-limb amputation. Gait & posture. 2023 Jan 1;99:104-10.
- ↑ ladybessviernes, UDM PT Students. Buerger Allen's Exercise. Available from: http://www.youtube.com/watch?v=jQUFmOmX35o [last accessed 01/12/12]
- ↑ Clegstories. Clegstories. Gait Training with C-Leg®: Sitting Down and Standing Up. Available from: http://www.youtube.com/watch?v=_lBkrLZ4PGo [last accessed 08/12/12]