Introduction to Foot Neuropathy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Diabetes is a global epidemic, affecting more than 537 million adults worldwide.<ref name=":7">Hicks CW, Wang D, Windham BG, Matsushita K, Selvin E. [https://www.nature.com/articles/s41598-021-98565-w Prevalence of peripheral neuropathy defined by monofilament insensitivity in middle-aged and older adults in two US cohorts]. Scientific reports. 2021 Sep 27;11(1):19159.</ref> Of those, 40 to 60 million people have diabetic-related foot and lower extremity complications. Diabetes accounts for 9% of total adult health care costs.<ref name=":2" /> | |||
Peripheral neuropathy is a common consequence of diabetes, with a prevalence of anywhere from 10 to 85%.<ref name=":2" />. The outcomes of peripheral neuropathy can be devastating to include (1) foot ulcers, (2) major amputation, (3) falls, (4) intracranial injuries, and (5) decreased quality of life.<ref name=":7" /> Approximately one in four people with diabetes will develop a diabetic foot ulcer, which puts them on a medical slippery slope: | |||
* They have a 2.5 times greater mortality risk than people with diabetes who did not develop a foot ulcer. | |||
* Their mortality rate increases to 42% within 5 years of developing a diabetic foot ulcer. | |||
* After 1 year, 20% of diabetic foot ulcers remain unhealed. | |||
* The recurrence rate for healed diabetic foot ulcers within one year is 40%, and with five years in 65%.<ref name=":2" /> | |||
This article will provide an introduction to the causes and types of peripheral neuropathy, exploring aetiology beyond diabetes. | |||
== Neuroanatomy Review == | == Neuroanatomy Review == | ||
| Line 22: | Line 29: | ||
== Peripheral Neuropathy == | == Peripheral Neuropathy == | ||
The term peripheral neuropathy (PN) describes many conditions which involve damage to the peripheral nervous system. Initially, this damage presents as nerve malfunction due to cellular and chemical changes. However, over time the nerve malfunction becomes true nerve or structural damage, resulting in atrophy and demyelination<ref name=":2">Merwarth, D. Understanding the Foot Programme. Introduction to Foot Neuropathy. Physioplus. 2023.</ref>. There are more than 100 known types of peripheral neuropathy, each with unique symptoms and prognosis. PN symptoms are dependent on the category of nerves involved, motor, sensory, or autonomic<ref name=":0" />. | |||
The exact pathophysiology of PN is contingent upon the underlying disease processes, however the mechanisms of peripheral nerve injury exhibit similar patterns. These reactions include (1) segmental demyelination, (2) [https://www.physio-pedia.com/Wallerian_Degeneration?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Wallerian degeneration], and (3) axonal degeneration<ref name=":1" />. | The exact pathophysiology of PN is contingent upon the underlying disease processes, however the mechanisms of peripheral nerve injury exhibit similar patterns. These reactions include (1) segmental demyelination, (2) [https://www.physio-pedia.com/Wallerian_Degeneration?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Wallerian degeneration], and (3) axonal degeneration<ref name=":1" />. | ||
| Line 43: | Line 50: | ||
The [https://www.nih.gov National Institute of Health] (NIH) states that PN aetiology can involve many causes, to include metabolic, systemic, and toxicity<ref name=":1" />: | The [https://www.nih.gov National Institute of Health] (NIH) states that PN aetiology can involve many causes, to include metabolic, systemic, and toxicity<ref name=":1" />: | ||
* [[Diabetes|Diabetes mellitus]]<ref name=":2" /><ref name=":1" /> | * [[Diabetes|Diabetes mellitus]]<ref name=":2" /><ref name=":1" />(most common cause of PN) | ||
* Chronic [[alcoholism]]<ref name=":2" /><ref name=":1" /> | * Chronic [[alcoholism]]<ref name=":2" /><ref name=":1" /> | ||
* Nutritional deficiencies (e.g., B1, B6, B12, and vitamin E)<ref name=":2" /><ref name=":1" /> | * Nutritional deficiencies (e.g., B1, B6, B12, and vitamin E)<ref name=":2" /><ref name=":1" /> | ||
Revision as of 19:21, 16 August 2023
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (16/08/2023)
Original Editor - User Name
Top Contributors - Stacy Schiurring, Jess Bell and Matt Huey
Introduction[edit | edit source]
Diabetes is a global epidemic, affecting more than 537 million adults worldwide.[1] Of those, 40 to 60 million people have diabetic-related foot and lower extremity complications. Diabetes accounts for 9% of total adult health care costs.[2]
Peripheral neuropathy is a common consequence of diabetes, with a prevalence of anywhere from 10 to 85%.[2]. The outcomes of peripheral neuropathy can be devastating to include (1) foot ulcers, (2) major amputation, (3) falls, (4) intracranial injuries, and (5) decreased quality of life.[1] Approximately one in four people with diabetes will develop a diabetic foot ulcer, which puts them on a medical slippery slope:
- They have a 2.5 times greater mortality risk than people with diabetes who did not develop a foot ulcer.
- Their mortality rate increases to 42% within 5 years of developing a diabetic foot ulcer.
- After 1 year, 20% of diabetic foot ulcers remain unhealed.
- The recurrence rate for healed diabetic foot ulcers within one year is 40%, and with five years in 65%.[2]
This article will provide an introduction to the causes and types of peripheral neuropathy, exploring aetiology beyond diabetes.
Neuroanatomy Review[edit | edit source]
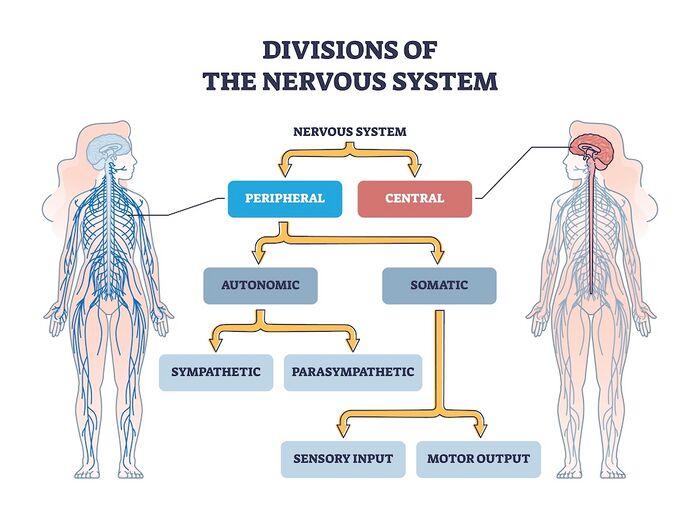
- Central Nervous System: includes the brain and spinal cord. The central nervous system (CNS) is the body's processing centre. In general terms, the three functions of the CNS are to (1) take in sensory information, (2) process that information, and (3) send out motor signals. Through these mechanisms, the CNS controls most of the body's functions, to include: movement, sensation through our five senses, and higher level functions such as cognition, awareness, and speech. The spinal cord is an extension of the brain and serves as a neural pathway for information exchange with the rest of the body.
- Peripheral Nervous System: a complex network of nerves which convey sensory information in from the body to the CNS via the spinal cord, and transmit information out from the CNS via the spinal cord to the body. Examples of outgoing signals transmitted along the peripheral nervous system (PNS) include (1) motor information for muscle activity and(2) autonomic functioning (heart rate, blood pressure, respiration, digestion, sexual arousal)[3].
- Motor Nerves: relay information to skeletal muscles and somatic tissue, which creates voluntary movement
- Sensory Nerves: conveys sensory information about the environment in from sensory receptors in the body to the CNS
- Autonomic Nervous System: relay motor information to the visceral organs to innervate smooth muscle, cardiac muscle, and glands and functions to maintain the body's homeostasis. The autonomic nervous system has two parts: the sympathetic and parasympathetic divisions which innervate visceral organs. The sympathetic stimulates ("fight or flight") while the parasympathetic inhibits ("rest and digest") their functions.
Peripheral Neuropathy[edit | edit source]
The term peripheral neuropathy (PN) describes many conditions which involve damage to the peripheral nervous system. Initially, this damage presents as nerve malfunction due to cellular and chemical changes. However, over time the nerve malfunction becomes true nerve or structural damage, resulting in atrophy and demyelination[2]. There are more than 100 known types of peripheral neuropathy, each with unique symptoms and prognosis. PN symptoms are dependent on the category of nerves involved, motor, sensory, or autonomic[3].
The exact pathophysiology of PN is contingent upon the underlying disease processes, however the mechanisms of peripheral nerve injury exhibit similar patterns. These reactions include (1) segmental demyelination, (2) Wallerian degeneration, and (3) axonal degeneration[4].
Classification methods of PN include:
- Categorisation as mono-neuropathies, multifocal neuropathies, poly-neuropathies and radiculopathies[5][4].
- Further sub-classification by separating PN as axonal, demyelinating, or mixed[4].
Common symptoms of PN include:
To learn more about neuropathy, please read this optional article.
Aetiology of Peripheral Neuropathies[edit | edit source]
The National Institute of Health (NIH) states that PN aetiology can involve many causes, to include metabolic, systemic, and toxicity[4]:
- Diabetes mellitus[2][4](most common cause of PN)
- Chronic alcoholism[2][4]
- Nutritional deficiencies (e.g., B1, B6, B12, and vitamin E)[2][4]
- Inflammatory conditions (e.g., vasculitis)[4]
- Hypothyroidism[2][4]
- Autoimmune disorders (e.g., Sjogren's syndrome[2], lupus, rheumatoid arthritis)[4]
- Infections (e.g., Lyme disease[2], Epstein-Barr virus, hepatitis C, shingles, leprosy, HIV,[4], and long COVID[6])
- Guillain-Barre syndrome[4]
- Toxins (heavy metals, chemicals such as mercury, lead, and arsenic)[4]
- Chemotherapy agents[2][4]
- Medications (antibiotics, cardiovascular medications)[4]
- Tumors (secondary to compression or associated paraneoplastic syndromes)[4]
- Inherited conditions (e.g., Charcot-Marie-Tooth disease, amyloidosis)[4]
- Trauma/injury (e.g., carpel tunnel syndrome)[4]
- Multiple myeloma and its treatments[4]
- Monoclonal gammopathy of undetermined significance (MGUS)[4][7]
- Idiopathic, when no direction cause can be identified[2]
Types of Peripheral Neuropathies[edit | edit source]
Sensory Neuropathy[edit | edit source]
"Sensory neuropathies refer to a host of diseases that result in loss of sensation throughout the body ... [sensory neuropathy conditions] may further sub-divide into small fiber (pain-dominant) and large fiber (ataxia-predominant) pathologies."[8]
To classify a sensory neuropathy, it is important to identify the size of the nerve fiber and the degree of myelination involved. Some diseases, such Diabetes, can involve sensory polyneuropathy.[8]
- Small fiber neuropathies (Aδ and small unmyelinated C fibers)
- Large fiber neuropathies (Aβ fibers)
Special Topic: Loss of Protect Sensation[edit | edit source]
Loss of Protective Sensation (LOPS) is a complication common to patients with diabetic neuropathy. PN related to diabetes is an "anatomically diffuse process" which affects sensory and autonomic nerve fibers and, in more advanced cases, distal motor fibers. Symptoms tend to develop distally in the toes, then advance by moving proximal. This disease process leads to LOPS meaning the person is unable to sense minor trauma and injury from mechanical, thermal, or chemical causes.[10]
LOPS is an important symptom used in the classification of diabetic foot wounds[11] because the foot is more vulnerable to physical and thermal trauma and predisposes it to deformity.[12]
Common mechanisms of injury related to LOPS:
- Exposure to constant, prolonged pressure such as wearing shoes that are too tight
- Exposure to moderate to high repetitive pressure which causes the development of a callus which in turn acts as a source of pressure
- Exposure to brief high pressure such as stepping on a sharp object which causes a wound or other injury[2]
For more information on testing for LOPS, please read this article.
Motor Neuropathy[edit | edit source]
Motor neuropathy is the result of damage to the motor nerves.[2]
Signs of motor neuropathy include:
- Foot deformities resulting from muscle imbalances within the foot[2] and the non-enzymatic glycation of proteins.
- Common deformities include (1) hammer toe, (2) claw toe, and (3) pes equinu[2]
- Changes in gait pattern due to tendon shortening
- Tendons commonly effected include (1) Achilles tendon and the (2) flexor hallucis tendons[2]
- Loss of deep tendon reflexes (DTR's)[2]
- Other symptoms can include:
- muscle twitching and cramps
- muscle weakness or paralysis
- muscle wasting[13]
Add images from Diane's lecture
Autonomic Neuropathy[edit | edit source]
"Autonomic neuropathies are a collection of syndromes and diseases affecting the autonomic neurons, either parasympathetic or sympathetic, or both. Autonomic neuropathies can be hereditary or acquired in nature."[14]
Signs and symptoms of autonomic neuropathy can present across a wide variety of body systems. Many of these impairments can affect a patient's gait pattern putting them at greater risk for foot dysfunction and wound formation. Impairments such as changes in the frequency and urgency to get to the bathroom, and their ability to effectively scan the environment and see for safety awareness can increase their fall risk.
- Cardiovascular system.
- Digestive system. Digestive difficulties can include:[15]
- feelings of bloating, fullness, and nausea
- vomiting
- constipation
- diarrhea
- fecal incontinence
- gastroparesis
- swallowing impairments
- Urogenital system.
- Bladder impairments[15]
- impaired ability to sense need to void
- urinary incontinence
- bladder infections stemming urinary retention
- Bladder impairments[15]
- Integumentary system.
- Non-enzymatic glycation of protein[2][16]
- Causes thickened, taut, inflexible skin on the foot. These skin changes present additional pressures against bony prominences which can put the patient at risk of developing an ischaemic ulcer over those areas.[2]
- Predisposes skin for formation of skin fissures.[2] [16]
- Causes contracture of the fascial structures, which can lead to joint deformity of the foot[16]
- Impaired wound healing[16]
- Sweat glands.
- Non-enzymatic glycation of protein[2][16]
- Eyes. Can experience difficulty with pupil adaptation to changes in light, and night blindness when driving.[15]
- Can develop hypoglycemia unawareness.[15]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 Hicks CW, Wang D, Windham BG, Matsushita K, Selvin E. Prevalence of peripheral neuropathy defined by monofilament insensitivity in middle-aged and older adults in two US cohorts. Scientific reports. 2021 Sep 27;11(1):19159.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 Merwarth, D. Understanding the Foot Programme. Introduction to Foot Neuropathy. Physioplus. 2023.
- ↑ 3.0 3.1 National Institute of Health. Peripheral Neuropathy. Available from: https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy#toc-what-is-peripheral-neuropathy- (accessed 3/August/2023).
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 Hammi C, Yeung B. Neuropathy. 2022 Available from;https://www.ncbi.nlm.nih.gov/books/NBK542220/(last accessed 5/August/2023)
- ↑ Martyn CN, Hughes R. Epidemiology of peripheral neuropathy. Journal of neurology, neurosurgery, and psychiatry. 1997 Apr;62(4):310.
- ↑ Oaklander AL, Mills AJ, Kelley M, Toran LS, Smith B, Dalakas MC, Nath A. Peripheral neuropathy evaluations of patients with prolonged long COVID. Neurology-Neuroimmunology Neuroinflammation. 2022 May 1;9(3).
- ↑ Rögnvaldsson S, Steingrímsson V, Turesson I, Björkholm M, Landgren O, Kristinsson SY. Peripheral neuropathy and monoclonal gammopathy of undetermined significance: a population-based study including 15,351 cases and 58,619 matched controls. haematologica. 2020 Nov 11;105(11):2679.
- ↑ 8.0 8.1 8.2 8.3 National Institute of Health. Sensory Neuropathy. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559020/ (accessed 6/August/2023).
- ↑ 9.0 9.1 Misra UK, Kalita J, Nair PP. Diagnostic approach to peripheral neuropathy. Annals of Indian Academy of Neurology. 2008 Apr;11(2):89.
- ↑ Centers for Medicare & Medicaid Services. Diabetic Peripheral Neuropathy with Loss of Protective Sensation (LOPS). Available from: https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=N&NCAId=22&%3Bfromdb=true#:~:text=Long%20nerves%20are%20affected%20first,%2C%20thermal%2C%20or%20chemical%20sources. (accessed 6/August/2023).
- ↑ Swanson T, Ousey K, Haesler E, Bjarnsholt T, Carville K, Idensohn P, Kalan L, Keast DH, Larsen D, Percival S, Schultz G. IWII Wound Infection in Clinical Practice consensus document: 2022 update. Journal of wound care. 2022 Dec 1;31(Sup12):S10-21.
- ↑ Adams OP, Herbert JR, Howitt C, Unwin N. The prevalence of peripheral neuropathy severe enough to cause a loss of protective sensation in a population‐based sample of people with known and newly detected diabetes in Barbados: a cross‐sectional study. Diabetic Medicine. 2019 Dec;36(12):1629-36.
- ↑ NHS. Peripheral neuropathy symptoms. Available from: https://www.nhs.uk/conditions/peripheral-neuropathy/symptoms/ (accessed 6/August/2023).
- ↑ Medscape. Autonomic Neuropathy. Available from: https://emedicine.medscape.com/article/1173756-overview?form=fpf (accessed 6/August/2023).
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 National Institute of Health. Autonomic Neuropathy. Available from: https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/autonomic-neuropathy (accessed 15/August/2023).
- ↑ 16.0 16.1 16.2 16.3 Mooney J. Illustrated Dictionary of Podiatry and Foot Science E-Book. Elsevier Health Sciences; 2009 Jul 30.