Knee Osteoarthritis
Original Editors - Fien Selderslaghs, Laura Van Der Perren, Mirabella Smolders, Liese Magnus
Top Contributors - Mirabella Smolders, Laura Van Der Perren, Hamelryck Sascha, Abbey Wright, Laura Ritchie, Lucinda hampton, Kim Jackson, Jessica Davis, Fien Selderslaghs, Venugopal Pawar, Rachael Lowe, Bo Hellinckx, Vidya Acharya, Admin, Ophélie Schraepen, Candace Goh, 127.0.0.1, Feebe Robyns, Joni Roesems, Arthur Devoldere, Jelien Wouters, Evan Thomas, Anthony Mertens, Rucha Gadgil, Michelle Lee, Barb Clemes, Jess Bell, Kai A. Sigel, Sai Kripa, WikiSysop, Aminat Abolade, Simisola Ajeyalemi, Robin Tacchetti and Rishika Babburu
Introduction[edit | edit source]
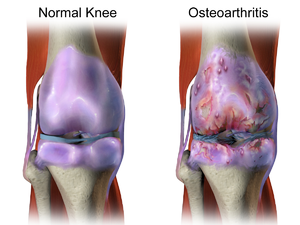
Knee osteoarthritis (OA), also known as degenerative joint disease, is typically the result of wear and tear and progressive loss of articular cartilage. It is most common in elderly people and can be divided into two types, primary and secondary:
- Primary osteoarthritis - is articular degeneration without any apparent underlying cause.
- Secondary osteoarthritis - is the consequence of either an abnormal concentration of force across the joint as with post-traumatic causes or abnormal articular cartilage, such as rheumatoid arthritis (RA).
Osteoarthritis is typically a progressive disease that may eventually lead to disability. The intensity of the clinical symptoms may vary from each individual. However, they typically become more severe, more frequent, and more debilitating over time. The rate of progression also varies for each individual.
Common clinical symptoms include
- Knee pain that is gradual in onset and worse with activity,
- Knee stiffness and swelling,
- Pain after prolonged sitting or resting.
Treatment for knee osteoarthritis begins with conservative methods and progresses to surgical treatment options when conservative treatment fails. While medications can help slow the progression of RA and other inflammatory conditions, no proven disease-modifying agents for the treatment of knee osteoarthritis currently.[1]
Relevant Anatomy[edit | edit source]
The knee (art. genus) is a synovial joint, which consists of 2 articulations.
- Tibiofemoral joint is located between the convex femoral condyles and the concave tibial condyles (the primary joint).[3]
- Patellofemoral joint between the Femur and the Patella
OA can occur in either or both of these articulations of the knee, it is usual that the patellofemoral joint is affected first.[4]
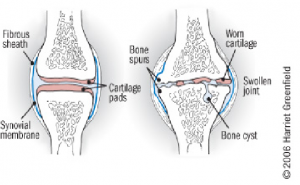
Pathological Process[edit | edit source]
The process of osteoarthritis affects the articular cartilage (mainly type II) that covers the articular surfaces of bone[1]:
- Articular cartilage is normally maintained in a healthy equilibrium of chemical reactions
- In the early stages of OA, chondrocytes secrete tissue inhibitors and attempt to increase the synthesis of proteoglycans to match the degradative process, this repairative process is not enough.
- The loss in equilibrium results in a decreased amount of proteoglycans despite increased synthesis, increase in water content, the disorganised pattern of collagen, and ultimately loss of articular cartilage elasticity.
- Macroscopically these changes result in cracking and fissuring of the cartilage and ultimately erosion of the articular surface.[1]
- Cartilage that has been damaged, cannot recover.
- The cartilage will continue to wear away
- Once the cartilage has worn away; bony surfaces will start to be affected, the bone will expand and spurs (osteophytes) will develop.[5][6]
“The pathogenesis of knee OA have been linked to biomechanical and biochemical changes in the cartilage of the knee joint.”[7]
Not only the cartilage can be affected, there can also occur laxity of the ligaments and muscle atrophy. [8] [9]
Epidemiology[edit | edit source]
- According to The Journal of the American Medical Association (JAMA) more than 10 million Americans are affected with knee osteoarthritis.[10]
- The most commonly affected joint is the knee[11]
- Most commonly affects population age 45 plus.
- Osteoarthritis eventually leads to pain and loss of function.[11]
- Osteoarthritis is the most common disease of joints adults affecting from worldwide.
- Osteoarthritis is the most prevalent form of arthritis and occurs especially in the knee joint
- It affects nearly 6% of all adults, but more women are affected than men.[11]
- Prevalence will continue to increase as life expectancy and obesity rises.
- Age is a determining factor in the development of OA.
- Roughly 13% of women and 10% of men 60 years and older have symptomatic knee osteoarthritis.
- Among those older than 70 years of age, the prevalence rises to as high as 40%.
- Not everyone who demonstrates radiographic findings of knee osteoarthritis will be symptomatic (15% of patients with radiographic findings of knee OA were symptomatic)
- Not factoring in age, the incidence of symptomatic knee osteoarthritis is roughly 240 cases per 100,000 people per year[1]
Etiology[edit | edit source]
Knee osteoarthritis is classified as either primary or secondary, depending on its cause. Primary knee osteoarthritis is the result of articular cartilage degeneration without any known reason. This is typically thought of as degeneration due to age as well as wear and tear. Secondary knee osteoarthritis is the result of articular cartilage degeneration due to a known reason. Possible Causes of Secondary Knee OA
- Obesity
- Joint hypermobility or instability
- Sport stress with high impact loading
- Repetitive knee bending or heavy weight lifting
- Specific occupations
- Peripheral neuropathy
- Injury to the joint (see image)
- History of immobilisation
- Family history
Characteristics/Clinical Presentation[edit | edit source]
Signs of knee osteoarthritis are pain at the beginning of the movement, later on, pain during movement and eventually permanent pain. These patients will also experience a loss of function like stiffness, decreased range of motion (ROM) and impairment in everyday activities. Other possible characteristics of knee OA are bony enlargement, crepitus, joint-line tenderness and elevated sensitivity to cold and/or damp.[12]
- Pay attention to the history as knee pain can be referred from the lumbar spine or the hip joint.
- It is equally important to obtain a detailed medical and surgical history to identify any risk factors associated with secondary knee OA.[1]
We can subdivide knee osteoarthritis in 5 stages:
- Stage 0: This is the “normal” knee health, without any pain in the joint functions.
- Stage 1: A person in this stage has very minor bone spur growth and is not experiencing any pain or discomfort.
- Stage 2: This is the stage where people will experience symptoms for the first time. They will have pain after a long day of walking and will sense a greater stiffness in the joint. It is a mild stage of the condition, but X-rays will already reveal greater bone spur growth. The cartilage will likely remain at a healthy size.
- Stage 3: Stage 3 is considered as a moderate osteoarthritis. People with this stage will experience a frequent pain during movement. The joint stiffness will also be more present, especially after sitting for long periods and in the morning. The cartilage between the bones shows obvious damage, and the space between the bones is getting smaller.
- Stage 4: This is the most severe stage of osteoarthritis. The joint space between the bones will be dramatically reduced, the cartilage will almost be completely gone and the synovial fluid will be decreased. That is why people will experience lots of pain and discomfort during walking or moving the joint.[13]
Diagnosis[edit | edit source]
The diagnosis can be established by clinical examination, and it can be confirmed by X-rays.
Diagnostic Tests[edit | edit source]
Blood Tests; to help determine the type of arthritis
X-ray: The basic X-ray is used to research breakdown of cartilage, narrowing of joint space, forming of bone spurs and to exclude other causes of pain in the affected joint.
Radiographic Findings of OA[edit | edit source]
- Joint space narrowing
- Osteophyte formation
- Subchondral sclerosis
- Subchondral cysts[1]
- Early stage of osteoarthritis show a minimal unequal joint space narrowing.
- If it deteriorates same problems with a lateral subluxation of the tibia as well.
- If it deteriorates more, the joint line will disappear completely(The image shows that the medial joint space is more narrow than the lateral joint space).[12]
Arthrocentesis: This is a procedure which can be performed at the doctor’s office. A sterile needle is used to take samples of joint fluid which can then be examined for cartilage fragments, infection or gout.
Arthroscopy: is a surgical technique where a camera is inserted in the affected joint to obtain visual information about the damage caused to the joint by the osteoarthritis.
MRI. Magnetic resonance imaging (MRI) does not use radiation but is more expensive than X-rays. Provides a view that offers better images of cartilage and other structures to detect early abnormalities typical of osteoarthritis[14].
Treatment/Management[edit | edit source]
Treatment for knee osteoarthritis can be broken down into non-surgical and surgical management. Initial treatment begins with non-surgical modalities and moves to surgical treatment once the non-surgical methods are no longer effective. A wide range of non-surgical modalities is available for the treatment of knee osteoarthritis. These interventions do not alter the underlying disease process, but they may substantially diminish pain and disability.
Non-Surgical Treatment Options[edit | edit source]
- Patient education
- Activity modification
- Physical therapy
- Weight loss
- Knee bracing
- Acetaminophen
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- COX-2 inhibitors
- Glucosamine and chondroitin sulfate
- Corticosteroid injections
- Hyaluronic acid (HA)
- The first-line treatment for all patients with symptomatic knee osteoarthritis includes patient education and physical therapy. A combination of supervised exercises and a home exercise program have been shown to have the best results. These benefits are lost after 6 months if the exercises are stopped.
- Weight loss is valuable in all stages of knee osteoarthritis. It is indicated in patients with symptomatic arthritis with a body mass index greater than 25. The best recommendation to achieve weight loss is with diet control and low-impact aerobic exercise.
- Knee bracing in the setting of osteoarthritis includes unloader-type braces which shift the load away from the involved knee compartment. This may be useful in the setting where either the lateral or medial compartment of the knee is involved such as in a valgus or varus deformity.
- Drug therapy is also the first-line treatment for patients with symptomatic osteoarthritis. There are a wide variety of NSAIDs available, and the choice should be based on physician preference, patient acceptability, and cost. The duration of treatment with NSAIDs should be based on effectiveness, adverse effects, and past medical history. There is strong evidence for NSAID use based on the AAOS guidelines.
- Glucosamine and chondroitin sulfate are available as dietary supplements. They are structural components of articular cartilage, and the thought is that a supplement will aid in the health of articular cartilage. No strong evidence exists that these supplements are beneficial in knee OA; in fact, there is strong evidence against the use according to the AAOS guidelines.
- Intra-articular corticosteroid injections may be useful for symptomatic knee osteoarthritis, especially where there is a considerable inflammatory component. The delivery of the corticosteroid directly into the knee may reduce local inflammation associated with osteoarthritis and minimize the systemic effects of the steroid.
- Intra-articular hyaluronic acid injections (HA) injections are another injectable option for knee osteoarthritis. HA is a glycosaminoglycan that is found throughout the human body and is an important component of synovial fluid and articular cartilage. HA breaks down during the process of osteoarthritis and contributes to the loss of articular cartilage as well as stiffness and pain. Local delivery of HA into the joint acts as a lubricant and may help increase the natural production of HA in the joint.[1]
Differential Diagnosis[edit | edit source]
Bursitis; Iliotibial band syndrome; ligamentous instability (medial and lateral collateral ligaments); Meniscal pathology; Gout and Pseudogout; Rheumatoid arthritis; Septic arthritis.[1][15]
Physical Examination[edit | edit source]
Inspection: Mind the position of the joints when in rest and how the patient moves. This can be accomplished by making the patient perform simulations of daily activities such as getting up from and down on a chair, stair climbing, etc.
Palpation: Mind: swelling, temperature differences, muscle tonus. Also be wary of possible bone spurs (osteocytes) that have formed on the edge of the joint. These osteocytes are a serious indication towards osteoarthritis.
Examination of basic functions: Testing of muscle power, coordination, mobility, balance and also stability of the joint. These factors can be tested by active test like standing on one leg and passive manual tests. When testing stability of the joint muscle strength and proprioception are of significant importance.
Evaluation and History[edit | edit source]
Primary[16]:More commonly diagnosed[12]
- Pain
- Joint line tenderness
- Stiffness, particularly in the morning
- Sensitivity when kneeling or bending[13]
- Decrease in the abilities of daily functioning
Secondary: This type of OA can be caused by obesity, trauma, inflammatory or genetically[12]
- Loss of mobility in the affected joint
- Decrease in muscle power
- Instability of the joint
- Crepitations
Physical Therapy Management[edit | edit source]
Physical therapy can be your first line of defence for managing knee OA symptoms. Pain is a common symptom that occurs in many levels (e.g. mild, moderate and severe). Exercises[17] have been proven to be effective as pain management and also improving physical functioning (e.g. muscle strengthening and aerobic condition) on short term.[12] In order to perform it correctly, exercises have to take place under the supervision of a health care professional such as a physiotherapist. When properly instructed these exercises can be performed at home, though research has shown that group exercise combined with home exercise is more effective.[18] Aerobic walking, strengthening of the quadriceps, resistance training and tai chi are a few examples of exercises that can be efficacious for knee OA patients.[12]
Main Goals of Physiotherapy[edit | edit source]
- Reduce knee pain and inflammation.
- Normalise knee joint range of motion.
- Strengthen lower kinetic chain: esp quadriceps (esp VMO) and hamstrings, and including calves, hip and pelvis muscles.
- Improve your patellofemoral alignment and function.
- Normalise muscle length via stretching and mobilisations.
- Improve proprioception, agility and balance.
- Improve function eg walking, squatting.
- Educate regarding activity modification, if necessary.
- Educate regarding weight loss (if appropriate) and general fitness/exercise.
- Teach in use of gait aide of appropriate.
Land-based exercises are ideal for most clients. Strongly recommend by guidelines[19] for knee OA, land-based exercises are appropriate for all clients regardless of their age, structural disease severity, functional status or pain levels. Exercise has also been found to be beneficial for other comorbidities and overall health. Walking, muscle-strengthening exercise, stationary cycling, Hatha yoga and Tai Chi are examples of such exercises. Individualised exercise program are always the best, taking into account the person’s preference, capability, and the availability of resources and local facilities. Realistic goals should be set. Dosage should be progressed with full consideration given to the frequency, duration and intensity of exercise sessions, number of sessions, and the period over which sessions should occur. Attention should be paid to strategies to optimise adherence.
The video below gives 5 good home exercises for people with knee osteoarthritis.
When being treated, other aspects such as self-management and education, are of crucial importance as well.[17] There are various forms of therapeutic interventions that may or may not be helpful for patients with knee OA as listed in the guidelines and include: Hydrotherapy; manual therapy; massage therapy; thermotherapy; electrotherapy; ultrasound; bracing; surgery and postoperative exercises. See table below.
| Hydrotherapy |
Is a non-invasive and non-interventional therapeutic intervention that is recommended in international guidelines.[12] Although there is some contradictory evidence hydrotherapy can be useful in cases where pain is too grave to exercise on dry land. Many consider water-based exercises as a good preparation of exercise ashore. [21] Knee osteoarthritis mostly affects the weight-bearing joints and leads, amongst other things, to pain and muscle weakness. The strength of muscles around the affected joints can be built up by graduated exercises making use of buoyancy and floats (in the later stage of the treatment).[22] , [23].[23] It has been shown that water buoyancy can reduce the weight that joints, bones and muscles have to carry.[24] Range of motion can also be maintained and increased[23]using the freedom of movement offered by the water with the support given by the buoyancy. Functional difficulties of osteoarthritis patients are generally walking and climbing stairs and much can be done to re-educate such patients in the pool.[23]. Many patients are more mobile in water than on land and this gives them greater confidence and a sense of achievement. Examples of hydrotherapeutic exercises:
Despite the controversy, other studies show that aquatic exercises (Aquatherapy) have some short-term beneficial effects.[25]. Thus, the results indicate that hydrotherapy is applicable and efficient for patients with knee OA. Though there are short-term effects, long-term effects have yet to be investigated.[24] Aquatic exercise may therefore be considered as the first part of an exercise therapy program to get particularly disabled patients introduced to training.[25] |
| Manual therapy |
Has proven effective to locate and eliminate factors like pain and joint immobility. However, it is only effective when combined with active exercise. This progress can enable further or advanced exercises. One study proved that manual therapy can relieve pain and decrease stiffness.[26] |
| Massage therapy |
Until recently massage has been proven not to be effective in the case of osteoarthritis. One study has shown that this therapeutic intervention, which uses both Swedish (including effleurage, pétrissage, fricition, tapotement and vibration) and the standard massage technique is safe, reduces pain and improves function.[27] |
| Thermotherapy |
Contrary to heat application, which did not have significant effects, ice massage and packs have showed to improve both ROM (range of motion) and physical function. Whether ice packs relieve pain is still unknown, thus further investigation is needed.[28] |
| Electrotherapy |
Transcutaneous electrical nerve stimulation is an example of electrotherapy, which has beneficial effects on relieving pain and improving physical function.[12], [29]TENS is a stimulation that uses electrical currents, which are applied directly to the skin and surrounding the knee.[12] Despite the positive effects, electro stimulation is not effective on improving strengthening of the quadriceps.[25] |
| Ultrasound |
Older studies have claimed that this therapeutic option is not beneficial in the treatment of knee osteoarthritis. However, newer studies have shown that ultrasound reduces pain and improves the aerobic condition.[29], [30] |
| External Support Devices |
Braces: Knee braces are used as a therapeutic procedure for patients with OA that involves the medial and lateral tibiofemoral compartments. Their purpose is to diminish the articular contact stress in those compartments. There are various types of braces [12]
Taping: Has proven to be slightly effective in decreasing pain and disability for patients with knee OA.[22] These beneficial effects are short-termed. |
| Surgery and post-operative exercise |
Surgery is only recommended when therapies are not effective. There are various types of knee OA surgery[12]:
Post- operative exercises are very much recommended. Exercises to improve the function of the new joint and muscle strengthening are most effective.[18] |
Medical Managment[edit | edit source]
In some cases, patients with knee arthritis choose to undergo knee surgery for knee arthritis. The most common forms of surgery for this condition are
- Therapeutic Injections,
- Arthroscopes,
- Osteotomy[1]
- Unicompartmental knee arthroplasty
- Total knee replacements.
- If symptoms are reaching an unmanageable level and treatment results have plateaued surgical options may be of benefit.
The below video gives a good guide to both surgical and non surgical options and why or when they are offered.
Conservative Treatment[edit | edit source]
Ottawa Panel of evidence suggests the use of therapeutic exercises or exercises with manual therapy to be most beneficial for patients with knee OA. [32]Deyle et al. found that knee mobilization gave statically improvements in WOMAC and 6 minute walk tests for both 4 week, 8 week, and 1 year follow up.[33]
A CPR (clinical prediction rules) for patients with knee pain to indicate those patients have knee OA, and which patients are likely to have short term benefits from hip mobilizations (confirmed by studies[34][35]) found this CPR:
1. Hip and groin parasthesia
2. Groin pain
3.Passive knee flexion less than 122 degrees
4.Passive hip IR less than 17 degrees
5.Pain with hip distraction”.[34]
If the patient has 2 variables then the positive likely hood ratio is 12.9.
Conclusion[edit | edit source]
Knee osteoarthritis (OA) is best managed by an interprofessional team that consists of an orthopedic surgeon, rheumatologist, physical therapist, dietitian, a pain specialist, and internist.
- The disorder has no cure and thus attempts should be made to prevent progression of the disorder.
- The patient should be referred to a dietitian for weight loss and to physical therapy to regain joint function and muscle strength.
- Treatment for knee osteoarthritis begins with conservative methods and progresses to surgical treatment options when conservative treatment fails.
- The pharmacist should look at the patient's medications to ensure there are no interactions and that the dosing and indications are all correct.
- While medications can help slow the progression of RA and other inflammatory conditions, no proven disease-modifying agents for the treatment of knee osteoarthritis currently exist.[1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Hsu H, Siwiec RM. Knee Osteoarthritis.2019 Available from:https://www.ncbi.nlm.nih.gov/books/NBK507884/ (last accessed 28.2.2020)
- ↑ rBioventus Stages of knee OA Available from: https://www.youtube.com/watch?v=BBqjltHNOrc&feature=youtu.be (last accessed 17.11.2019)
- ↑ Jennifer Reft. Knee Osteokinematics and Arthokinematics. Available from: http://www.youtube.com/watch?v=EyhiCvWER0Y [last accessed 07/12/2014]
- ↑ Brukner P, Clarsen B, et al. Brukner & Khan's Clinical sports medicine 5th edition. McGraw Hill Education; 2017; p777
- ↑ J.A. Buckwalter, et al., Articular cartilage and osteoarthritis, 2005, 54: 465-480
- ↑ A.D. Pearle, et al., Basic science of articular cartilage and osteoarthritis, Elsevier Sounders, 2005: 1-12
- ↑ K. Uth, et al., Stem cell application for osteoarthritis in the knee joint: A minireview, World Journal of Stem Cells, 2014, 6(5): 629–636
- ↑ E. Schulte, et al., General anatomy and musculoskeletal system, Atlas of Anatomy, 2006: 372-373
- ↑ C. Logan, The knee joint, Idea health & fitness association, 2005, 2(1)
- ↑ Parmet S. JAMA patient page: osteoarthritis of the knee. Jama. 2003;289:1068.
- ↑ 11.0 11.1 11.2 Michael JW, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Deutsches Arzteblatt International. 2010 Mar;107(9):152.
- ↑ 12.00 12.01 12.02 12.03 12.04 12.05 12.06 12.07 12.08 12.09 12.10 RK Arya, Vijay Jain, Osteoarthritis of the knee joint: An overview, Journal Indian Academy of Clinical Medicine, 2013, 14(2): 154-62
- ↑ 13.0 13.1 G. Krucik, et al., Stages of Osteoarthritis of the knee, Healthline, 2013
- ↑ Osteoarthritis Diagnosis Arthritis Foundation Available from: https://www.arthritis.org/about-arthritis/types/osteoarthritis/diagnosing.php (last accessed 17.11.2019)
- ↑ E. RINGDAHL, et al., Treatment of Osteoarthritis, American Family Physician, 2011, 83(11):1287-1292.
- ↑ EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis, W Zhang, M Doherty, G Peat, et al., Ann Rheum Dis 2010;69:483–489. doi:10.1136/ard.2009.113100 ( Quality level C : literature study)
- ↑ 17.0 17.1 T.E. McAlindon et al., OARSI guidelines for the non-surgical management of knee osteoarthritis, Osteoarthritis Research Society International, 2014, 22: 363-388
- ↑ 18.0 18.1 Supplementing a home exercise program with a class-based exercise program is more effective than home exercise alone in the treatment of knee osteoarthritis ,C. J. McCarthy, P. M. Mills1, R. Pullen, C. Roberts, A. Silman and,J. A. Oldham, Rheumatology 2004;43:880–886
- ↑ RACGP Guidelines for hip and knee arthritis Available from: https://www.racgp.org.au/download/Documents/Guidelines/Musculoskeletal/guideline-for-the-management-of-knee-and-hip-oa-2nd-edition.pdf (last accessed 18.11.2019)
- ↑ Bob and Brad 5 Proven Exercises for Knee Osteoarthritis or Knee Pain- Do it Yourself Available at: https://www.youtube.com/watch?v=T3qKHLP8fVo&feature=youtu.be (last accessed 17.11.2019)
- ↑ Bartels et al., Aquatic exercise for the treatment of knee and hip osteoarthritis (Review),The Cochrane Library 2007, Issue 4
- ↑ 22.0 22.1 Hinman, R.S., Heywood, S.E. (2007). Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Journal of Physical Therapy 87 (1), 32-43
- ↑ 23.0 23.1 23.2 23.3 Wang, T., Belza, B., Elaine Thompson, F., Whitney, J.D., Bennett, K. (2007) Effects of aquatic exercise of flexibility, strength and aerobic fitness in adults with osteoarthritis of the hip or knee. Journal of Advanced Nursing, 57 (2), 141-152
- ↑ 24.0 24.1 L.E. Silva et al., Hydrotherapy Versus Conventional Land-Based Exercise for the Management of Patients With Osteoarthritis of the Knee: A Randomized Clinical Trial, Physical Therapy Journal, 2008, 88(1): 12-21
- ↑ 25.0 25.1 25.2 A Clinical Trial of Neuromuscular Electrical Stimulation in Improving Quadriceps Muscle Strength and Activation Among Women With Mild and Moderate Osteoarthritis, Riann M. Palmieri-Smith, Abbey C. Thomas, Carrie Karvonen-Gutierrez, MaryFran Sowers, Physical Therapy - Volume 90 Number 10 October 2010
- ↑ G.D. Deyle et al., Physical Therapy Treatment Effectiveness for Osteoarthritis of the Knee: A Randomized Comparison of Supervised Clinical Exercise and Manual Therapy Procedures Versus a Home Exercise Program, Physical Therapy Journal, 2005, 85(12): 1301-1317
- ↑ A.I. Perlman et al., Massage Therapy for Osteoarthritis of the Knee, Archives of Internal Medicine, 2006, 166: 2533-2538
- ↑ L. Brosseau et al., Thermotherapy for treatment of osteoarthritis (Review), The Cochrane Library, 2011, 10: 1-23
- ↑ 29.0 29.1 N.C. Mascarin et al., Effects of kinesiotherapy, ultrasound and electrotherapy in management of bilateral knee osteoarthritis: prospective clinical trial, BMC Musculoskeletal Disorders, 2012, 13: 182-191
- ↑ A. Loyola-Sánchez et al., Efficacy of ultrasound therapy for the management of knee osteoarthritis: a systematic review with meta-analysis, Osteoarthritis Research Society International Journal, 2010, 18: 1117-1126
- ↑ Mayo Clinic Mayo Clinic's Approach to Knee Arthritis - Both Surgical and Non-Surgical Available from: https://www.youtube.com/watch?v=4Mk9GZ7-Dz8 (last accessed 17.11.2019)
- ↑ No authors listed. Ottawa panel evidence-based clinical practice guidelines for therapeutic exercises and manual therapy in the management of osteoarthritis. Phys Ther. 2005 Sep; 85 (9):907-71.
- ↑ Deyle Gail, Henderson Nancy, Matekel Robert, Ryder Micahel, Garber Matthew, Allison Stephen. Effectiveness of Manual Physical therapy and Exercise in Osteoarthritis of the Knee A Randomized, Controlled Trial
- ↑ 34.0 34.1 Linda L Currier, Paul J Froehlich, Scott D Carow, Ronald K McAndrew, Amy V Cliborne, Robert E Boyles, Liem T Mansfield and Robert S Wainner. Development of a Clinical Prediction Rule to Identify Patients With Knee Pain and Clinical Evidence of Knee Osteoarthritis Who Demonstrate a Favorable Short-Term Response to Hip Mobilization. PHYS THER Vol. 87, No. 9, September 2007, pp. 1106-1119
- ↑ Cliborne Amy, Rhon Dan, Judd Coy, Fee Terrance, Matekel Robert, Whitman Julie, Roberts Maj. Clinical hip tests and a functional squat test in patients with knee osteoarthritis: Reliability, Prevalence of Positive Test Findings, and Short-Term Response to Hip Mobilization. J Orthop Sports Phys Ther. 2004;34(11):676-685. doi:10.2519/jospt.2004.1432
37. Seyed Mansour Rayegani 1 , Seyed Ahmad Raeissadat 1 , Saeed Heidari 2 , Mohammad Moradi-Joo 3,4. Safety and Effectiveness of Low-Level Laser Therapy in Patients With Knee Osteoarthritis: A Systematic Review and Meta-analysis. S12–S19 2017 Aug 29.