Walking Aids
Original Editor - The Open Physio project.
Top Contributors - Admin, Lauren Lopez, Kim Jackson, Ammar Suhail, Redisha Jakibanjar, Lucinda hampton, Natalie Patterson, Tolulope Adeniji, Rachael Lowe, Naomi O'Reilly, WikiSysop, Karen Wilson and Amanda Ager
Introduction[edit | edit source]
Walking aids are sometimes also referred to as ambulatory assistive devices. A walking aid is one of several devices a patient may be issued in order to improve their walking pattern, balance or safety while mobilising independently. They can also be a means of transferring weight from the upper limb to the ground, in cases where reducing weight bearing through the lower limb is desired.
Walking aids fall into multiple categories and include the following:
- Canes or walking sticks (note - The distal tip of canes and crutches should have a rubber ferrule to prevent the walking aid from slipping, with some ferrules being depressed to form a vacuum when it comes into contact with the ground. The ferrule should not be worn or cracked and should fit well onto the point of the walking aid).
- Crutches
- Walkers
- Standing Aids: to assist with manual handling often used with in rehabilitation.
The video below gives a good introduction to the categories
[1]Prescription[edit | edit source]
Although often a solution to mobility issues, walking aids do come with their own mix of benefits and challenges to the individual using them. A 2005 study reported that these devices can improve balance and mobility but also can interfere with balance in certain situations, and the strength and metabolic demands can be excessive. They hoped for improved designs and guidelines for safer use of canes and walkers.[2]
Prescription of walking aids should ideally be done by a physiotherapist or occupational therapist after a thorough assessment of gait, balance, cognition and the cardiovascular, musculoskeletal and neurological systems. Assessment should also take into account any clinically significant co-morbidities[3] and the individual's day to day mobility requirements for example. thresholds in their home, community ambulation, navigating steps or public transport. Thought needs to be given to whether the walking aid is a temporary requirement for example post fracture or a more long-term option for example a walking frame for an elderly adult with reduced mobility post stroke.
Therapists should also be aware of the perceptions of walking aids can be negative at times as individuals may feel like they are giving up their independence or fear they will look frail[4]. In such instances, the Therapists needs to balance the individual's concerns with safety, encouraging the individual to consider the walking aid as keeping them mobile and able to participate in their activities of daily activities.
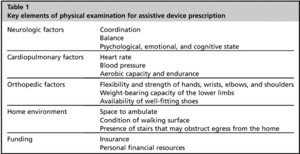
Furthermore, comprehensive system review of the patient such as the neurological factors, cardiopulmonary factors and musculoskeletal system is an important component of assessment in prescribing a assistive device.Follow up is also needed after an initial assessment and prescription in order to adjust the walking aid as needed. Although beneficial for stability and balance, walking aids can be difficult to use which is associated with falls[5]. See the canes, crutches and walkers pages for further detail.
Descriptors of Weight Bearing Status[edit | edit source]
Prescription of an appropriate walking aids requires knowledge of weight bearing prescribed to the patient or being allowed by the problem
present. Weight bearing status can be described using the following[6]:
- Full weight bearing (FWB): There are no restrictions and client can bear 100% body weight on the lower extremities (LE).
- Non-weight bearing (NWB): No weight is borne on the involved limb
- Partial weight bearing (PWB): Client is allowed to bear only a portion of body weight on lower extremities. It is sometimes expressed as a percentage of body weight (example 20% to 70%)
- Toe touch weight bearing (TTWB): Only the toes of the affected extremity contact the floor to improve balance
Weight bearing as tolerated (WBAT): Weight bearing is limited by patient tolerance of weight borne on extremity.
Effectiveness[edit | edit source]
A 2017 study into "Do Canes or Walkers Make Any Difference? NonUse and Fall Injuries" reported that of the people who fell at home, most did not have an assistive device with them when they fell. Nonusers who fall sustain more severe injuries. The concluding thoughts were that providers must place increased emphasis on the importance of cane/walker use for injury prevention via patient education, promoting personal relevance, proper fitting, and training. Also new strategies are needed to improve device acceptability and accessibility.[7]
Limitations[edit | edit source]
- Rollators: Studies have shown a reduction in the use of the quadriceps during the stance phase due to a reduction in knee extensor movement. There is also an increase in hip flexion throughout the stance phase due to the increased forward trunk flexion. "The reduced knee flexion during rollator-walking could possibly explain the reduced dorsiflexion of the ankle joint observed in this situation." [8]
- Quad Stick/Cane: heavier than a standard stick/cane. Require a slower walking pattern (gait).
- Reduced stability: Up to 30% of the time people were using their 2 wheel or non-wheel zimmer frames/ walker incorrectly by not putting the appropriate amount of weight through the frame when stepping.[9]
References[edit | edit source]
- ↑ mmlearn.org Assistive Devices: Which One Should I Use? Available from: https://www.youtube.com/watch?v=QNyY-hwP3NA (last accessed 27.6.2019)
- ↑ Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Archives of physical medicine and rehabilitation. 2005 Jan 1;86(1):134-45. Available from: https://www.archives-pmr.org/article/S0003-9993(04)00474-5/fulltext (last accessed 27.6.2019)
- ↑ Allet L, Leeman B, Guyen E, Murphy L,Monnin D, Herrmann FR, Schnider A. Effect of different walking aids on walking capacity of patients with poststroke hemiparesis. Arch Physi Med Rehabil. 2009; 90 (8): 1408–1413. Accessed 1 February 2019.
- ↑ Gooberman-Hill R, Ebrahim S. Making decisions about simple interventions: older people's use of walking aids. Age Ageing, 2007; 36 (5): 569–573. Accessed 1 February 2019.
- ↑ Bateni H, Maki BE. Assistive devices for balance and mobility: Benefits, demands, and adverse consequences. Arch Phys Med Rehab. 2005; 86 (1): 134–145. Accessed 1 February 2019.
- ↑ O'Sullivan SB, Schmitz TJ, Fulk G. Physical rehabilitation. FA Davis; 2013 Jul 23.
- ↑ Luz C, Bush T, Shen X. Do canes or walkers make any difference? Nonuse and fall injuries. The Gerontologist. 2017 Apr 1;57(2):211-8. Available from: https://academic.oup.com/gerontologist/article/57/2/211/2631943 (last accessed 27.6.2019)
- ↑ Alkjaer T, Larsen PK, Pedersen G, Nielsen LH, Simonsen EB. Biomechanical analysis of rollator walking. Biomed Eng Online. 2006;5:2. Published 2006 Jan 6. doi:10.1186/1475-925X-5-2 (Last accessed 19 Feb 2020)
- ↑ Thies SB, Bates A, Costamagna, E, Costamagna, E, Kenney, L, Granat, M, Webb, J, Howard, D, Baker, R. Dawes H, Are older people putting themselves at risk when using their walking frames?.BMC Geriatrics 20, 90 (2020). https://doi.org/10.1186/s12877-020-1450-2