Introduction to Foot Neuropathy
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (7/08/2023)
Original Editor - User Name
Top Contributors - Stacy Schiurring, Jess Bell and Matt Huey
Introduction[edit | edit source]
diabetes is a global epidemic. It's been found to affect more than 537 million adults worldwide. 75% of those individuals have been found to come from low- to middle-income countries or low- to middle-income regions of more affluent countries. It is believed that 50% of individuals with diabetes are undiagnosed, and those that are diagnosed have been found to have diabetes for many years prior to their diagnosis. 6,7 million deaths have been attributed to diabetes, although the article did not mention the timeframe that involved that number. Diabetes accounts for 9% of total health care costs for adults, and the complications of foot and lower extremity issues related to diabetes affects 40 to 60 million people worldwide. The prevalence of neuropathy in one study was found to be anywhere from 10 to 85 percent, and the discrepancies found in the various studies were attributed to different definitions of when a diagnosis of neuropathy is made, which caused that huge variable in the prevalence study.
Another startling finding is that less than 33% of physicians surveyed will recognise the signs of a neuropathy when they're evaluating their patient. The lifetime risk of an individual developing a diabetic foot ulcer after they have diabetes is anywhere from 19 to 34 percent. Or put another way, one in four people with diabetes will develop a diabetic foot ulcer at some point in time. A person with diabetes who develops a diabetic foot ulcer is at 2,5 times greater risk of mortality than a person with diabetes who doesn't develop a diabetic foot ulcer. To put that more seriously, a person with a diabetic foot ulcer has a 5% mortality rate within one year. Their mortality rate increases to 42% within 5 years of developing a diabetic foot ulcer. After 5 years of a minor amputation, the mortality rate is 46%. And with a major amputation, after 5 years, the mortality rate increases to 57%. After 1 year, 20% of diabetic foot ulcers remain unhealed. And the recurrence rate after they do heal is 40% within one year and 65% within five years, which is a huge problem for diabetic patients. Once they have a foot ulcer, their risk of developing another one is significantly high.
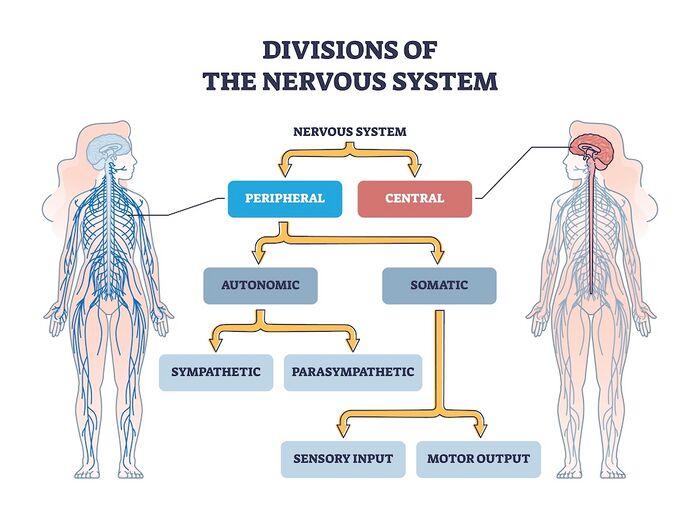
Neuroanatomy Review[edit | edit source]
- Central Nervous System: includes the brain and spinal cord. The central nervous system (CNS) is the body's processing centre. In general terms, the three functions of the CNS are to (1) take in sensory information, (2) process that information, and (3) send out motor signals. Through these mechanisms, the CNS controls most of the body's functions, to include: movement, sensation through our five senses, and higher level functions such as cognition, awareness, and speech. The spinal cord is an extension of the brain and serves as a neural pathway for information exchange with the rest of the body.
- Peripheral Nervous System: a complex network of nerves which convey sensory information in from the body to the CNS via the spinal cord, and transmit information out from the CNS via the spinal cord to the body. Examples of outgoing signals transmitted along the peripheral nervous system (PNS) include (1) motor information for muscle activity and(2) autonomic functioning (heart rate, blood pressure, respiration, digestion, sexual arousal)[1].
- Motor Nerves: relay information to skeletal muscles and somatic tissue, which creates voluntary movement
- Sensory Nerves: conveys sensory information about the environment in from sensory receptors in the body to the CNS
- Autonomic Nervous System: relay motor information to the visceral organs to innervate smooth muscle, cardiac muscle, and glands and functions to maintain the body's homeostasis. The autonomic nervous system has two parts: the sympathetic and parasympathetic divisions which innervate visceral organs. The sympathetic stimulates ("fight or flight") while the parasympathetic inhibits ("rest and digest") their functions.
Peripheral Neuropathy[edit | edit source]
Peripheral neuropathy (PN) describes the many conditions which involve damage to the peripheral nervous system. Initially, that presents as nerve malfunction due to cellular and chemical changes. Eventually, that malfunction becomes true nerve or structural damage, resulting in atrophy and demyelination[2]. There are more than 100 known types of peripheral neuropathy, each with unique symptoms and prognosis. PN symptoms are dependent on the category of nerves involved, motor, sensory, or autonomic[1].
The exact pathophysiology of PN is contingent upon the underlying disease processes, however the mechanisms of peripheral nerve injury exhibit similar patterns. These reactions include (1) segmental demyelination, (2) Wallerian degeneration, and (3) axonal degeneration[3].
Classification methods of PN include:
- Categorisation as mono-neuropathies, multifocal neuropathies, poly-neuropathies and radiculopathies[4][3].
- Further sub-classification by separating PN as axonal, demyelinating, or mixed[3].
Common symptoms of PN include:
To learn more about neuropathy, please read this optional article.
Aetiology of Peripheral Neuropathies[edit | edit source]
The National Institute of Health (NIH) states that PN aetiology can involve many causes, to include metabolic, systemic, and toxicity[3]:
- Diabetes mellitus[2][3]
- Chronic alcoholism[2][3]
- Nutritional deficiencies (e.g., B1, B6, B12, and vitamin E)[2][3]
- Inflammatory conditions (e.g., vasculitis)[3]
- Hypothyroidism[2][3]
- Autoimmune disorders (e.g., Sjogren's syndrome[2], lupus, rheumatoid arthritis)[3]
- Infections (e.g., Lyme disease[2], Epstein-Barr virus, hepatitis C, shingles, leprosy, HIV,[3], and long COVID[5])
- Guillain-Barre syndrome[3]
- Toxins (heavy metals, chemicals such as mercury, lead, and arsenic)[3]
- Chemotherapy agents[2][3]
- Medications (antibiotics, cardiovascular medications)[3]
- Tumors (secondary to compression or associated paraneoplastic syndromes)[3]
- Inherited conditions (e.g., Charcot-Marie-Tooth disease, amyloidosis)[3]
- Trauma/injury (e.g., carpel tunnel syndrome)[3]
- Multiple myeloma and its treatments[3]
- Monoclonal gammopathy of undetermined significance (MGUS)[3][6]
- Idiopathic, when no direction cause can be identified[2]
Types of Peripheral Neuropathies[edit | edit source]
Sensory Neuropathy[edit | edit source]
"Sensory neuropathies refer to a host of diseases that result in loss of sensation throughout the body ... [sensory neuropathy conditions] may further sub-divide into small fiber (pain-dominant) and large fiber (ataxia-predominant) pathologies."[7]
To classify a sensory neuropathy, it is important to identify the size of the nerve fiber and the degree of myelination involved. Some diseases, such Diabetes, can involve sensory polyneuropathy.[7]
- Small fiber neuropathies (Aδ and small unmyelinated C fibers)
- Large fiber neuropathies (Aβ fibers)
Special Topic: Loss of Protect Sensation[edit | edit source]
Loss of Protective Sensation (LOPS) is a complication common to patients with diabetic neuropathy. PN related to diabetes is an "anatomically diffuse process" which affects sensory and autonomic nerve fibers and, in more advanced cases, distal motor fibers. Symptoms tend to develop distally in the toes, then advance by moving proximal. This disease process leads to LOPS meaning the person is unable to sense minor trauma and injury from mechanical, thermal, or chemical causes.[9]
Common mechanisms of injury related to LOPS:
- Exposure to constant, prolonged pressure such as wearing shoes that are too tight
- Exposure to moderate to high repetitive pressure which causes the development of a callus which in turn acts as a source of pressure
- Exposure to brief high pressure such as stepping on a sharp object which causes a wound or other injury[2]
For more information on testing for LOPS, please read this article.
Motor Neuropathy[edit | edit source]
Motor neuropathy results from damage to the motor nerves.
Signs of motor neuropathy include:
- Foot deformities resulting from muscle imbalances within the foot
- Common deformities include (1) hammer toe, (2) claw toe, and (3) pes equinu
- Changes in gait pattern due to tendon shortening
- Tendons commonly effected include (1) Achilles tendon and the (2) flexor hallucis tendons.
- Loss of deep tendon reflexes (DTR's)
Autonomic Neuropathy[edit | edit source]
The third neuropathy that can develop related to diabetes is the autonomic neuropathy. It's often not talked about as much, but it has some significant ramifications to the skin and physiology of the foot as well. An autonomic neuropathy causes dry skin or anhidrosis and hair loss. It also is the main cause of the medial arterial stenosis that develops in the arteries of the foot. The medial lining of the foot becomes calcified, directly related to the effect of diabetes on the circulation, and that stiffens those arteries so they can't respond to environmental changes as they should.
There's also systemic changes related to the autonomic neuropathy that can affect the gastrointestinal system, the cardiac system, the urogenital system. One of the most common ways that that's recognised is when someone has a silent heart attack. Because they don't have sensation, they don't recognise that their heart muscle is being damaged from an ischaemic event. They don't recognise their heart attack, and it can go untreated. In many cases, that's fatal because they don't get the treatment that they need. Injuries that you might see due to the autonomic neuropathy are things like, because of a sweating dysfunction, you can get really wet skin, which can create problems or more often really dry skin because of lack of sweating, and that can cause the skin to start to crack and fissure and lead to dermal openings where that wound can then develop an infection.
Another autonomic neuropathy effect is the increased glycation of keratin, which causes that really thickened, taut, inflexible skin on the foot. Because the skin is so taut and not flexible, there is an additional pressure against the bony prominences, which can cause an ischaemic ulcer to develop over those areas. There's also the decreased vasodilatory response, as I talked about, due to that medial calcinosis of the arteries in the foot.
Sub Heading 3[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 National Institute of Health. Peripheral Neuropathy. Available from: https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy#toc-what-is-peripheral-neuropathy- (accessed 3/August/2023).
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Merwarth, D. Understanding the Foot Programme. Introduction to Foot Neuropathy. Physioplus. 2023.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 Hammi C, Yeung B. Neuropathy. 2022 Available from;https://www.ncbi.nlm.nih.gov/books/NBK542220/(last accessed 5/August/2023)
- ↑ Martyn CN, Hughes R. Epidemiology of peripheral neuropathy. Journal of neurology, neurosurgery, and psychiatry. 1997 Apr;62(4):310.
- ↑ Oaklander AL, Mills AJ, Kelley M, Toran LS, Smith B, Dalakas MC, Nath A. Peripheral neuropathy evaluations of patients with prolonged long COVID. Neurology-Neuroimmunology Neuroinflammation. 2022 May 1;9(3).
- ↑ Rögnvaldsson S, Steingrímsson V, Turesson I, Björkholm M, Landgren O, Kristinsson SY. Peripheral neuropathy and monoclonal gammopathy of undetermined significance: a population-based study including 15,351 cases and 58,619 matched controls. haematologica. 2020 Nov 11;105(11):2679.
- ↑ 7.0 7.1 7.2 7.3 National Institute of Health. Sensory Neuropathy. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559020/ (accessed 6/August/2023).
- ↑ 8.0 8.1 Misra UK, Kalita J, Nair PP. Diagnostic approach to peripheral neuropathy. Annals of Indian Academy of Neurology. 2008 Apr;11(2):89.
- ↑ Centers for Medicare & Medicaid Services. Diabetic Peripheral Neuropathy with Loss of Protective Sensation (LOPS). Available from: https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=N&NCAId=22&%3Bfromdb=true#:~:text=Long%20nerves%20are%20affected%20first,%2C%20thermal%2C%20or%20chemical%20sources. (accessed 6/August/2023).