Patella
Original Editor - Venus Pagare
Top Contributors - Venus Pagare, Memoona Awan, Kim Jackson, Admin, 127.0.0.1, Evan Thomas, WikiSysop and Leana Louw
Introduction[edit | edit source]
The patella (derived from Latin means 'small plate') is a flat, inverted triangular bone, situated on the front of the knee joint.[1] It is the largest sesamoid bone, developed in the tendon of the Quadriceps femoris, and resembles these bones as it is...
- developed in a tendon
- its centre of ossification has a knotty or tuberculated outline
- it's composed mainly of dense cancellous tissue.
Osteological Features[edit | edit source]
It has an anterior and a posterior surface, three borders, and an apex.[3]
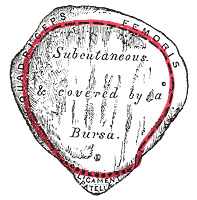
SURFACES
- The subcutaneous anterior surface is convex in all directions, perforated by small apertures for the passage of nutrient vessels, and marked by numerous rough, longitudinal striae. This surface is covered, in the recent state, by an expansion from the tendon of the Quadriceps femoris, which is continuous below the superficial fibres of the ligamentum patellae. It is separated from the integument by a bursa.[3]
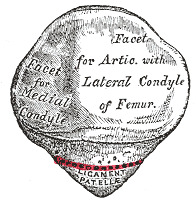
- The posterior surface is covered with articular cartilage up to 4 to 5 mm thick. This helps in the dissipation of the force.
- It presents above a smooth, oval, articular area, divided into two facets by a vertical ridge; the ridge corresponds to the groove on the patellar surface of the femur, and the facets to the medial and lateral parts of the same surface; the lateral facet is the broader and deeper. The medial facet shows significant anatomic variation. The 3rd odd facet exists along the extreme medial border of the medial facet.[4]
BORDERS & MUSCLE ATTACHMENTS
- The base or superior border is thick, rough and sloped from behind, downward, and forward: it gives attachment to that portion of the Quadriceps femoris which is derived from the Rectus femoris and Vastus intermedius.[5]
- The medial and lateral borders are thinner and converge below: they attach to those portions of the Quadriceps femoris derived from the Vasti lateralis and medialis.
APEX
- The apex is pointed and gives attachment to the ligamentum patellae [1]
- In a relaxed standing position, the apex lies just proximal to the knee joint line[1]
Structure[edit | edit source]
The patella consists of a nearly uniform dense cancellous tissue, covered by a thin compact lamina. The cancelli immediately beneath the anterior surface are arranged parallel with it. In the rest of the bone, they radiate from the articular surface toward the other parts of the bone.
Ossification[edit | edit source]
The patella is ossified from a single centre, which usually makes its appearance in the second or third year, but may be delayed until the sixth year. More rarely, the bone is developed by two centres, placed side by side. Ossification is completed at about the age of puberty.
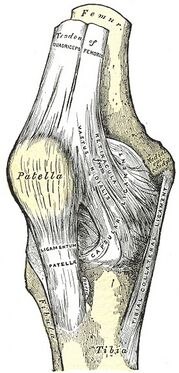
Articulation[edit | edit source]
The patella articulates with the femur to form the Patellofemoral Joint
Functions of the patella[edit | edit source]
The patella plays the following role at the knee joint:
- Functions primarily as an anatomic pulley for the quadriceps muscle. It increases the lever arm of the extensor mechanism allowing for more effective knee flexion and thus increases quadriceps strength by 33–50%.
- Earlier, the patella was considered to be a frictionless pulley, in which the force of the patellar tendon equals the force of the quadriceps tendon. However, recent studies have shown that the patella acts more like a balance beam, adjusting the length, direction and force of each of its arms- the quadriceps tendon and the patella tendon- at different degrees of flexion. With increasing flexion, the patellofemoral contact area moves from distal to proximal on the patella surface. This change in contact area results in a change in the lever arm and mechanical advantage provided by the patella to the quadriceps.
- Interposed between the quadriceps tendon and the femoral condyles it acts as a “spacer” and protects the tendon by reducing the friction and compressive stress and minimizes the concentration of stress by transmitting forces evenly to the underlying bone.
Clinical Relevance[edit | edit source]
Patellar Dislocation
Sudden forceful twisting of the knee causes dislocation of the patella bone causing it to displace out of the patellofemoral groove. It mostly occurs laterally and comprises around 3% of knee injuries. Patellar dislocations are more common in sports such as football, rugby and ice hockey.[6]
Patellar Fracture
Patellar fractures are more common in males of the 20-50 age range and usually occur from sudden contraction of the quadriceps muscle or direct trauma to the bone. It will usually separate the proximal fragment and be displaced superiorly by the quadriceps tendon while the distal fragment is pulled inferiorly by the patellar ligament.[6]
Assessment[edit | edit source]
Some tests such as the Patellar tap test, Patellar grind test/ Clark's sign, and Patellar apprehension sign can be used to assess and diagnose.
Treatment[edit | edit source]
Certain knee-strengthening exercises keep the parts of the leg in line such as squatting. Manual techniques such as mobilization to improve ROM. Supportive braces or taping are also used to ease pain and make you able to exercise. Icing your knee after exercise might be helpful.
During the recovery phase knee friendly sports such as bicycling or swimming help strengthen muscles.
Surgical and other procedures: In more severe cases, a surgeon may need to perform arthroscopy or realignment surgery to fix the angle of the kneecap or relieve pressure on the cartilage.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Neumann DA. Kinesiology of the musculoskeletal system: Foundations for Physical Rehabilitation.2nd Ed.Elsevier Health Sciences;2009
- ↑ 2.0 2.1 Cox CF, Sinkler MA, Black AC, et al. Anatomy, Bony Pelvis and Lower Limb, Knee Patella. [Updated 2023 Oct 27]. In: StatPearls [Internet] Treasure Island (FL): StatPearls Publishing. 23AD Oct;
- ↑ 3.0 3.1 http://education.yahoo.com/reference/gray/subjects/subject/60
- ↑ Levangie PK, Norkin CC. Joint Structure and Function : A Comprehensive Analysis. 4th ed. India: JAYPEE; 2006.
- ↑ Levangie PK, Norkin CC. Joint Structure and Function : A Comprehensive Analysis. 4th ed. India: JAYPEE; 2006.
- ↑ 6.0 6.1 Cassidy A. The Patella [Internet]. TeachMe Anatomy. 2023 [cited 23AD Dec 21].
- ↑ nabil ebraheim. Basic Anatomy Of The Patella - Everything You Need To Know - Dr. Nabil Ebraheim. Available from:https://www.youtube.com/watch?v=X__7PDT4LjM [last accessed 22/12/2023]
- ↑ Mike Reinold. Quick Assessment for Patellar Instability. Available from: https://www.youtube.com/watch?v=ZH_lHsZH-lM [last accessed 22/12/2023]
- ↑ Tone and Tighten. Fix Knee Cap Pain FAST! Exercises For Patellofemoral Pain. Available from: https://www.youtube.com/watch?v=kLKHZgu_czI [last accessed 22/12/2023]