Stress Fractures
Introduction[edit | edit source]
Stress fractures refer to fractures occurring in the bone due to a mismatch of bone strength and chronic mechanical stress placed upon the bone.[1] Stress fractures represent a spectrum of injuries ranging from periostitis, caused by inflammation of the periosteum, to a complete stress fracture that includes a full cortical break.
They are relatively common overuse injuries in athletes, caused by repetitive submaximal loading on a bone over time. Often seen in running and jumping athletes and are associated with increased volume or intensity of training workload. Most common in the lower extremities and are specific to the sport. Upper extremity stress injuries (usually of ulna) are much less common and are also the result of overuse and fatigue.[2]
Terminology:
- A pathological fracture are fractures that occur in abnormal bone and occur spontaneously or following minor trauma that would not otherwise fracture biomechanically normal bone, this is not a stress fracture.
- Some authors use the term stress fracture synonymously with fatigue fracture.
This article is about Fatigue fractures, often simply termed a stress fracture.[1]
This great 6-minute video sums up stress fractures.
Pathophysiology[edit | edit source]
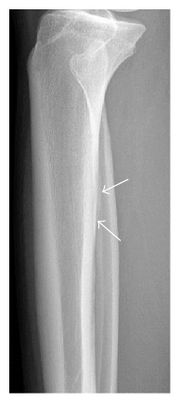
Healthy bone is in constant homeostasis between microcrack creation and repair. Fatigue failure of the bone has three stages: crack initiation, crack propagation, and complete fracture. Crack initiation typically occurs at sites of stress concentration during bone loading. Crack propagation occurs if loading continues at a frequency or intensity above the level at which new bone can be laid down and microcracks repaired. Continued loading allows for the coalescence of multiple cracks to the point of becoming a clinically symptomatic stress fracture. If the loading episodes are not modified or the reparative response is not increased the stress fracture can continue until structural failure or complete fracture occurs.[4] The Xray image shows a subtle periosteal stress fracture of the tibia.
Epidemiology /Etiology[edit | edit source]
Stress fractures are the partial or complete fracture of a bone as a result of sub-maximal loading. Normally, submaximal forces do not result in the fracture but with repetitive loading and inadequate time for healing and recovery, stress fractures can potentially occur. It still is unknown if the cause is contractile muscle forces acting on a bone or increased fatigue of supporting structures; it is likely that both contribute.
- Up to 20% of all sports medicine clinic injuries may be related to stress injuries[2]
- Stress fractures are more common in weight-bearing than non-weight bearing limbs. Stress fractures of the tibia, metatarsals, and fibula are the most frequently reported sites. Medial tibial stress syndrome, also known as shin splints, is the most common form of early stress injury. This diagnosis reflects a spectrum of medial tibial pain in early manifestations before developing into a stress fracture.
- The location of stress injuries varies by sport. The ulna is the upper extremity bone most frequently affected.[2] Women experienced stress fractures at higher rates than men, more often in the preseason, and predominantly in the foot and lower leg[5]:
- Track athletes - fractures to the navicular, tibia, and metatarsals are most common.
- Distance runners - the tibia and fibula are most common.
- Dancers - the metatarsals are most afflicted.
- Military recruits- calcaneus and metatarsals are the most commonly fractured site.
- Intrinsic factors can include:[6]
- Low bone density
- Sex: female > male
- History of stress fracture
- Hormonal status: late menarche (>15 years of age), oligo or amenorrhea
- BMI < 19
- Low energy availability and/or eating disorder
- Systemic medical conditions that affect metabolic and/or nutritional status, such as thyroid dysfunction
Characteristics/Clinical Presentation[edit | edit source]
Symptoms can vary widely but a common complaint is pain with activity which subsides with rest.
- Pain that gradually worsens over time when continuing the aggravating activity.
- Swelling and tenderness may also be present around the area of pain.
Differential Diagnosis[edit | edit source]
Stress fractures should be considered in patients who present with tenderness or edema after a recent increase in activity or repeated activity with limited rest. The differential diagnosis varies based on location, commonly includes[7]
- Tendinopathy
- Compartment syndrome
- Nerve or artery entrapment syndrome
- Shin splints
Diagnostic Procedures[edit | edit source]
- Bone scans for many years been regarded as the gold standard for evaluating stress-induced injuries. Although recently supplanted by magnetic resonance imaging (MRI), it continues to be widely utilized in many situations.[4]
- Radiography - Two thirds of initial radiographs are normal early in the course of a stress fracture half ultimately prove positive once healing begins to occur (specific but not sensitive). Even after healing has begun to occur, radiographic findings can be subtle and may be easily overlooked[4]
- MRI is an effective diagnostic technique in patients who show strong clinical manifestations of a stress fracture but have normal initial radiographs.
- CT delineates the bone well, useful when the diagnosis of a stress injury is difficult eg tarsal navicular stress fractures as well as linear stress fractures that may occur in the tibia.[4]
Examination[edit | edit source]
See specific pages for specific areas
Patients will report[2]
- History of insidious onset of pain without any specific trauma.
- Often a history of a significant volume of a specific exercise such as running, an increase in training intensity or volume, or a change in training surface.
- Initially, symptoms are made worse when training only but may progress to pain with activities of daily living. The symptoms often improve with cessation of activity.
On examination
- Focal tenderness on the area of a suspected stress injury.
- There may be soft tissue swelling. Soft tissue tenderness will tend to suggest muscle injury, early stress reaction, or another etiology of the pain whereas bony tenderness is more likely to suggest stress fracture.
- Some areas of stress injuries may be more clinically subtle or difficult to examine such as the pelvis and sacrum thus requiring the clinician to have a higher index of suspicion from the history alone.
- A “one leg hop test” can be used to distinguish between medial tibial stress syndrome and tibial stress fractures. Patients with stress injuries can tolerate repeated jumping whereas stress fractures cannot hop without pain. Of note, the landing is typically when the patient notices the pain.
Physical Therapy Management[edit | edit source]
Correct management needs to be specific to an individual. In most cases, the initial management will include a period of rest to allow the stress fracture to heal, this may involve the use of crutches or wearing a weight-bearing boot in moderate to severe cases, to reduce the bone’s weight-bearing loads.
In the early stages, treatment includes- analgesia, modified weight-bearing, and activity modification including discontinuing the offending activities. If the patient cannot ambulate without pain, temporary immobilization is indicated. Examples of activity modification include water fitness, cycling, and elliptical exercise to maintain strength and fitness. Progression, after a period of pain-free rest, involves a gradual return to activity over the subsequent weeks including continued physical therapy.
Rehabilitation and strengthening, as well as a gradual return to activity, are extremely important to prevent or reduce the likelihood of re-injury. It is of key importance to develop a specific program to enable your clients to safely and efficiently return to their activity or sport.
Patient’s symptoms should be monitored and the patient should be kept pain-free during progression back to activity. Pain should not worsen during or after stopping exercise.
If symptoms return, activity modification (reduction of load, volume, and/or intensity or use of non-impact mode) and further investigation for other etiologies may be needed.[6]
Education and risk factor modification/optimization are key in prevention. eg
- Proper footwear for specific type of exercise
- Gradual build up -hen starting a new exercise program
- Walk/warm up prior to running
- Stretch + strengthen muscles
- Cool down properly after exercise
Management of Stress Fractures by Region.[edit | edit source]
Regarding specific types of stress fractures, management varies[2]:
- Femoral shaft: Most femoral shaft stress injuries can be managed conservatively including rest, activity modification, and protected weight-bearing. If the patient has low bone mineral density, is older than 60 years old, or has fracture completion or displacement, ORIF with an intramedullary nail is indicated.
- Patella: Patellar stress injuries can be managed conservatively with immobilization and gradual return to activity.
- Tibia: Most tibial shaft stress injuries can be managed conservatively. This includes activity restriction and protected weight-bearing. If the “dreaded black line” is present and violates the anterior cortex, then ORIF with intramedullary tibial nailing or plating may be indicated. This depends on the duration of conservative treatment and the patient’s occupation and the sport in which the patient participates. Medial tibial plateau stress fractures can be managed conservatively. Medial malleolus stress fractures can typically be managed conservatively but should be discussed with one’s orthopedic surgeon.
- Fibula: Fibular stress injuries can be managed conservatively with rest, immobilization, activity modification, and a gradual return to play.
- Tarsals: Calcaneal stress injuries respond well to conservative management with rapid healing and return to activity. Navicular stress injuries are at high risk of nonunion. They can be managed conservatively including non-weight-bearing for up to 12 weeks with close follow up before beginning return to play, or if there’s a completed fracture line, ORIF with screw fixation is typically performed. Medial cuneiform and some talus stress injuries can also be managed conservatively.
- Metatarsal Fractures: Metatarsal Stress Fractures in the Athletic Population
Non lower limb stress fractures:
- Rib: See Rib stress fracture in rowers
- Pars interarticularis of the lumbar spine, see Lumbar Spondylolysis in Extension Related Sport
- Pelvis: Pelvic stress injuries are managed conservatively with rest, crutches (if required), and a gradual return to sport.
Concluding Remarks[edit | edit source]
Stress injuries are common injuries related to overtraining with inadequate recovery time.
Most stress injuries will improve with rest, analgesia, activity modification, cross-training, and a gradual return to sport.
Many low-risk stress injuries can be managed non-operatively with a gradual return to play.
Certain high-risk stress injuries require surgical intervention. Some stress injuries may require surgical intervention if conservative measures fail.[2]
References[edit | edit source]
- ↑ 1.0 1.1 Radiopedia Stress fractures Available:https://radiopaedia.org/articles/stress-fracture-2?lang=us (accessed 12.12.2022)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Kiel J, Kaiser K. Stress reaction and fractures. InStatPearls [Internet] 2019 Jun 4. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507835/ (last accessed 30.11.2019)
- ↑ Ohio state medical centre Stress Fractures, Explained by Ohio State Sports Medicine Available from: https://www.youtube.com/watch?v=AVS99bCKwzQ (last accessed 30.11.2019)
- ↑ 4.0 4.1 4.2 4.3 Miller TL, Best TM. Taking a holistic approach to managing difficult stress fractures. Journal of orthopaedic surgery and research. 2016 Dec;11(1):98. Available from: https://josr-online.biomedcentral.com/articles/10.1186/s13018-016-0431-9 (last accessed 30.11.2019)
- ↑ Rizzone KH, Ackerman KE, Roos KG, Dompier TP, Kerr ZY. The epidemiology of stress fractures in collegiate student-athletes, 2004–2005 through 2013–2014 academic years. Journal of athletic training. 2017 Oct;52(10):966-75. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28937802 (last accessed 30.11.2019)
- ↑ 6.0 6.1 Denay KL. Stress Fractures. Current sports medicine reports. 2017 Jan 1;16(1):7-8. Available from: https://journals.lww.com/acsm-csmr/Pages/articleviewer.aspx?year=2017&issue=01000&article=00005&type=Fulltext (last accessed 1.12.2019)
- ↑ Patel DS, Roth M, Kapil N. Stress fractures: diagnosis, treatment, and prevention. American family physician. 2011 Jan 1;83(1). Available from: https://www.aafp.org/afp/2011/0101/p39.html (last accessed 30.11.2019)