Pre-Fitting Management of the Patient with a Lower Limb Amputation
Original Editor - Liezel Wegner as part of the World Physiotherapy Network for Amputee Rehabilitation Project
Top Contributors - Sheik Abdul Khadir, Admin, Leslie Angama, Tarina van der Stockt, Lucy Aird, Kim Jackson, Tony Lowe, Simisola Ajeyalemi and Amrita Patro
Introduction[edit | edit source]
The loss of a lower limb has severe implications for a person’s mobility, and ability to perform activities of daily living [1]. This negatively impacts their participation and integration into society [2]. The ultimate goal of rehabilitation after limb loss is to ambulate successfully with the use of a prosthesis[3]. Prosthetic rehabilitation is a complex task that ideally requires input from an interdisciplinary rehabilitation team. However, most often physiotherapists are in charge of the physical rehabilitation process [4].
Overview of the Rehabilitation Process[edit | edit source]
The rehabilitation process of the lower limb amputee consists of nine phases[5] as shown in the table below (modified from Esquenazi &Meier[6]cited in Esquenazi[7]):
| Phase | Hallmark |
|---|---|
| Pre-operative | Assess body condition, patient education, surgical level discussion, postoperative prosthetic plans |
| Amputation Surgery/Reconstruction | Length, myoplastic closure, soft tissue coverage, nerve, handling, rigid dressing |
| Acute Post-surgical | Wound healing, pain control, proximal body motion, emotional support |
| Pre-prosthetic | Shaping, shrinking, increase muscle strength, restore patient locus of control |
| Prosthetic Prescription | Team consensus on prosthetic prescription and fabrication |
| Prosthetic Training | Increase prosthetic wearing and functional utilization |
| Community Integration | Resumption of roles in family and community activities. Emotional equilibrium and healthy coping strategies. Recreational activities |
| Vocational Rehabilitation | Assess and plan vocational activities for future. May need further education, training or job modification |
| Follow-up | Life-long prosthetic, functional, medical assessment and emotional support |
Pre-prosthetic Fitting Phase[edit | edit source]
The PRE-PROSTHETIC rehabilitation phase of the lower limb amputee will include six components:
- Physiotherapist preparation
- Assessment of the amputee (covered on a different page)
- Patient education
- Residuum management
- Exercise therapy
- Restoring locus of control
- Referral
Physiotherapist Preparation[edit | edit source]
As you approach an amputee, you should physically and mentally prepare for the interaction with the patient. Some questions to consider include:
- Who is my patient? (young/old)
- What was the cause of the amputation? (traumatic/dysvascular)
- Where (what level) was the amputation performed? (implications for rehabilitation outcome)
- What is the patient’s goal? (Is the patient aware of the possibilities, are they being realistic?)
- What prosthetic options are available for this particular patient? (self-study and preparation)
Awareness of Stages of Grief Process[edit | edit source]
A young patient who suffered an amputation as a result of a traumatic experience will most likely be in some stage of the grieving process and be in acute post-surgical pain. An older patient who suffered a dysvascular or neuropathic limb loss, might have had some time to psychologically and physically prepare for the loss of their limb[3]. Either way, your patient might be psychologically and physically distressed when you start the rehabilitation process, so early discussion and education about the patient’s expectations and goals are essential [8].
- Emotional and psychological reactions to amputation
- Reaction to amputation: Recognition and treatment
- Slideshow on grief amongst amputees
Knowledge of Appropriate Outcome Measures and Assessment Tools[edit | edit source]
Be prepared with the appropriate assessment tools and outcome measures to assess your patient’s potential for prosthetic use, and try not to create false hope (Outcome Measures for Patients with Lower Limb Amputations)
Knowledge of the Appropriate Assistive Technology Available[edit | edit source]
Your patient will look to you to provide early information about the possibilities for a prosthesis. Ensure that you have a basic knowledge and understanding of the prosthetic technology that is available and could be appropriate for your patient (Prosthetics).
Assessment of the Amputee[edit | edit source]
In order to formulate an appropriate patient-centred prosthetic rehabilitation plan for any amputee, the patient needs to be adequately assessed. Refer to Assessment of the amputee
Patient Education[edit | edit source]
Rehabilitation Process[edit | edit source]
Patient education should commence with a discussion regarding the rehabilitation process, and patient-centred goal setting[3]. The patient should be educated with regards to their potential options for assistive and prosthetic devices [9].
Pain Management[edit | edit source]
Managing the patient’s expectations with regards to the acute post-surgical pain they will potentially experience during the rehabilitation process will enhance patient cooperation and improve the rehabilitation outcome [3] [9].
Prevention of Complications[edit | edit source]
Education on limb care of both the residual and sound limbs are vital in preventing further complications, and the possibility of re-amputation[9]. Patients should be educated on diabetic foot care and advised to visually inspect the sound limb daily for any signs of redness[9].
Carer Education[edit | edit source]
The primary caregiver of the amputee should be involved from an early stage of the rehabilitation process and educated on all the rehabilitation techniques that are taught to the patient in order to improve patient compliance on discharge[9].
Residuum (Stump) Management[edit | edit source]
The following list of factors may directly influence the success of rehabilitation with a prosthesis, and should be evaluated and addressed during rehabilitation: the wound, oedema, scar from the incision, skin condition, length and shape of the residuum, tenderness, contracture of the proximal joint, the distal bone, dog ears, additional (redundant) tissue, other scars/factors[10].
Desensitisation of the Residuum, Scar Massage and Skin Care[edit | edit source]
Management of the surgical scar is also important when preparing the residual limb for prosthetic fitting. A scar that is hypersensitive or uneven can make weight-bearing on the residuum very painful or impossible. Once the surgical wound on the residual limb is adequately healed, the therapist should initiate a regime of desensitisation of the residuum in order to prepare the residuum for weight-bearing on a prosthesis and scar massage to prevent adhesions of the scar to bony prominences [3] [9] and teach the patient how to perform it themselves.
Shaping of the Residuum (bandaging)[edit | edit source]
See Acute post-surgical management of the amputee to read more about post-op dressings.
Shaping or coning of the residuum is a vital part of pre-prosthetic rehabilitation [3] [5] [9]. A residuum that is poorly shaped or bulbous in shape (distal circumference measured 5cm proximal to the end of the residuum is larger than the proximal circumference) cannot be fitted with a prosthesis, or greatly complicates prosthetic fitting (see figure below).
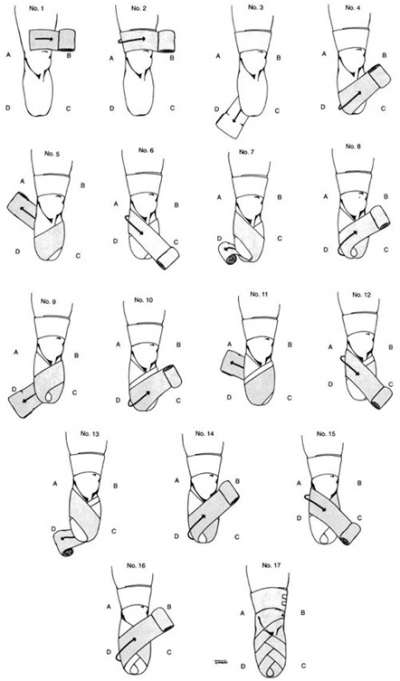
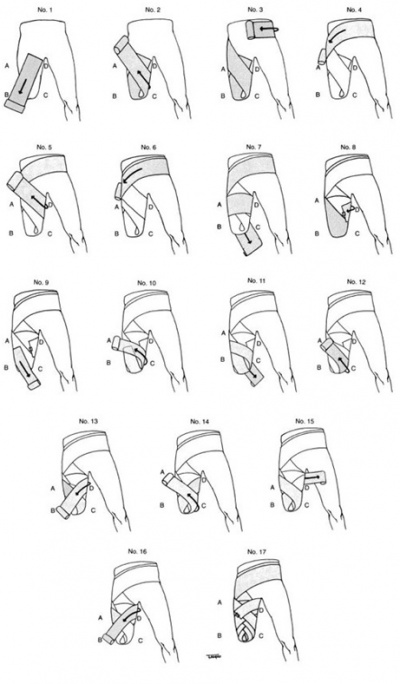
residuum bandaging or coning is essential in shaping the residuum. See the videos and diagrams below on how to perform residuum bandaging for a transtibial and transfemoral amputee.
Transtibial residuum Bandaging:[edit | edit source]
Transfemoral residuum Bandaging:[edit | edit source]
Post-op Silicone Liner[14][edit | edit source]
- it is applied after the Removable Rigid Dressing is taken off
- the same level of compression is applied to the residuum even if different people apply it
- it decreases oedema and shapes the residuum for prosthetic fitting
- helps with pain relief
- fast track the rehabilitation process
- It can be sterilised
- the liner size is prescribed according to the circumference of the residuum and can be changed when oedema decreases
- Disadvantages are: the cost involved, as the oedema goes down another size silicone liner needs to be applied, not readily available
Exercise Therapy[edit | edit source]
Exercise forms a large component of pre-prosthetic rehabilitation. The different elements of a pre-prosthetic exercise programme that should be included and tailored to the needs of the individual patient are listed below [9].
Basic Training and Skills[edit | edit source]
- Strengthening
- Range of Motion
- Functional Activities
- General Conditioning
- Bed Mobility
- Transfers
- Wheelchair Propulsion
- Unsupported Standing Balance
- Ambulation With Assistive Devices
Pre-gait Training[edit | edit source]
- Balance and Coordination
- Orientation to the Center of Gravity and Base of Support
- Gait-Training Skills
- Sound Limb and Prosthetic Limb Training
- Pelvic Motions
- Variations
- Immediate post-op prosthesis
- Balance standing on 2 limbs
- Pelvic motions
- Gait training
- Sit to stand
Exercise Videos[edit | edit source]
| Strengthening of residual limb with and without thera-band | Transfemoral amputation BOSU ball balance retraining |
Follow these links to YouTube playlists with exercise videos:
- Below knee amputee exercise video collection
- Above knee amputee exercise video collection
- Bilateral leg amputee exercise video collection
Restoring locus of control[edit | edit source]
Mobility with an assistive device/ wheelchair[edit | edit source]
Early post-operative mobilisation is imperative to prevent deconditioning after amputation surgery. Ideally, patients would be mobilised with an assistive device such as a walking frame or elbow crutches, but often this is quite challenging in patients with co-morbid diseases. The use of a pneumatic compression splint prosthesis is advised for patients with limited physical function and mobility [3]. This type of inflatable splint fits around the residual limb without putting pressure on the wound, and can be used to facilitate early mobilisation, and to assess the potential for prosthetic rehabilitation [3]. Another alternative for early mobilisation in high-risk patients is the application of an immediate postoperative prosthesis (IPOP) [3]. The non-removable rigid dressing used for an IPOP is applied by a Prosthetist in the theatre, and is shaped around the residual limb for patellar-tendon weight bearing to avoid pressure on the wound during early mobilisation [3]. Patients will have to be assessed in order to determine which assistive device is most appropriate for early mobilisation, and then taught how to mobilise safely with these devices.
Mobilising with crutches:
- Using elbow crutches with an amputation
- Using axillary crutches with an amputation
- Alternatives: Hands-free crutches
See this video below on how amputees can safely accommodate stairs with the use of crutches
Transfers[edit | edit source]
An important step in the rehabilitation process is regaining functional independence. The amputee should be taught how to safely and if possible independently transfer themselves between the following surfaces especially in the case of a double lower limb amputee, or a frail person.
- Bed to fixed chair
- Bed to wheelchair
- Wheelchair to bed
- Wheelchair to floor – if the patient has the muscle power to perform this
- Floor to wheelchair – if the patient has the muscle power to perform this
- Wheelchair to toilet
- Wheelchair to shower/bath
- Wheelchair to car
- Car to wheelchair
See the videos below on transfers involving lower limb amputees.
Referral[edit | edit source]
The physiotherapist should always remember that even though they might often manage the rehabilitation process of an amputee [5], pre-prosthetic rehabilitation is a multidisciplinary task [3] [5], and physiotherapists should not operate in isolation of other health care professionals. Some of the health care professionals and other resources that should form part of the MDT and could be referred to are listed below.[3] [5]
- Psychologist - counselling
- Nurse – specialist wound care
- Dietician – in the case of poorly controlled diabetes
- Physician –medical management of phantom pain
- Prosthetist – prosthetic prescription and management
- Occupational therapist – assessment and adaptation of the home environment
- Social services – potential disability grant / financial support
- Local or national amputation support group or disabled persons organisation for peer support
Useful resources[edit | edit source]
- Physical therapy management of adult lower limb amputees
- The Rehabilitation of People with Amputations
- VA/DoD clinical practice guideline for rehabilitation of lower limb amputation
- Exercise tick-sheet for transtibial amputation strengthening exercises
- Care of Your Wounds After Amputation Surgery - Amputee Coalition
- YouTube presentation: Transfemoral Strength and Balance Exercises
- Focus on IPOPs, EPOPs: Does Early Mobility Benefit Amputees?
- Improving Outcomes With Immediate Postoperative Prostheses
- Post-Op Prostheses offer Benefits After Amputation Surgery
- Below Knee Amputation – Surgery, Recovery and Maintaining Mobility
References[edit | edit source]
- ↑ Dillingham TD and Pezzin LE. Rehabilitation setting and associated mortality and medical stability among persons with amputations. Archives of Physical and Medical Rehabilitation 2008; 89; 1038-1045.
- ↑ World Health Organisation (WHO). International classification of functioning disability and health (ICF). World Health Organisation 2001. Geneva.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 Lusardi MM, Postoperative and preprosthetic care. In Lusardi, MM, Jorge, M and Nielsen, CC editors. Orthotics and Prosthetics in Rehabilitation, Third Edition. Missouri: Elsevier, 2013.p. 532-594.
- ↑ Kaplan SL, Outcome measurement and management: First steps for the practicing clinician. Philadelphia, FA Davis Company, 2007.
- ↑ 5.0 5.1 5.2 5.3 5.4 Esquenazi A. Amputation rehabilitation and prosthetic restoration: from surgery to community reintegration. Disability and Rehabilitation, 2004; 26,(14/15); 831–6.
- ↑ Esquenazi A, Meier RH. Rehabilitation in limb deficiency. 4. Limb amputation.Arch Phys Med Rehabil. 1996 Mar;77(3 Suppl):S18-28.
- ↑ Esquenazi A. Amputation rehabilitation and prosthetic restoration. From surgery to community reintegration. Disabil Rehabil. 2004 Jul 22-Aug 5;26(14-15):831-6.
- ↑ Livingstone W, Van de Mortel TF, Taylor B. A path of perpetual resilience: Exploring the experience of a diabetes related amputations through grounded theory. Contemporary Nursing. 2011; 39(1):20-30.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 Gaily RS, Clark CR.Physical therapy management of adult lower-limb amputees. In: Michael, JW editor. Atlas of Limb Prosthetics: Surgical, Prosthetic, and Rehabilitation Principles. Rosemont, IL, American Academy of Orthopedic Surgeons,1992. http://www.oandplibrary.org/alp/(accessed 8 February 2015).
- ↑ O'Keeffe B, Rout S. Prosthetic Rehabilitation in the Lower Limb. Indian Journal of Plastic Surgery. 2019 Jan;52(01):134-43.
- ↑ AmputeeOT: Massage, Scar Mobilization, Desensitization, and End-Bearing Exercises for New Amputees. Jan 2014. Available from: https://youtu.be/AqmKhuT-mWw
- ↑ Ottobock. Skin care after amputation. Jan 2019. Available from: https://youtu.be/15gsqIrz8Ps
- ↑ Ottobock. Scar care & scar mobilisation after amputation. Available from: https://youtu.be/-IMV8j21kLw
- ↑ Johannesson A, Larsson GU, Öberg T. From major amputation to prosthetic outcome: a prospective study of 190 patients in a defined population. Prosthetics and orthotics international. 2004 Jan 1;28(1):9-21. Available at: https://www.researchgate.net/publication/8534355_From_major_amputation_to_prosthetic_outcome_A_prospective_study_of_190_patients_in_a_defined_population[Accessed 11 Oct 2017]
- ↑ 15.0 15.1 15.2 15.3 International Committee of the Red Cross (ICRC), ICRC physiotherapy reference manual: prothetic gait analysis, 2014 Prosthetic gait analysis, a course manual for physiotherapists, ICRC, 2014. Available from: https://members.physio-pedia.com/open-ebooks/prosthetic-gait-analysis-for-physiotherapists/view.php?start=44 [Accessed 27 Dec 2017]
- ↑ AmputeeOT: Using crutches etc to get around after amputation . Available from: https://www.youtube.com/watch?v=lugS_AmY2BU&t=86s[last accessed 16/12/17]
- ↑ IPOP Immediate Postoperative Prosthesis. Available from: https://youtu.be/9voyLE_9IMU[last accessed 16/12/17]
- ↑ Double amputee transferring from wheelchair to floor . Available from: https://www.youtube.com/watch?v=1l5447Hhfxc[last accessed 16/12/17]
- ↑ AmputeeOT: Safe Showers and Baths for Amputees . Available from: https://www.youtube.com/watch?v=16qdl_25xmQ[last accessed 16/12/17]