Foot and Ankle Structure and Function: Difference between revisions
Evan Thomas (talk | contribs) mNo edit summary |
No edit summary |
||
| (86 intermediate revisions by 17 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
= | == Anatomy == | ||
[[Image:Foot.jpg| | [[Image:Foot.jpg|493x493px|Foot & Ankle|right|frameless]] | ||
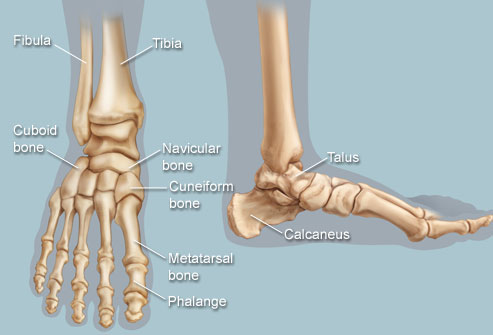
The foot and ankle form a complex system which consists of | The foot and ankle form a complex system which consists of 28 [[Bone|bones]], 33 joints, 112 [[Ligament|ligaments]], controlled by 13 extrinsic and 21 intrinsic [[Muscle|muscles]]. | ||
The foot is subdivided into the rearfoot, midfoot, and forefoot. | |||
The | It functions as a rigid structure for weight bearing and it can also function as a flexible structure to conform to uneven terrain. The foot and ankle provide various important functions which includes: | ||
* Supporting body weight. | |||
* Providing [[balance]]. | |||
* Shock absorption. | |||
* Transferring ground reaction forces. | |||
* Compensating for proximal malalignment. | |||
* Substituting hand function in individuals with upper extremity [[Amputations|amputation]]/paralysis.<ref name="p1">Houglum PA, Bertoti DB. Brunnstrom's clinical kinesiology. FA Davis; 2012</ref> | |||
{| width="100%" cellspacing="1" cellpadding="1" | |||
|- | |||
| {{#ev:youtube|4hCS1O2LP_c|400}}<ref>Anatomy Zone. Ankle Joint - 3D Anatomy Tutorial. Available from: https://www.youtube.com/watch?v=lPLdoFQlZXQ [last accessed 19/03/2015]</ref> | |||
| {{#ev:youtube|ROd1Acma64o|400}}<ref>AnimatedBiomedical. Ankle Joint, Bones of the Foot - 3D Medical Animation. Available from: https://www.youtube.com/watch?v=X-eAXKS4pJM [last accessed 19/03/2015]</ref> | |||
|} | |||
=== Structure === | |||
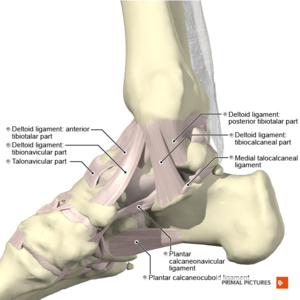
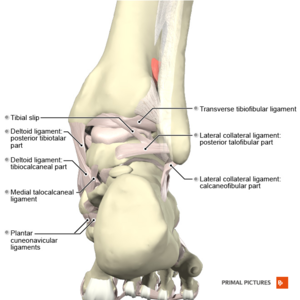
[[File:Ligaments of the ankle medial aspect Primal.png|right|frameless]][[File:Ligaments of the ankle posterior aspect Primal.png|right|frameless]]The ankle or tibiotalar joint constitutes the junction of the lower leg and foot. The osseous components of the ankle joint include the distal [[tibia]], distal [[fibula]], and [[talus]]. | |||
The anatomic structures below the ankle joint comprise the foot, which includes: | |||
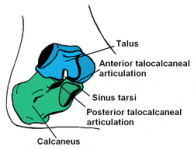
# Hindfoot: Hindfoot, the most posterior aspect of the foot, is composed of the talus and [[calcaneus]], two of the seven tarsal bones. The [[talus]] and calcaneus articulation is referred to as the [[Subtalar joint arthritis|subtalar]] joint, which has three facets on each of the talus and calcaneus. | |||
# Midfoot: The midfoot is made up of five of the seven tarsal bones: [[navicular]], [[cuboid]], and medial, middle, and lateral [[cuneiforms]]. The junction between the hind and midfoot is termed the Chopart's joint, which includes the talonavicular and calcaneocuboid joints. | |||
#Forefoot: The forefoot is the most anterior aspect of the foot. It includes [[metatarsals]], phalanges (toes), and [[Sesamoiditis|sesamoid]] bones. There are a metatarsal and three phalanges for each digit apart from the great toe, which only has two phalanges. The articulation of the midfoot and forefoot forms the [[Lisfranc Injuries|Lisfranc]] joint.<ref name=":0">Ficke J, Byerly DW. [https://www.ncbi.nlm.nih.gov/books/NBK546698/#_article-21883_s2_ Anatomy, Bony Pelvis and Lower Limb, Foot.] InStatPearls [Internet] 2019 Sep 3. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK546698/#_article-21883_s2_ ( last accessed 11.3.2020)</ref> | |||
=== | === Talocrural (TC) Joint === | ||
The [[Ankle Joint|talocrural joint]] is formed between the distal tibia-fibula and the talus, and is commonly known as the ankle joint. The distal and inferior aspect of the tibia – known as the plafond – is connected to the fibula via tibiofibular ligaments forming a strong mortise which articulates with the talar dome distally. It is a hinge [[Joint Classification|joint]] and allows for dorsiflexion and plantarflexion movements in the sagittal plane. | |||
=== | === Subtalar (ST) Joint === | ||
Also known as transverse tarsal joints or Chopart’s joint. It is an S-shaped joint when viewed from above | [[Image:SubtalarJoint.PNG|thumb|right|200x150px|Subtalar Joint]]It is also known as the talocalcaneal joint and is formed between the talus and calcaneus. | ||
* There are three facets on each of the talus and calcaneus. | |||
* The posterior subtalar joint constitutes the largest component of the subtalar joint. | |||
* The subtalar joint allows inversion and eversion of ankle and hindfoot.<ref name=":0" /> | |||
=== Midtarsal (MT) Joint === | |||
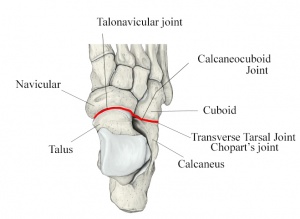
[[Image:Transverse-tarsal-joint.jpg|300x300px|Chopart's Joint|right|frameless]]Also known as transverse tarsal joints or Chopart’s joint. It is an S-shaped joint when viewed from above. It consists of two joints – the Talonavicular Joint and Calcaneocuboid Joint. | |||
#Talonavicular (TN) Joint - Formed between the anterior talar head and the concavity on the navicular. It does not have its own capsule, but rather shares one with the two anterior talocalcaneal articulations. | #Talonavicular (TN) Joint - Formed between the anterior talar head and the concavity on the navicular. It does not have its own capsule, but rather shares one with the two anterior talocalcaneal articulations. | ||
# | #Calcaneocuboid (CC) Joint - Formed between the anterior facet of the calcaneus and the posterior cuboid. Both articulating surface, present a convex and concave surface with the joint being convex vertically and concave transversely. Very little movement occurs at this joint. | ||
=== Tarsometatarsal (TMT) Joint Complex === | |||
Also known as Lisfranc’s joint. | Also known as Lisfranc’s joint. This complex divides the midfoot from forefoot. | ||
The distal tarsal rows including the three cuneiform bones and cuboid articulate with the base of each metatarsal to form the TMT complex. It is an S-shaped joint and is divided into 3 distinct columns<ref name="p1" />: | |||
*Medial – composed of 1st metatarsal and medial cuneiform. | |||
*Middle – composed of 2nd and 3rd metatarsals, intermediate and lateral cuneiforms respectively. | |||
*Lateral – composed of 4th and 5th metatarsals and the cuboid. | |||
=== Metatarsophalangeal (MTP) Joints and Interphalangeal (IP) Joints === | |||
The MTP joints are formed between the metatarsal heads and the corresponding bases of the proximal phalanx. The interphalangeal joints of the toes are formed between the phalanges of the toes. Each toe has proximal and distal IP joints except for the great toe which only has one IP joint. <br> | The MTP joints are formed between the metatarsal heads and the corresponding bases of the proximal phalanx. The interphalangeal joints of the toes are formed between the phalanges of the toes. Each toe has proximal and distal IP joints except for the great toe which only has one IP joint. <br> | ||
| Line 41: | Line 67: | ||
{| border="1" cellpadding="1" cellspacing="1" | {| border="1" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
! scope="col" | Joint | ! scope="col" | Joint | ||
! scope="col" | Type of Joint | ! scope="col" | Type of Joint | ||
! scope="col" | Plane of Movement | ! scope="col" | Plane of Movement | ||
! scope="col" | Motion | ! scope="col" | Motion | ||
|- | |- | ||
| TC joint | | TC joint | ||
| Hinge | | Hinge | ||
| | | Sagittal | ||
| | | Dorsiflexion & Plantarflexion | ||
|- | |- | ||
| ST joint | | ST joint | ||
| | | Condyloid | ||
| | | | ||
Mainly transverse<br> | Mainly transverse<br> | ||
Some sagittal | Some sagittal | ||
| | | | ||
| Line 66: | Line 92: | ||
| MT joint | | MT joint | ||
| | | | ||
TN joint - Ball and socket | TN joint - Ball and socket | ||
CC joint - | CC joint - Modified saddle | ||
| | | | ||
Largely in transverse | Largely in transverse | ||
Some sagittal | Some sagittal | ||
| | | | ||
| Line 82: | Line 108: | ||
|- | |- | ||
| TMT joint | | TMT joint | ||
| | | Planar | ||
| | | | ||
| | | | ||
|- | |- | ||
| MTP joint | | MTP joint | ||
| | | Condyloid | ||
| | | | ||
Sagittal | Sagittal | ||
Some Transverse | Some Transverse | ||
| | | | ||
| Line 100: | Line 126: | ||
|- | |- | ||
| IP joint | | IP joint | ||
| | | Hinge | ||
| | | Sagittal | ||
| | | Flexion & Extension | ||
|} | |} | ||
= | <ref name="p1" /> | ||
== | == Kinematics == | ||
{{#ev:youtube|v=0R4zRSE_-40&t=29s}}<ref>Dr Glass DPM.Ankle & Subtalar Joint Motion Function Explained Biomechanic of the Foot - Pronation & Supination. Published on 21 January 2008. Available from https://www.youtube.com/watch?v=0R4zRSE_-40&t=29s (last accessed 10 June 2019)</ref> | |||
=== Talocrural Joint === | |||
[[File:AnkleAxisPost.jpg|right|frameless|162x162px]] | |||
The tip of the medial malleoli is anterior and superior to the lateral malleoli, which makes its axis oblique to both the sagittal and frontal planes. The axis of rotation is approximately 13°-18° laterally from the frontal plane and at angle of 8°-10° from the transverse plane.<ref name="p1" /><ref name="p7">http://www.pt.ntu.edu.tw/hmchai/Kinesiology/KINlower/Ankle.htm#Kinematics</ref> Motion in other planes is required (like horizontal and frontal plane) to achieve a complete motion for plantarflexion and dorsiflexion.<ref name="p2">Lundberg A, Goldie I, Kalin B, Selvik G. Kinematics of the ankle/foot complex: Plantarflexion and dorsiflexion. Foot and Ankle 9(4):194–200, 1989.</ref> The reported normal available range for dorsiflexion varies in the literature between 0°-16.5°<ref>Baggett BD, Young G. Ankle joint dorsiflexion. Establishment of a normal range. Journal of the American Podiatric Medical Association. 1993 May;83(5):251-4.</ref> and 0°-25°,<ref>CDCP. Normal joint range of motion study. Acceessed https://www.cdc.gov/ncbddd/jointrom/</ref> and this changes with weightbearing. The normal range of plantarflexion has been reported to be around 0°- 50°.<br> | |||
[[File:AnkleAxisSup.jpg|right|frameless|200x200px]] | |||
=== Subtalar Joint[[Image:STJaxis.jpg|right|150x200px]] === | |||
The axis of the subtalar joint lies about 42° superiorly to the sagittal plane and about 16° to 23° medial to the transverse plane.<ref name="p4">http://www.wheelessonline.com/ortho/Sub_talar_joint</ref><ref name="p5">Stagni R, Leardini A, O'Connor JJ, Giannini S. Role of passive structures in the mobility and stability of the human subtalar joint: a literature review. Foot andankle international. 2003 May 1;24(5):402-9.</ref> The literature presents vast ranges of subtalar motion ranging from 5° to 65°<sup>.</sup><ref name="p5" /> The average ROM for pronation is 5° and 20° for supination. Inversion and eversion ROM has been identified as 30° and 18°, respectively.<ref name="p6">Ball P, Johnson GR. Technique for the measurement of hindfoot inversion and eversion and its use to study a normal population. Clinical Biomechanics 11(3):165–169, 1996</ref> Total inversion-eversion motion is about 2:1 and a 3:2 ratio of inversion-to-eversion movement.<ref name="p2" /> | |||
=== Midtarsal Joint === | |||
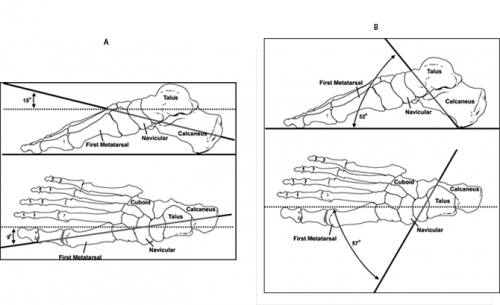
The Midtarsal joint rotates at two axes due to its anatomy, making its motion complex. The longitudinal axis (image 'A' below) lies about 15° superior to the horizontal plane and about 10° medial to the longitudinal plane. The oblique axis (image 'B' below) lies about 52° superior to the horizontal plane and 57° from the midline. The longitudinal axis is close to the subtalar joint axis and the oblique axis is similar to the talocrural joint axis. | |||
[[File:Midtarsal_Longitudinal_axis.png|right|frameless|500x500px]] | |||
==== '''MT Joint Locking''' ==== | |||
An important function of the foot is propulsion of weight during stance phase<ref name="p0">http://www.amputation.research.va.gov/limb_loss_prevention/Midtarsal_Joint_Locking.asp</ref>. This function is made possible by the MT joint locking and unlocking. During heel strike, the foot needs to be flexible in order to adjust to the surface and the MT joint unlocks to provide this flexibility. Later in the gait cycle, the foot then needs to act as a rigid lever to propel the weight of the body forward which is made possible by MT joint locking. During pronation/eversion of the foot, the axis of the TN and CC joints are parallel to each other, making it easier for them to independently move and unlock the MT joint. The axes cross each other during supination/inversion and locks the MT joint making it difficult to move. Blackwood et al<ref name="p9">Blackwood CB, Yuen TJ, Sangeorzan BJ, Ledoux WR. The midtarsal joint locking mechanism. Foot and ankle international. 2005 Dec 1;26(12):1074-80</ref> concluded that there is increased forefoot movement when the calcaneus is everted. This is consistent with the MT joint locking mechanism. | |||
{{#ev:youtube|v=h9OzIw2XCSY}}<ref>Jacqueline Buchman. Midtarsal Joint Oblique Axis. Available from https://www.youtube.com/watch?v=h9OzIw2XCSY (last accessed 30.03.2023)</ref> | |||
=== Lisfranc Joint Complex === | |||
The degree of sagittal motion for each TMT joint is presented below<ref name="p2" /> | |||
The degree of sagittal motion for each TMT joint is presented below | |||
{| border="1" cellpadding="1" cellspacing="1" | {| border="1" cellpadding="1" cellspacing="1" | ||
| Line 134: | Line 164: | ||
| Degree of Motion | | Degree of Motion | ||
|- | |- | ||
| 1st | | 1st | ||
| 1.6<sup>o</sup> | | 1.6<sup>o</sup> | ||
|- | |- | ||
| Line 152: | Line 182: | ||
<br> | <br> | ||
=== MTP and IP joints === | |||
The MTP joints are | The MTP joints are bi-axial and move in sagittal and transverse planes. MTP joints have a greater sagittal plane movement and very little transverse plane movement. At MTP joints, hyperextension is about 90° and flexion is about 30° to 50°. IP joints are hinge joints which limit motion in one direction. | ||
== Arthrokinematics == | |||
[[Arthrokinematics]] refers to the movement of joint surfaces. | |||
#'''Talocrural Joint''' – The talus rolls within the mortise during dorsiflexion and plantarflexion. During dorsiflexion, the talus rolls anteriorly and it glides posteriorly. While with plantarflexion, the talus rolls posteriorly and glides anteriorly. | |||
#'''Subtalar Joint''' – Secondary to the anatomy of the subtalar joint, the coupled motion of dorsiflexion, abduction and eversion produces pronation, whereas the coupled motion of plantarflexion, adduction and inversion produces supination. It presents two point of articulations – anterior talocalcaneal articulation and posterior talocalcaneal articulation.<ref name="p8">https://en.wikipedia.org/wiki/Subtalar_joint</ref> During open kinetic chain inversion, the calcaneus rolls into inversion and it glides/slides laterally. And during eversion, the calcaneus rolls into eversion and it glides/slides medially. | |||
#'''Midtarsal Joint''' – For the Talonavicular joint, the concave navicular moves on the convex talus and hence the roll and glide is in the same direction of movement. The calcaneocuboid joint is a saddle joint so the direction changes depending on the movement. During flexion-extension, the cuboid is concave and the calcaneus is convex; Hence, the roll and glide occurs in the same direction as the talonavicular joint. During abduction-adduction, however, the cuboid is convex and the calcaneus is concave, and therefore the roll and glide occurs in the opposite direction. | |||
#'''Lisfranc Joint''' – Secondary to the bony and ligamentous anatomy of the complex, the primary role is stability of the midfoot as it has very little movement. It has three distinct arches and the main stabilizing structure of TMT joint is a Y-shaped ligament known as Lisfranc’s ligament. | |||
#'''MTP and IP Joints''' – Glide and roll is in the same direction as the movement for the MTP joints, as the concave base of the phalanx moves on the convex head of the metatarsal. The same is true for the IP joints, where glide and roll is in the same direction, as the concave distal phalanx moves on the convex proximal phalanx.<br> | |||
{| border="1" cellpadding="1" cellspacing="1" | {| border="1" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
| Line 183: | Line 210: | ||
| Full dorsiflexion | | Full dorsiflexion | ||
| 10<sup>o</sup> of plantarflexion and midway between pronation and supination | | 10<sup>o</sup> of plantarflexion and midway between pronation and supination | ||
| Limitation of plantarflexion, although clinically dorsiflexion | | Limitation of plantarflexion, although clinically dorsiflexion. | ||
Limitation is more common. | |||
| Proximal - Mortise formed by Tibia, tibiofibular ligament and fibula | | Proximal - Mortise formed by Tibia, tibiofibular ligament and fibula | ||
| Distal - Trochlear surface of Talar dome | | Distal - Trochlear surface of Talar dome | ||
| Line 191: | Line 219: | ||
| Full inversion | | Full inversion | ||
| Inversion/plantarflexion | | Inversion/plantarflexion | ||
| Limitation of inversion in chronic arthritis. Limitation of eversion in traumatic | | Limitation of inversion in chronic arthritis. Limitation of eversion in traumatic. | ||
| Proximal - Anterior, middle and posterior facet of talus | | Proximal - Anterior, middle and posterior facet of talus | ||
| Distal – Calcaneal Anterior, middle and posterior talar articular surface | | Distal – Calcaneal Anterior, middle and posterior talar articular surface | ||
| Line 208: | Line 236: | ||
| Midway between extreme ROM | | Midway between extreme ROM | ||
| Limitation of dorsiflexion, plantarflexion, adduction and internal rotation. | | Limitation of dorsiflexion, plantarflexion, adduction and internal rotation. | ||
| Distal - Cuboid is concave during flexion-extension. <br>Calcaneus is concave during adduction-abduction<br> | | Distal - Cuboid is concave during flexion-extension. <br>Calcaneus is concave during adduction-abduction.<br> | ||
| Proximal - Calcaneus is convex during flexion-extension.<br>Cuboid is convex during adduction-abduction<br> | | Proximal - Calcaneus is convex during flexion-extension.<br>Cuboid is convex during adduction-abduction.<br> | ||
| | | | ||
Flexion-extension = Same direction<br>Adduction-abduction = Opposite direction<br> | Flexion-extension = Same direction<br>Adduction-abduction = Opposite direction<br> | ||
| Line 225: | Line 253: | ||
| Hyperextension | | Hyperextension | ||
| Slight (10<sup>o</sup>) extension | | Slight (10<sup>o</sup>) extension | ||
| Loss of motion more in extension than flexion | | Loss of motion more in extension than flexion. | ||
| Distal - Base of phalanx | | Distal - Base of phalanx | ||
| Proxmial - Head of Metatarsal | | Proxmial - Head of Metatarsal | ||
| Line 233: | Line 261: | ||
| Maximum flexion | | Maximum flexion | ||
| Slight (10<sup>o</sup>) extension | | Slight (10<sup>o</sup>) extension | ||
| Loss of flexion | | Loss of flexion. | ||
| Distal - Base of phalanges | | Distal - Base of phalanges | ||
| Proximal - Head of metatarsals | | Proximal - Head of metatarsals | ||
| Line 241: | Line 269: | ||
| Full extension | | Full extension | ||
| Slight flexion | | Slight flexion | ||
| Restriction in all direction with more in extension | | Restriction in all direction with more in extension. | ||
| Distal Phalanx | | Distal Phalanx | ||
| Proximal Phalanx | | Proximal Phalanx | ||
| Line 247: | Line 275: | ||
|} | |} | ||
= | == Gait and the Foot == | ||
[[File:8 phases of gait cycle.png|right|frameless|363x363px]] | |||
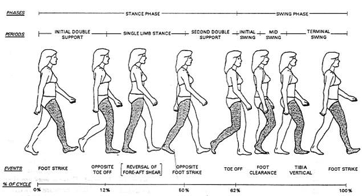
[[Gait Cycle|Gait]] is made up of repetitive cycles of the stance phase when the foot is on the ground (foot strike, mid stance, and terminal stance) and the swing phase when the foot is in the air. When running, there is an additional phase: the float phase when both feet are off the ground. | |||
* During walking, In foot strike, the foot is supinated, and Chopart joint is locked, making the foot rigid when the heel first lands. | |||
* The foot pronates and flattens during mid-stance as it comes in full contact with the surface. | |||
* Terminal stance is then characterized by propulsion via heel off and toe-off. | |||
* The Lisfranc joint allows slight dorsiflexion and plantarflexion. | |||
* Force is then transferred to the middle column of the forefoot during the toe-off phase of stepping, and the forefoot supinates. | |||
* The lateral column acts during the final phase of push-off while stepping, providing primarily sensory input. | |||
* The base of the fifth metatarsal alone absorbs significant force and weight. | |||
The combination of fixed midfoot, slightly flexible Lisfranc joint, and flexible metatarsophalangeal joints create a lever for propulsion during gait<ref name=":0" />. | |||
== Influence on Kinetic Chain/Gait == | |||
In closed chain | As discussed above with MT joint locking, the transition in the foot from pronation to supination is an important function that assists in adapting to uneven terrain and acting as a rigid lever during push off. | ||
* During pronation, the MT joint unlocks, providing flexibility of the foot and assisting in maintaining balance. | |||
* During supination, the MT joint locks, providing rigidity of the foot and maximizing stability. | |||
If the foot remains pronated, it would lead to hypermobility of the midfoot and place greater demand on the neuromuscular structures that stabilize the foot and maintain upright stance. Whereas if the foot remains supinated, the midfoot would be hypomobile, which would compromise the ability of the foot to adjust to the terrain and increase demand on surrounding structures to maintain postural stability and balance. Cote et al.<ref name="p3">Cote KP, Brunet II ME, Gansneder BM, Shultz SJ. Effects of pronated and supinated foot postures on static and dynamic postural stability. Journal of athletic training. 2005 Jan 1;40(1):41.</ref> concluded that postural stability is affected by foot position in both static and dynamic conditions. Chain reactions occur secondary to the positioning of the foot. <br> | |||
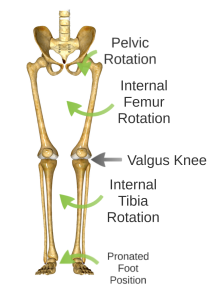
In closed chain movements, the following kinetic chain reaction takes place in an over-pronated foot:[[Image:Kinetic chain.png|right]] | |||
*Calcaneal eversion | *Calcaneal eversion | ||
| Line 261: | Line 304: | ||
*Anterior tilting of pelvis | *Anterior tilting of pelvis | ||
In closed chain movement following kinetic chain reaction | In closed chain movement the following kinetic chain reaction takes place in an over-supinated foot: | ||
*Calcaneal inversion | *Calcaneal inversion | ||
| Line 269: | Line 312: | ||
*Varus at knee | *Varus at knee | ||
*Lateral rotation of femur | *Lateral rotation of femur | ||
*Posterior tilting of pelvis | *Posterior tilting of pelvis | ||
[[ | == Arches of Foot == | ||
[[File:Arches_of_foot.jpg|right|frameless|650x650px]]The arches of the foot provide functions of force absorption, base of support and acts as a rigid lever during gait propulsion. | |||
The medial longitudinal arch, lateral longitudinal arch and transverse arch are the 3 arches that compromise arches of foot. | |||
=== Medial Longitudinal Arch (MLA) === | |||
It is the longest and highest of all the arches. Bony components of MLA include the calcaneus, talus, navicular, the three cuneiform bones and the first 3 metatarsals. The arch consists of two pillars: the anterior and posterior pillars. The anterior pillar consists of the head of first 3 metatarsal heads and the posterior pillar consists of the tuberosity of the calcaneus. The plantar aponeurosis forms the supporting beam connecting the two pillars<ref name="p1" />. The apex of the MLA is the superior articular surface of talus. In addition to the plantar aponeurosis the MLA is also supported by the [[Spring Ligament|spring ligament]] and the deltoid ligament. The [[Tibialis Anterior|Tibialis anterior]] and [[Tibialis Posterior|posterior]] muscles play an important role in raising the medial border of the arch, whereas [[Flexor hallucis longus]] acts as bowstring. <br> | |||
=== Lateral Longitudinal Arch (LLA) === | |||
It is the lowest arch and comprises of the calcaneus, cuboid, fourth & fifth metatarsal as its bony component. Like the Medial Longitudinal Arch (MLA) the posterior pillar consists of the tuberosity of the calcaneus. The anterior pillar is formed by the metatarsal heads of 4th and 5th metatarsals. The plantar aponeurosis, long & short plantar ligaments provides support to the LLA. The [[Peroneus longus and brevis tests|Peroneus longus]] tendon plays an important role in maintaining the lateral border of the arch. | |||
=== Transverse Arch === | |||
It is concave in non-weight bearing and runs medial to lateral in the midtarsal and tarsometatarsal area. The bony component of the arch consists of the metatarsal heads, cuboids and 3 cuneiform bones. The medial and lateral pillars of the arch is formed by the medial and lateral longitudinal arch respectively. The arch is maintained by the Posterior tibialis tendon and the Peroneus longus tendon which cross the plantar surface from medial to lateral and lateral to medial respectively.<br> | |||
''' | === '''Windlass Mechanism of the Foot''' === | ||
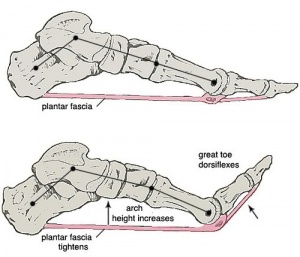
[[File:Windlass.jpg|right|frameless|300x300px]] | |||
The plantar aponeurosis acts similarly to a windlass mechanism. A [[Windlass Test|windlass]] is typically a horizontal cylinder that rotates with a crank or belt on a chain or rope to pull heavy objects. The common use of a windlass is in pulling the anchor of the ship known as an anchor windlass. This mechanism can be seen in the foot. When the MTP joints are hyperextended, the plantar aponeurosis becomes taut as it is wrapped around the MTP joints. This actions brings the metatarsal and tarsal bones together converting it into a rigid structure and eventually rising the longitudinal arches. This function is important in providing a rigid lever for gait propulsion during push off. | |||
== Function of the Foot == | |||
The foot requires sufficient mobility and stability for all of its functions. Mobility is necessary for absorbing the ground reaction force of the body.<ref name="p0" /> Subtalar pronation has a shock absorbing effect during initial heel contact.<ref name="p0" /><ref name="p1" /><ref name="Langer">Langer PS, et al. A practical manual of clinical electrodynography. 2nd ed. Deer Park: The Langer Foundation for Biomechanics and Sports Medicine Research, 1989.</ref><ref name="p3" /> Pronation is also necessary to enable rotation of the leg and to absorb the impact of this rotation. Subtalar pronation plays a role in shock absorption through eccentric control of the supinators.<ref name="p0" /> On the other side, the joint of Chopart becomes unlocked so that the forefoot can stay loose and flexible.<ref name="p1" /> In midstance, the foot needs mobility to adapt to variation in surfaces.<ref name="p0" /><ref name="p1" /><ref name="Langer" /><ref name="p3" /> | |||
Foot stability is necessary to provide a stable base for the body. The foot needs the capacity to bear body weight and act as a stable lever to propel the body forward.<ref name="p0" /><ref name="p1" /><ref name="Langer" /><ref name="p3" /> This function requires pronation control of the subtalar joint.<ref name="p1" /><ref name="Langer" /><ref name="p3" /> | |||
Normal foot function provides the foot with the capacity to transform at the right time from a mobile adapter to a rigid lever. The foot needs sufficient mobility to move into all the positions of the gait cycle while maintaining mobility and stability.<ref name="p4" /><ref name="p0" /> Physiological mobility is essential; if mobility was too large, the foot would not have the capacity to be stable. When this condition is fulfilled, the joint can support standing in the stable maximally close packed position.<ref name="p0" /><ref name="p1" /> When the normal transition of the two functions isn’t normal, many overload injuries can be observed in the foot, leg but also in the lower back.<ref name="p1" /><ref name="Langer" /><ref name="p3" /> Therefore the three phases of ground contact have to fall in the normal time interval, otherwise some compensation mechanisms (example: genu recurvatum in cases of reduced dorsiflexion) will be used, which cause overuse syndromes.<ref name="p1" /><ref name="DD">Den Dekker JB, et al. Jaarboek 1991 Fysiotherapie Kinesitherapie, 1st ed, Houten/Zwaventem, Bohn Stafleu Van Longhum,1993. (201-241)</ref> (Example: [[Chondromalacia Patellae|chondromalacia]], [[Medial Tibial Stress Syndrome|shin-splints]]) | |||
In the transition from midstance to propulsion phase, the mechanisms often fail. The transition from eversion to inversion is facilitated by the tibialis posterior muscle.<ref name="p0" /> The muscle is stretched like a spring and potential energy is stored.<ref name="p0" /> At the end of the midstance, the muscle passes from eccentric to concentric work and the energy is released. The tibialis posterior muscle then causes abduction and dorsiflexion of the caput tali in which the hindquarter is everted.<ref name="p0" /> At the same time, the peroneus longus muscle, at the end of the midstance, will draw the forefoot with a plantar flexion of the first toe.<ref name="p0" /> This is how the forefoot becomes stable.<ref name="p0" /> | |||
< | |||
When the forefoot moves in the propulsion phase, the [[Windlass Test|windlass phenomena]] starts. When the dorsiflexion of the metatarsophalangeal joints begins, the plantar fascia undergoes stress.The calcaneus becomes vertical and teared in inversion. Like this, the hindquarter rests in inversion in the unwinding of the forefoot.<ref name="p0" /> | |||
[[ | |||
When there are some abnormalities in the normal gait cycle of functions of the body, some functional orthosis can be used.<ref name="p1" /><ref name="Langer" /><ref name="p3" /> This orthosis have the capacity to correct the biomechanical function of the foot.<ref name="p1" /><ref name="Langer" /><ref name="p3" /> In contrast, insoles only support the arch of the foot. Reduced or limited mobility in the lower limbs can be caused by a articular limitation.<ref name="p1" /><ref name="Langer" /><ref name="p3" /> In these cases some classic mobilizations or mobilizations according to manual therapy can be applied.<ref name="p1" /><ref name="Langer" /><ref name="p3" /> When the cause is a muscle shortening some stretching can be prescribed. Also, good (running) shoes are indicated.<ref name="Shepard">Shephard R.J. and Taunton J.E., Foot and Ankle in Sport and exercise, Basel, 1987. (p.30-38).</ref> | |||
==References== | |||
<references /><br> | |||
<br> | |||
[[Category:Biomechanics]] | |||
[[Category:Anatomy]] | |||
[[Category:Ankle - Anatomy]] | |||
[[Category:Foot - Anatomy]] | |||
[[Category:Foot]] | |||
[[Category:Ankle]] | |||
[[Category:Ankle - Joints]] | |||
[[Category:Foot - Joints]] | |||
[[Category:Foot - Arches]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Sports Medicine]] | |||
Latest revision as of 23:29, 30 March 2023
Original Editor - Vinit Kothekar
Top Contributors - Vinit Kothekar, Wanda van Niekerk, Kim Jackson, Admin, Evan Thomas, Lucinda hampton, Chelsea Mclene, Candace Goh, Rachael Lowe, Simisola Ajeyalemi, WikiSysop, Rucha Gadgil, Jess Bell, Khloud Shreif, 127.0.0.1, Ewa Jaraczewska, Cath Young and Priyanka Chugh
Anatomy[edit | edit source]
The foot and ankle form a complex system which consists of 28 bones, 33 joints, 112 ligaments, controlled by 13 extrinsic and 21 intrinsic muscles.
The foot is subdivided into the rearfoot, midfoot, and forefoot.
It functions as a rigid structure for weight bearing and it can also function as a flexible structure to conform to uneven terrain. The foot and ankle provide various important functions which includes:
- Supporting body weight.
- Providing balance.
- Shock absorption.
- Transferring ground reaction forces.
- Compensating for proximal malalignment.
- Substituting hand function in individuals with upper extremity amputation/paralysis.[1]
| [2] | [3] |
Structure[edit | edit source]
The ankle or tibiotalar joint constitutes the junction of the lower leg and foot. The osseous components of the ankle joint include the distal tibia, distal fibula, and talus.
The anatomic structures below the ankle joint comprise the foot, which includes:
- Hindfoot: Hindfoot, the most posterior aspect of the foot, is composed of the talus and calcaneus, two of the seven tarsal bones. The talus and calcaneus articulation is referred to as the subtalar joint, which has three facets on each of the talus and calcaneus.
- Midfoot: The midfoot is made up of five of the seven tarsal bones: navicular, cuboid, and medial, middle, and lateral cuneiforms. The junction between the hind and midfoot is termed the Chopart's joint, which includes the talonavicular and calcaneocuboid joints.
- Forefoot: The forefoot is the most anterior aspect of the foot. It includes metatarsals, phalanges (toes), and sesamoid bones. There are a metatarsal and three phalanges for each digit apart from the great toe, which only has two phalanges. The articulation of the midfoot and forefoot forms the Lisfranc joint.[4]
Talocrural (TC) Joint[edit | edit source]
The talocrural joint is formed between the distal tibia-fibula and the talus, and is commonly known as the ankle joint. The distal and inferior aspect of the tibia – known as the plafond – is connected to the fibula via tibiofibular ligaments forming a strong mortise which articulates with the talar dome distally. It is a hinge joint and allows for dorsiflexion and plantarflexion movements in the sagittal plane.
Subtalar (ST) Joint[edit | edit source]
It is also known as the talocalcaneal joint and is formed between the talus and calcaneus.
- There are three facets on each of the talus and calcaneus.
- The posterior subtalar joint constitutes the largest component of the subtalar joint.
- The subtalar joint allows inversion and eversion of ankle and hindfoot.[4]
Midtarsal (MT) Joint[edit | edit source]
Also known as transverse tarsal joints or Chopart’s joint. It is an S-shaped joint when viewed from above. It consists of two joints – the Talonavicular Joint and Calcaneocuboid Joint.
- Talonavicular (TN) Joint - Formed between the anterior talar head and the concavity on the navicular. It does not have its own capsule, but rather shares one with the two anterior talocalcaneal articulations.
- Calcaneocuboid (CC) Joint - Formed between the anterior facet of the calcaneus and the posterior cuboid. Both articulating surface, present a convex and concave surface with the joint being convex vertically and concave transversely. Very little movement occurs at this joint.
Tarsometatarsal (TMT) Joint Complex[edit | edit source]
Also known as Lisfranc’s joint. This complex divides the midfoot from forefoot.
The distal tarsal rows including the three cuneiform bones and cuboid articulate with the base of each metatarsal to form the TMT complex. It is an S-shaped joint and is divided into 3 distinct columns[1]:
- Medial – composed of 1st metatarsal and medial cuneiform.
- Middle – composed of 2nd and 3rd metatarsals, intermediate and lateral cuneiforms respectively.
- Lateral – composed of 4th and 5th metatarsals and the cuboid.
Metatarsophalangeal (MTP) Joints and Interphalangeal (IP) Joints[edit | edit source]
The MTP joints are formed between the metatarsal heads and the corresponding bases of the proximal phalanx. The interphalangeal joints of the toes are formed between the phalanges of the toes. Each toe has proximal and distal IP joints except for the great toe which only has one IP joint.
| Joint | Type of Joint | Plane of Movement | Motion |
|---|---|---|---|
| TC joint | Hinge | Sagittal | Dorsiflexion & Plantarflexion |
| ST joint | Condyloid |
Mainly transverse Some sagittal |
Inversion & Eversion Dorsiflexion & Plantarflexion |
| MT joint |
TN joint - Ball and socket CC joint - Modified saddle |
Largely in transverse Some sagittal |
Inversion & Eversion Flexion & Extension |
| TMT joint | Planar | ||
| MTP joint | Condyloid |
Sagittal Some Transverse |
Flexion & Extension Abduction & Adduction |
| IP joint | Hinge | Sagittal | Flexion & Extension |
Kinematics[edit | edit source]
Talocrural Joint[edit | edit source]
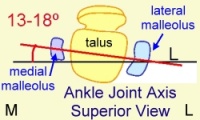
The tip of the medial malleoli is anterior and superior to the lateral malleoli, which makes its axis oblique to both the sagittal and frontal planes. The axis of rotation is approximately 13°-18° laterally from the frontal plane and at angle of 8°-10° from the transverse plane.[1][6] Motion in other planes is required (like horizontal and frontal plane) to achieve a complete motion for plantarflexion and dorsiflexion.[7] The reported normal available range for dorsiflexion varies in the literature between 0°-16.5°[8] and 0°-25°,[9] and this changes with weightbearing. The normal range of plantarflexion has been reported to be around 0°- 50°.
Subtalar Joint[edit | edit source]
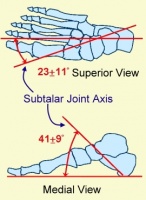
The axis of the subtalar joint lies about 42° superiorly to the sagittal plane and about 16° to 23° medial to the transverse plane.[10][11] The literature presents vast ranges of subtalar motion ranging from 5° to 65°.[11] The average ROM for pronation is 5° and 20° for supination. Inversion and eversion ROM has been identified as 30° and 18°, respectively.[12] Total inversion-eversion motion is about 2:1 and a 3:2 ratio of inversion-to-eversion movement.[7]
Midtarsal Joint[edit | edit source]
The Midtarsal joint rotates at two axes due to its anatomy, making its motion complex. The longitudinal axis (image 'A' below) lies about 15° superior to the horizontal plane and about 10° medial to the longitudinal plane. The oblique axis (image 'B' below) lies about 52° superior to the horizontal plane and 57° from the midline. The longitudinal axis is close to the subtalar joint axis and the oblique axis is similar to the talocrural joint axis.
MT Joint Locking[edit | edit source]
An important function of the foot is propulsion of weight during stance phase[13]. This function is made possible by the MT joint locking and unlocking. During heel strike, the foot needs to be flexible in order to adjust to the surface and the MT joint unlocks to provide this flexibility. Later in the gait cycle, the foot then needs to act as a rigid lever to propel the weight of the body forward which is made possible by MT joint locking. During pronation/eversion of the foot, the axis of the TN and CC joints are parallel to each other, making it easier for them to independently move and unlock the MT joint. The axes cross each other during supination/inversion and locks the MT joint making it difficult to move. Blackwood et al[14] concluded that there is increased forefoot movement when the calcaneus is everted. This is consistent with the MT joint locking mechanism.
Lisfranc Joint Complex[edit | edit source]
The degree of sagittal motion for each TMT joint is presented below[7]
| TMT Joint | Degree of Motion |
| 1st | 1.6o |
| 2nd | 0.6o |
| 3rd | 3.5o |
| 4th | 9.6o |
| 5th | 10.2o |
MTP and IP joints[edit | edit source]
The MTP joints are bi-axial and move in sagittal and transverse planes. MTP joints have a greater sagittal plane movement and very little transverse plane movement. At MTP joints, hyperextension is about 90° and flexion is about 30° to 50°. IP joints are hinge joints which limit motion in one direction.
Arthrokinematics[edit | edit source]
Arthrokinematics refers to the movement of joint surfaces.
- Talocrural Joint – The talus rolls within the mortise during dorsiflexion and plantarflexion. During dorsiflexion, the talus rolls anteriorly and it glides posteriorly. While with plantarflexion, the talus rolls posteriorly and glides anteriorly.
- Subtalar Joint – Secondary to the anatomy of the subtalar joint, the coupled motion of dorsiflexion, abduction and eversion produces pronation, whereas the coupled motion of plantarflexion, adduction and inversion produces supination. It presents two point of articulations – anterior talocalcaneal articulation and posterior talocalcaneal articulation.[16] During open kinetic chain inversion, the calcaneus rolls into inversion and it glides/slides laterally. And during eversion, the calcaneus rolls into eversion and it glides/slides medially.
- Midtarsal Joint – For the Talonavicular joint, the concave navicular moves on the convex talus and hence the roll and glide is in the same direction of movement. The calcaneocuboid joint is a saddle joint so the direction changes depending on the movement. During flexion-extension, the cuboid is concave and the calcaneus is convex; Hence, the roll and glide occurs in the same direction as the talonavicular joint. During abduction-adduction, however, the cuboid is convex and the calcaneus is concave, and therefore the roll and glide occurs in the opposite direction.
- Lisfranc Joint – Secondary to the bony and ligamentous anatomy of the complex, the primary role is stability of the midfoot as it has very little movement. It has three distinct arches and the main stabilizing structure of TMT joint is a Y-shaped ligament known as Lisfranc’s ligament.
- MTP and IP Joints – Glide and roll is in the same direction as the movement for the MTP joints, as the concave base of the phalanx moves on the convex head of the metatarsal. The same is true for the IP joints, where glide and roll is in the same direction, as the concave distal phalanx moves on the convex proximal phalanx.
| Joint | Closed-Packed Position | Open-Packed Position | Capsular Pattern | Concave Surface | Convex Surface |
Concave-convex rule Roll & glide |
|---|---|---|---|---|---|---|
| Talocrural joint | Full dorsiflexion | 10o of plantarflexion and midway between pronation and supination | Limitation of plantarflexion, although clinically dorsiflexion.
Limitation is more common. |
Proximal - Mortise formed by Tibia, tibiofibular ligament and fibula | Distal - Trochlear surface of Talar dome | Opposite direction |
| Subtalar joint | Full inversion | Inversion/plantarflexion | Limitation of inversion in chronic arthritis. Limitation of eversion in traumatic. | Proximal - Anterior, middle and posterior facet of talus | Distal – Calcaneal Anterior, middle and posterior talar articular surface | Opposite direction |
| Talonavicular joint | Full supination | Midway between extreme ROM | Limitation of dorsiflexion, plantarflexion, adduction and internal rotation. | Proximal - Head of Talus | Distal - Concavity on Navicular bone for talus | Same direction |
| Calcaneocuboid joint | Full supination | Midway between extreme ROM | Limitation of dorsiflexion, plantarflexion, adduction and internal rotation. | Distal - Cuboid is concave during flexion-extension. Calcaneus is concave during adduction-abduction. |
Proximal - Calcaneus is convex during flexion-extension. Cuboid is convex during adduction-abduction. |
Flexion-extension = Same direction |
| Lisfranc joint | Full supination | Midway between supination and pronation | ||||
| 1st MTP joint | Hyperextension | Slight (10o) extension | Loss of motion more in extension than flexion. | Distal - Base of phalanx | Proxmial - Head of Metatarsal | Same direction |
| 2nd to 5th MTP joint | Maximum flexion | Slight (10o) extension | Loss of flexion. | Distal - Base of phalanges | Proximal - Head of metatarsals | Same direction |
| Interphalangeal Joint | Full extension | Slight flexion | Restriction in all direction with more in extension. | Distal Phalanx | Proximal Phalanx | Same direction |
Gait and the Foot[edit | edit source]
Gait is made up of repetitive cycles of the stance phase when the foot is on the ground (foot strike, mid stance, and terminal stance) and the swing phase when the foot is in the air. When running, there is an additional phase: the float phase when both feet are off the ground.
- During walking, In foot strike, the foot is supinated, and Chopart joint is locked, making the foot rigid when the heel first lands.
- The foot pronates and flattens during mid-stance as it comes in full contact with the surface.
- Terminal stance is then characterized by propulsion via heel off and toe-off.
- The Lisfranc joint allows slight dorsiflexion and plantarflexion.
- Force is then transferred to the middle column of the forefoot during the toe-off phase of stepping, and the forefoot supinates.
- The lateral column acts during the final phase of push-off while stepping, providing primarily sensory input.
- The base of the fifth metatarsal alone absorbs significant force and weight.
The combination of fixed midfoot, slightly flexible Lisfranc joint, and flexible metatarsophalangeal joints create a lever for propulsion during gait[4].
Influence on Kinetic Chain/Gait[edit | edit source]
As discussed above with MT joint locking, the transition in the foot from pronation to supination is an important function that assists in adapting to uneven terrain and acting as a rigid lever during push off.
- During pronation, the MT joint unlocks, providing flexibility of the foot and assisting in maintaining balance.
- During supination, the MT joint locks, providing rigidity of the foot and maximizing stability.
If the foot remains pronated, it would lead to hypermobility of the midfoot and place greater demand on the neuromuscular structures that stabilize the foot and maintain upright stance. Whereas if the foot remains supinated, the midfoot would be hypomobile, which would compromise the ability of the foot to adjust to the terrain and increase demand on surrounding structures to maintain postural stability and balance. Cote et al.[17] concluded that postural stability is affected by foot position in both static and dynamic conditions. Chain reactions occur secondary to the positioning of the foot.
In closed chain movements, the following kinetic chain reaction takes place in an over-pronated foot:
- Calcaneal eversion
- Adduction and plantarflexion of talus
- Medial rotation of talus
- Medial rotation of tibia and fibula
- Valgus at knee
- Medial rotation of femur
- Anterior tilting of pelvis
In closed chain movement the following kinetic chain reaction takes place in an over-supinated foot:
- Calcaneal inversion
- Abduction and dorsiflexion of talus
- Lateral rotation of talus
- Lateral rotation of tibia and fibula
- Varus at knee
- Lateral rotation of femur
- Posterior tilting of pelvis
Arches of Foot[edit | edit source]
The arches of the foot provide functions of force absorption, base of support and acts as a rigid lever during gait propulsion.
The medial longitudinal arch, lateral longitudinal arch and transverse arch are the 3 arches that compromise arches of foot.
Medial Longitudinal Arch (MLA)[edit | edit source]
It is the longest and highest of all the arches. Bony components of MLA include the calcaneus, talus, navicular, the three cuneiform bones and the first 3 metatarsals. The arch consists of two pillars: the anterior and posterior pillars. The anterior pillar consists of the head of first 3 metatarsal heads and the posterior pillar consists of the tuberosity of the calcaneus. The plantar aponeurosis forms the supporting beam connecting the two pillars[1]. The apex of the MLA is the superior articular surface of talus. In addition to the plantar aponeurosis the MLA is also supported by the spring ligament and the deltoid ligament. The Tibialis anterior and posterior muscles play an important role in raising the medial border of the arch, whereas Flexor hallucis longus acts as bowstring.
Lateral Longitudinal Arch (LLA)[edit | edit source]
It is the lowest arch and comprises of the calcaneus, cuboid, fourth & fifth metatarsal as its bony component. Like the Medial Longitudinal Arch (MLA) the posterior pillar consists of the tuberosity of the calcaneus. The anterior pillar is formed by the metatarsal heads of 4th and 5th metatarsals. The plantar aponeurosis, long & short plantar ligaments provides support to the LLA. The Peroneus longus tendon plays an important role in maintaining the lateral border of the arch.
Transverse Arch[edit | edit source]
It is concave in non-weight bearing and runs medial to lateral in the midtarsal and tarsometatarsal area. The bony component of the arch consists of the metatarsal heads, cuboids and 3 cuneiform bones. The medial and lateral pillars of the arch is formed by the medial and lateral longitudinal arch respectively. The arch is maintained by the Posterior tibialis tendon and the Peroneus longus tendon which cross the plantar surface from medial to lateral and lateral to medial respectively.
Windlass Mechanism of the Foot[edit | edit source]
The plantar aponeurosis acts similarly to a windlass mechanism. A windlass is typically a horizontal cylinder that rotates with a crank or belt on a chain or rope to pull heavy objects. The common use of a windlass is in pulling the anchor of the ship known as an anchor windlass. This mechanism can be seen in the foot. When the MTP joints are hyperextended, the plantar aponeurosis becomes taut as it is wrapped around the MTP joints. This actions brings the metatarsal and tarsal bones together converting it into a rigid structure and eventually rising the longitudinal arches. This function is important in providing a rigid lever for gait propulsion during push off.
Function of the Foot[edit | edit source]
The foot requires sufficient mobility and stability for all of its functions. Mobility is necessary for absorbing the ground reaction force of the body.[13] Subtalar pronation has a shock absorbing effect during initial heel contact.[13][1][18][17] Pronation is also necessary to enable rotation of the leg and to absorb the impact of this rotation. Subtalar pronation plays a role in shock absorption through eccentric control of the supinators.[13] On the other side, the joint of Chopart becomes unlocked so that the forefoot can stay loose and flexible.[1] In midstance, the foot needs mobility to adapt to variation in surfaces.[13][1][18][17]
Foot stability is necessary to provide a stable base for the body. The foot needs the capacity to bear body weight and act as a stable lever to propel the body forward.[13][1][18][17] This function requires pronation control of the subtalar joint.[1][18][17]
Normal foot function provides the foot with the capacity to transform at the right time from a mobile adapter to a rigid lever. The foot needs sufficient mobility to move into all the positions of the gait cycle while maintaining mobility and stability.[10][13] Physiological mobility is essential; if mobility was too large, the foot would not have the capacity to be stable. When this condition is fulfilled, the joint can support standing in the stable maximally close packed position.[13][1] When the normal transition of the two functions isn’t normal, many overload injuries can be observed in the foot, leg but also in the lower back.[1][18][17] Therefore the three phases of ground contact have to fall in the normal time interval, otherwise some compensation mechanisms (example: genu recurvatum in cases of reduced dorsiflexion) will be used, which cause overuse syndromes.[1][19] (Example: chondromalacia, shin-splints)
In the transition from midstance to propulsion phase, the mechanisms often fail. The transition from eversion to inversion is facilitated by the tibialis posterior muscle.[13] The muscle is stretched like a spring and potential energy is stored.[13] At the end of the midstance, the muscle passes from eccentric to concentric work and the energy is released. The tibialis posterior muscle then causes abduction and dorsiflexion of the caput tali in which the hindquarter is everted.[13] At the same time, the peroneus longus muscle, at the end of the midstance, will draw the forefoot with a plantar flexion of the first toe.[13] This is how the forefoot becomes stable.[13]
When the forefoot moves in the propulsion phase, the windlass phenomena starts. When the dorsiflexion of the metatarsophalangeal joints begins, the plantar fascia undergoes stress.The calcaneus becomes vertical and teared in inversion. Like this, the hindquarter rests in inversion in the unwinding of the forefoot.[13]
When there are some abnormalities in the normal gait cycle of functions of the body, some functional orthosis can be used.[1][18][17] This orthosis have the capacity to correct the biomechanical function of the foot.[1][18][17] In contrast, insoles only support the arch of the foot. Reduced or limited mobility in the lower limbs can be caused by a articular limitation.[1][18][17] In these cases some classic mobilizations or mobilizations according to manual therapy can be applied.[1][18][17] When the cause is a muscle shortening some stretching can be prescribed. Also, good (running) shoes are indicated.[20]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 Houglum PA, Bertoti DB. Brunnstrom's clinical kinesiology. FA Davis; 2012
- ↑ Anatomy Zone. Ankle Joint - 3D Anatomy Tutorial. Available from: https://www.youtube.com/watch?v=lPLdoFQlZXQ [last accessed 19/03/2015]
- ↑ AnimatedBiomedical. Ankle Joint, Bones of the Foot - 3D Medical Animation. Available from: https://www.youtube.com/watch?v=X-eAXKS4pJM [last accessed 19/03/2015]
- ↑ 4.0 4.1 4.2 Ficke J, Byerly DW. Anatomy, Bony Pelvis and Lower Limb, Foot. InStatPearls [Internet] 2019 Sep 3. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK546698/#_article-21883_s2_ ( last accessed 11.3.2020)
- ↑ Dr Glass DPM.Ankle & Subtalar Joint Motion Function Explained Biomechanic of the Foot - Pronation & Supination. Published on 21 January 2008. Available from https://www.youtube.com/watch?v=0R4zRSE_-40&t=29s (last accessed 10 June 2019)
- ↑ http://www.pt.ntu.edu.tw/hmchai/Kinesiology/KINlower/Ankle.htm#Kinematics
- ↑ 7.0 7.1 7.2 Lundberg A, Goldie I, Kalin B, Selvik G. Kinematics of the ankle/foot complex: Plantarflexion and dorsiflexion. Foot and Ankle 9(4):194–200, 1989.
- ↑ Baggett BD, Young G. Ankle joint dorsiflexion. Establishment of a normal range. Journal of the American Podiatric Medical Association. 1993 May;83(5):251-4.
- ↑ CDCP. Normal joint range of motion study. Acceessed https://www.cdc.gov/ncbddd/jointrom/
- ↑ 10.0 10.1 http://www.wheelessonline.com/ortho/Sub_talar_joint
- ↑ 11.0 11.1 Stagni R, Leardini A, O'Connor JJ, Giannini S. Role of passive structures in the mobility and stability of the human subtalar joint: a literature review. Foot andankle international. 2003 May 1;24(5):402-9.
- ↑ Ball P, Johnson GR. Technique for the measurement of hindfoot inversion and eversion and its use to study a normal population. Clinical Biomechanics 11(3):165–169, 1996
- ↑ 13.00 13.01 13.02 13.03 13.04 13.05 13.06 13.07 13.08 13.09 13.10 13.11 13.12 13.13 http://www.amputation.research.va.gov/limb_loss_prevention/Midtarsal_Joint_Locking.asp
- ↑ Blackwood CB, Yuen TJ, Sangeorzan BJ, Ledoux WR. The midtarsal joint locking mechanism. Foot and ankle international. 2005 Dec 1;26(12):1074-80
- ↑ Jacqueline Buchman. Midtarsal Joint Oblique Axis. Available from https://www.youtube.com/watch?v=h9OzIw2XCSY (last accessed 30.03.2023)
- ↑ https://en.wikipedia.org/wiki/Subtalar_joint
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 17.8 17.9 Cote KP, Brunet II ME, Gansneder BM, Shultz SJ. Effects of pronated and supinated foot postures on static and dynamic postural stability. Journal of athletic training. 2005 Jan 1;40(1):41.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 18.6 18.7 18.8 Langer PS, et al. A practical manual of clinical electrodynography. 2nd ed. Deer Park: The Langer Foundation for Biomechanics and Sports Medicine Research, 1989.
- ↑ Den Dekker JB, et al. Jaarboek 1991 Fysiotherapie Kinesitherapie, 1st ed, Houten/Zwaventem, Bohn Stafleu Van Longhum,1993. (201-241)
- ↑ Shephard R.J. and Taunton J.E., Foot and Ankle in Sport and exercise, Basel, 1987. (p.30-38).