Paraneoplastic Syndrome
Original Editors -Brittany Chorley &Seth Chorleyfrom Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Seth Chorley, Brittany Chorley, Lucinda hampton, Kim Jackson, Priya Gulla, Admin, Elaine Lonnemann, Rujuta Naik, WikiSysop, Vidya Acharya, Claire Knott, 127.0.0.1, Wendy Walker, Mariam Hashem and Adam Vallely Farrell
Introduction[edit | edit source]
Paraneoplastic syndromes (PNS) occur due to the systemic effect of a malignancy and occur remotely to the primary malignancy. Symptoms are brought about by cytokines, hormones or immune cross-reactivity. These syndromes can cause a manifold of symptoms and can affect numerous systems.[1] PNS can occur concurrently with tumour diagnosis, before tumour is diagnosed and even after tumours have been resected[2]. The symptoms typically presents in the middle-aged to older population. Also, it is common in individuals with lung, ovarian, lymphatic, or breast cancer. The most common cancer associated with paraneoplastic syndrome is small cell cancer of the lungs. [3]
Etiology[edit | edit source]
PNS are largely due to two main causes:
- Those due to tumour secretions of hormones, functionally active peptides, enzymes cytokines
- Those due to tumours operating through auto-immune/immunological mechanisms with cross-reacting antibodies between neoplastic and normal tissues. Nb Remission of symptoms often follows resection of humoral secretory tumours but not always of tumours due to immunological mechanisms[2].
Epidemiology[edit | edit source]
PNS occur in up to 15% of patients with cancer.[1] Neurological manifestation in the form of neuropathies is common. Males and females are affected equally.[4]
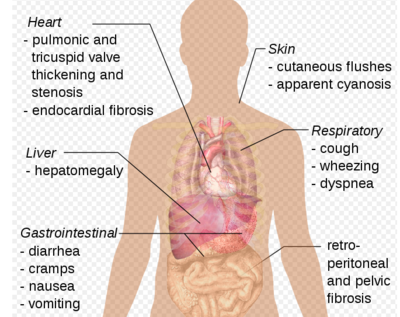
Clinical Presentation[edit | edit source]
PNS can affect multiple systems and have various presentations. Some examples are given below, categorized based on the organ system involved.
- Paraneoplastic neurological syndromes: encephalitis (paraneoplastic rhombencephalitis, limbic encephalitis); Lambert-Eaton myasthenic syndrome; Optic neuropathy; Cerebellar degeneration.
- Endocrine eg Cushing syndrome; Syndrome of inappropriate antidiuretic hormone secretion (SIADH); Hypercalcemia
- Rheumatological eg Paraneoplastic polyarthritis; Polymyalgia rheumatica; Multicentric reticulohistiocytosis; Hypertrophic osteoarthropathy
- Paraneoplastic haematologic syndromes: Good syndrome; Polycythaemia[1]
- Dermatological eg Acanthosis nigricans; Paraneoplastic pemphigus; Sweet syndrome; Leukocytoclastic vasculitis; Dermatomyositis
- Renal eg Electrolyte imbalance (hypokalemia, hypo or hypernatremia, hyperphosphatemia) causing nephropathy and acid-base disturbance due to ectopic hormones produced by tumor cells such as ACTH and ADH. Nephrotic syndrome can also be one of the manifestations of paraneoplastic syndrome.
- Miscellaneous eg Fever, cachexia, anorexia, dysgeusia[4]
Management[edit | edit source]
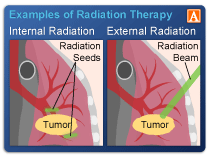
Management of the patients is based on type, severity, and location of the paraneoplastic syndrome. First, therapeutic options are to treat underlying malignancy with chemotherapy, radiation, or surgery.
- Other therapeutic options are immunosuppression with corticosteroids or other immunosuppressive drugs, intravenous immunoglobulins, plasma exchange, or plasmapheresis.
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
First, a health care provider will perform a clinical exam that would include a general physical and neurological screening.
- Tests that would be involved in the neurological screening could include reflexes, sensation, myotomes, balance, and coordination.
Laboratory tests that could be utilized to diagnose paraneoplastic syndrome include:
- Blood tests: This may identify antibodies typically associated with paraneoplastic syndrome. However, some people who have the syndrome do not have the antibody, and some people who do not have the syndrome actually have the antibody. Blood tests can also identify an infection, disorder of nutrient processing, or hormone disorder.
- Spinal tap: A neurologist or nurse will insert a needle into your lumbar spine to extract a small amount of cerebrospinal fluid (CSF). At times, paraneoplastic antibodies may be present in the CSF but not in the blood.
Imaging tests that could be utilized to diagnose paraneoplastic syndrome include:
If the physicians cannot find a malignant tumor, the syndrome may be the cause of a tumor that is too small to locate. In this instance, the physician will continue to have follow-up imaging conducted every three to six months for a several years unless the cause is identified. [5]
Physical Therapy Management[edit | edit source]
People with paraneoplastic syndrome can have difficulty with walking, balance, coordination, muscle tone, sensory of where the body is in space, and vertigo.
- All of these symptoms the physical therapist can treat with traditional therapy.
- Precautions must be taken into account for the cancer or neoplasm that is involved.[3]
Differential Diagnosis[edit | edit source]
- Abdominal Aortic Aneurysm
- Anemia
- Antithrombin Deficiency
- Attention Deficit Hyperactivity Disorder
- Bone Marrow Failure
- Chronic Fatigue Syndrome
- Dermatomyositis
- Diabetes Mellitus, Type 1
- Glomerulonephritis, Acute
- Mixed Connective-Tissue Disease
- Myelodysplastic Syndrome
- Nephrotic Syndrome
- Personality Disorders
- Polycythemia Vera
- Polymyalgia Rheumatica
- Scleroderma
- Superficial Thrombophlebitis
- Systemic Lupus Erythematosus
- Undifferentiated Connective-Tissue Disease [6]
Case Reports/ Case Studies[edit | edit source]
A case of paraneoplastic syndrome accompanied by two types of cancer: jnnp.bmj.com/content/72/3/408.full.pdf+html
Conclusion[edit | edit source]
The diagnosis and management of paraneoplastic syndromes is difficult.
- In most cases, there is an underlying malignancy responsible.
- Due to the numerous causes, the condition is best managed by an interprofessional team (including a pathologist, oncologist, radiologist, hematologist, nurse specialist, and an internist).
- Once the cause is discovered, it needs to be treated.
The management of the patients is based on type, severity, and location of the paraneoplastic syndrome.
- First, therapeutic options are to treat underlying malignancy with chemotherapy, radiation, or surgery.
- Other therapeutic options are immunosuppression with corticosteroids or other immunosuppressive drugs, intravenous immunoglobulins, plasma exchange, or plasmapheresis.[4]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Paraneoplastic syndromes Available: https://radiopaedia.org/articles/paraneoplastic-syndromes(accessed 24.1.2023)
- ↑ 2.0 2.1 Henry K. Paraneoplastic syndromes: definitions, classification, pathophysiology and principles of treatment. InSeminars in diagnostic pathology 2019 Jul 1 (Vol. 36, No. 4, pp. 204-210). WB Saunders.Available from:https://www.sciencedirect.com/science/article/abs/pii/S0740257019300097 (last accessed 15.7.2020)
- ↑ 3.0 3.1 National Institute of Neurological Disorders and Stroke. NINDS Paraneoplastic Syndromes Information Page. http://www.ninds.nih.gov/disorders/paraneoplastic/paraneoplastic.htm. (accessed 18 March 2013).
- ↑ 4.0 4.1 4.2 Thapa B, Ramphul K. Paraneoplastic syndromes. InStatPearls [Internet] 2020 Jun 27. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK507890/ (last accessed 15.7.2020)
- ↑ Mayo Clinic. Paraneoplastic syndromes of the nervous system. http://www.mayoclinic.com/health/paraneoplastic-syndromes/DS00840. (accessed 18 March 2013).
- ↑ Medscape Reference. Paraneoplastic Syndromes. http://emedicine.medscape.com/article/280744-differential. (accessed 18 March 2013).