Fibromyalgia: Difference between revisions
No edit summary |
Kapil Narale (talk | contribs) No edit summary |
||
| (90 intermediate revisions by 16 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- | '''Original Editors ''' - [[Pathophysiology of Complex Patient Problems|Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == <b>Definition/Description</b> == | ||
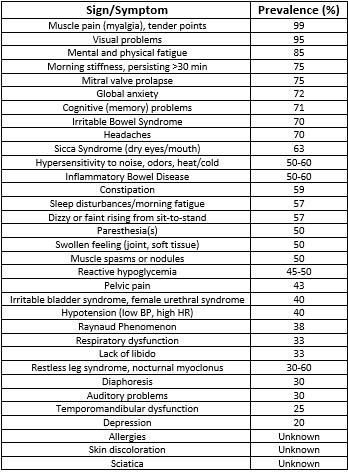
[[File:Fibromyalgia Pain Chart.JPG|right|frameless]] | |||
'''Fibromyalgia Syndrome''' '''(FMS)''' is a disease characterized by [https://www.physio-pedia.com/Chronic_Pain?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal chronic pain], stiffness, and tenderness of [[Muscle|muscles]], [[Tendon Anatomy|tendons]], and [[Joint Classification|joints]], without detectable [[Inflammation Acute and Chronic|inflammation]]. Fibromyalgia does not cause body damage or deformity. Fatigue affects 90 percent of patients, and sleep disorders are common. Fibromyalgia can be associated with other rheumatic conditions, and [[Irritable Bowel Syndrome|irritable bowel syndrome (IBS)]]. There is no definitive medical test for the diagnosis of fibromyalgia. Fibromyalgia symptoms can occur and disappear over time. Diagnosis is made by eliminating other possible causes of the symptoms. It can take time to identify which symptoms are caused by which problems <ref>Medicine net. [https://www.medicinenet.com/script/main/art.asp?articlekey=3453 Medical definition of fibromyalgia] Available from: https://www.medicinenet.com/script/main/art.asp?articlekey=3453 (last accessed 6.10.19)</ref>. FMS is NOT just one condition; it's a complex syndrome involving many different factors that can severely impact and disrupt a person’s daily life. | |||
FMS is considered a systemic problem involving biochemical, neuroendocrine, and physiologic abnormalities, leading to a disorder of pain processing and perception (i.e. [[allodynia]], hyperalgesia). The symptoms associated with FMS may originate from primary or secondary/reactive causes. <ref name="p1">Goodman, Catherine and Fuller Kendra. Pathology: Implications for the Physical Therapist. Philadelphia, WB Saunders. 4th edition (Goodman & Fuller), 2014. (pp. 310-317)</ref> As fibromyalgia encompasses persistent pain in various areas, without any evidence of tissue damage, it is classified as [[Nociplastic Pain|nociplastic pain]]. <ref>International Association for the Study of Pain - What's in a Name for Chronic Pain? “Nociplastic pain” was officially adopted by IASP as the third mechanistic descriptor of chronic pain. Available from: <nowiki>https://www.iasp-pain.org/publications/pain-research-forum/prf-news/92059-whats-name-chronic-pain/</nowiki> (accessed 11 August 2023).</ref> | |||
The most effective treatment is a combination of education, stress reduction, exercise, and medication. | |||
Here is a thorough video from Dr. Andrea Furlan, with an explanation of Fibromyalgia: <ref>Dr. Andrea Furlan. Fibromyalgia by Dr. Andrea Furlan MD, PhD. Available from: https://www.youtube.com/watch?v=_1B8U-eEkE0&t=53s&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023). </ref> | |||
{{#ev:youtube|_1B8U-eEkE0}} | |||
== <b>Prevalence</b> == | |||
FMS occurs in more than 6 million Americans, or 4% of the population, causing it to be the most common musculoskeletal disorder in the U.S. It mainly effects women (90%) more often than men. Symptoms typically present between the ages of 20-55 years, but individuals have been diagnosed as young as 6 years and as old as 85 years of age.<ref name="p1" /> | |||
== <b>Pathophysiology</b> == | |||
The pathogenesis of FMS is theorised to be a malfunctioning of the [[Central Nervous System Pathways|central nervous system (CNS)]], characterized by central sensitisation, which is a heightened pain perception accompanied by ineffective pain inhibition and/or modulation. This increased response to peripheral stimuli causes hyperalgesia, allodynia, and referred pain across multiple spinal segments, resulting in chronic widespread pain and decreased tolerance to sensory input of the musculoskeletal system. | |||
FMS systemically causes a dysregulation : : neurologic; immunologic; endocrinologic; and enteric organ systems <ref name="p1" />. | |||
'''1. Autonomic Nervous System''' | |||
The [[Autonomic Nervous System|Autonomic Nervous System (ANS)]] is responsible for regulating the [[Sympathetic Nervous System|Sympathetic]] (“fight or flight”) and the [[Parasympathetic System|Parasympathetic]] (“rest and digest”) responses. With FMS, patients experience a systemically heightened sympathetic (SNS) response with a diminished parasympathetic (PNS) modulation. Continuous over activation of the SNS results in increased heart rate, excessive gastric secretions and contractions, abnormalities of smooth muscle contraction throughout the digestive tract, rapid and shallow respiration, and vasoconstriction. This can lead to [[malnutrition]] due to absorption and digestion disruptions. Prolonged inhibition of PNS alters the neuroimmunoendocrine systems, directly affecting growth hormone secretion by the pituitary gland. This can result in nonrestorative sleep, pain, fatigue, and [[Cognitive Impairments|cognitive]]/mood symptoms. <ref name="p1" /> | |||
'''2. Immune System''' | |||
''' | |||
< | The immune response to infection, inflammation, and/or trauma is a release of cytokines for local healing, which trigger the CNS to release glial cells within the brain and [[Spinal cord anatomy|spinal cord]] for healing support and pain response. With FMS, this auto-immune response is heightened, causing an excess of glia in the body, which creates an exaggerated state of pain (chronic).<ref name="p1" /> | ||
=== <b>Causes</b>[[:File:FMS physiologic Effects.png|<nowiki/>]] === | |||
There are many hypotheses of how multiple factors play a role in the development of FMS. The exact etiology of FMS is still being researched; however, there are several potential causes and risk factors, listed below, that are currently associated with, or increase one’s risk for developing this condition<ref name="p1" />. | |||
*Diet | |||
<gallery widths="260" heights="260"> | |||
File:Food Pyramid.gif | |||
</gallery> | |||
*Viral | |||
*Occupation, seasonal, environmental influences | |||
*Adverse childhood experiences (i.e. [[Post-traumatic Stress Disorder|PTSD]]) | |||
*Psychological and cognitive/behavioral factors | |||
*Other conditions: [[Rheumatoid Arthritis|rheumatoid athritis]], [[Systemic Lupus Erythematosus|systemic]] [[Systemic Lupus Erythematosus|lupus]] [[Systemic Lupus Erythematosus|erythematosus]], or [[Ankylosing Spondylitis (Axial Spondyloarthritis)|ankylosing]] [[Ankylosing Spondylitis (Axial Spondyloarthritis)|spondylitis]] [[Ankylosing Spondylitis (Axial Spondyloarthritis)|AS]] | |||
Current research remains inconclusive regarding the genetic or hereditary cause of FMS. A family history of FMS is also a risk factor. | |||
& | == <b>Characteristics/Clinical Presentation</b> == | ||
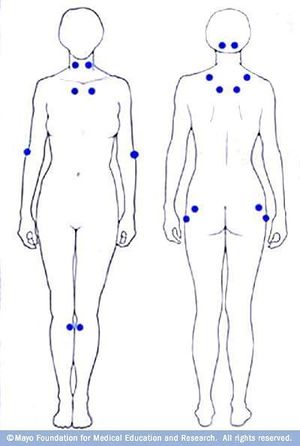
[[Image:FMSSx.png|right]] | |||
Muscle pain is characterised as the major symptom of FMS, often described by patients as “aching or burning” regardless of physical activity. Other symptoms or associated problems occur, with various reports of frequencies, that can also affect function. FMS may cause residual pain sensations at a lower intensity due to repetitive exposure to peripheral stimuli or activity, also known as the “Wind-up Response.” <ref name="p2">Solano C, Martinez A, Martinez-Lavin M, et al. Autonomic dysfunction in fibromyalgia assessed by the Composite Autonomic Symptoms Scale (COMPASS). Journal Of Clinical Rheumatology: Practical Reports On Rheumatic & Musculoskeletal Diseases [serial online]. June 2009;15(4):172-176. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017.</ref><ref name="p1" /> Other symptoms include sleep disturbances, fatigue, and other cognitive and somatic symptoms. <ref>Bair MJ, Krebs EE. Fibromyalgia. Annals of internal medicine. 2020 Mar 3;172(5):ITC33-48. https://sci-hub.hkvisa.net/10.7326/AITC202003030</ref> | |||
| | Symptoms are often exacerbated by: | ||
*[[Stress and Health|Stress]] | |||
*Overloading [[Physical Activity|physical activity]] | |||
*Overstretching | |||
*Damp or chilly weather | |||
*Heat exposure or humidity | |||
*Sudden change in barometric pressure | |||
*Trauma | |||
*Another illness | |||
A recent study carried out by Sempere-Rubio et al found out that functional capacity, upper limb muscular strength, postural maintenance, pain threshold, and anxiety are important predictive factors of [[Quality of Life|Quality of Life (QoL)]] in women with FMS.<ref>Sempere-Rubio N, Aguilar-Rodríguez M, Inglés M, Izquierdo-Alventosa R, Serra-Añó P. Physical Condition Factors that Predict a Better Quality of Life in Women with Fibromyalgia. International journal of environmental research and public health. 2019 Jan;16(17):3173.</ref> | |||
== <sup> </sup><b>Associated Co-morbidities</b> == | |||
Those with FMS are likely to present with several co-morbidities. It is important that a diagnosis of FMS is not overlooked given the presence of additional co-morbidities which would be more commonly diagnosed. Below is a list of common co-morbidities associated with FMS <ref name="p1" />: | |||
[[File:Depression 2.jpg|frameless|257x257px|right]] | |||
*[[Sleep Apnea|Sleep disturbances]] / [[Sleep Apnea|apnea]] | |||
*[[Depression]] | |||
*Anxiety | |||
*[[Post-traumatic Stress Disorder|PTSD]] | |||
*[[Rheumatoid Arthritis|Rheumatoid arthritis]] | |||
*[[Systemic Lupus Erythematosus]] | |||
*[[Ankylosing Spondylitis (Axial Spondyloarthritis)]], | |||
== Fibromyalgia Diagnostic Criteria (2016) == | |||
There is no definitive diagnostic test currently available to determine the presence of FMS. A diagnosis of FMS is generally made based upon the results of a physical examination and ruling out other similar conditions. No special laboratory or radiologic testing is necessary for making a diagnosis; however, some recommended lab tests can be performed in order to rule out other conditions. These tests include: CBC, ESR, basic chemistry (blood urea nitrogen, creatine, hepatic enzymes, serum calcium), thyroid levels (TSH, T3, and T4), and Rheumatoid factor. | |||
Fibromyalgia may now be diagnosed in adults when all of the following criteria are met <ref>Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, Mease PJ, Russell AS, Russell IJ, Walitt B. [https://acrabstracts.org/abstract/2016-revisions-to-the-20102011-fibromyalgia-diagnostic-criteria/ 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria.] InSeminars in arthritis and rheumatism 2016 Dec 1 (Vol. 46, No. 3, pp. 319-329). WB Saunders. Available from: https://acrabstracts.org/abstract/2016-revisions-to-the-20102011-fibromyalgia-diagnostic-criteria/ (last accessed 6.9.2019)</ref>: | |||
* Widespread pain index (WPI) ≥7 and Symptom Severity Scale (SSS) score ≥5 OR WPI 4–6 and SSS score ≥9. | |||
* Generalised pain, defined as pain in at least 4 of 5 regions, is present. | |||
* Symptoms have been present at a similar level for at least 3 months. | |||
* A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses. | |||
Here is a video from Dr. Andrea Furlan on how Doctors diagnose Fibromyalgia: | |||
{{#ev:youtube|aQ7znPfOTW0}} | |||
== Management == | |||
=== Medication === | |||
Active rehabilitative approaches have primacy in management, but drugs can help to control symptoms. There is evidence to support the use of amitriptyline, duloxetine, milnacipran or pregabalin, but pure opioids should be avoided <ref>Kwiatek R. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5662432/ Treatment of fibromyalgia]. Australian prescriber. 2017 Oct;40(5):179. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5662432/ (last accessed 6.10.19)</ref>. | |||
<br> | === Physical Therapy Management & Exercise === | ||
[[File:Yoga pose.jpg|frameless|right]] | |||
Education about the pathophysiology and the neuroscience behind the condition is the most effective method in reducing catastrophising pain symptoms in patients experiencing FMS, according to current research. Simple acknowledgement and explanation of symptoms, and [[Relaxation Techniques|relaxation strategies]] can enhance a patient’s ability to cope with their condition. | |||
*Explanation of disorder | |||
*Reassurance of condition and symptoms | |||
*Activity management - Pacing, self-monitoring, rest breaks, AVOID exacerbations, set [[SMART Goals|realistic activity goals]], etc. | |||
*[[Relaxation Techniques]] - Minimize environmental stress, deep breathing, healthy & active lifestyle habits, adequate sleep, therapeutic massage, etc. | |||
<br> | |||
| |||
{{#ev:youtube|RYZ2BtFjZAg|500|center}}<ref>Jackie Crush Basic Educational Tool for Fibromyalgia Syndrome. Available from https://www.youtube.com/watch?time_continue=6&v=RYZ2BtFjZAg&feature=emb_logo </ref><br>[Example of a Physical Therapist providing a patient with the educational tools to manage their condition and rehabilitation process.] | |||
< | |||
[ | |||
Here is a video with an explanation to exercises for patients with Fibromyalgia, since it is helpful for the condition. There are 3 other videos that follow this video, one on strengthening, low intensity aerobic exercises, and stretching exercises, which are presented in the next section: <ref>Dr. Andrea Furlan. #094 Fibromyalgia: A beginner's guide to start exercising. Available from: https://www.youtube.com/watch?v=eOK_I-5cMHQ&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023).</ref> | |||
{{#ev:youtube|eOK_I-5cMHQ}} | |||
==== Aerobic and Resistance Exercise ==== | |||
According to the Ottawa Panel Evidence-Based Clinical Practice Guidelines (2008), supervised light [[Aerobic Exercise|aerobic exercise]] and [[Strength Training|strength/resistance training]] is highly recommended for the management of patients with chronic pain, such as those with FMS. It has been found to increase their capacity for activity while minimising their symptoms associated with FMS. Specifically, aerobic activity has been shown to improve psychological symptoms associated with [[depression]], cognitive decline, and [[Sleep Deprivation and Sleep Disorders|sleep disturbances]]. Exercise also improves patient’s cellular metabolism and respiratory capacity, increases lean muscle mass and tone, and increases oxygen uptake within the body’s system(s), which ultimately reduces their complaints of chronic pain and fatigue. <ref name="p1" /><ref name="p9">Brosseau L, Wells G, Veilleux L, et al. Ottawa Panel evidence-based clinical practice guidelines for aerobic fitness exercises in the management of fibromyalgia: part 1. Physical Therapy [serial online]. July 2008;88(7):857-871. Available from: CINAHL, Ipswich, MA. Accessed April 4, 2017.</ref> | |||
Here is a video on strengthening exercises: <ref>Dr. Andrea Furlan. #095 Fibromyalgia: Resistance (weight training) exercises to gain power and strength. Available from: https://www.youtube.com/watch?v=XlyUQK-RplI&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023). </ref> | |||
{{#ev:youtube|XlyUQK-RplI}} | |||
Here is a video on gentle aerobic exercises for Fibromyalgia: <ref>Dr. Andrea Furlan. #096 Fibromyalgia: A 20-minute low-intensity (cardio) exercise routine. Available from: https://www.youtube.com/watch?v=Gd1fdRA-ZjA&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023). </ref> | |||
{{#ev:youtube|Gd1fdRA-ZjA}} | |||
== | Here is a video on stretching exercises for Fibromyalgia: <ref>Dr. Andrea Furlan. #097 Fibromyalgia: A 15-miute gentle stretching routine. Available from: https://www.youtube.com/watch?v=YMFES0QpwA8&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023).</ref> | ||
{{#ev:youtube|YMFES0QpwA8}} | |||
==== Manual / Passive Therapy ==== | |||
Some studies support that [[Transcutaneous Electrical Nerve Stimulation (TENS)|TENS]] and joint mobilisations foster the reduction of pain as short-term relief in patients with FMS. Specifically, patients with chronic back pain due to FMS may benefit from spinal manipulations with limited evidence to support this modality. Moderate evidence shows that the use of passive soft tissue manipulation (STM) is helpful with pain regulation. In addition, diffuse chronic pain presentations are less likely to be reliable for medical management with TENS compared to localised pain. Passive therapy should not be the foundation of FMS medical management due to the maladaptive illness beliefs and coping strategies for patients’ pain. <ref name="p0">Skyba DA, Radhakrishnan R, Rohlwing JJ, et al. Joint manipulation reduces hyperalgesia by activation of monoamine receptors but not opioid or GABA receptors in the spinal cord. Pain. 2003;106:159–168.</ref><ref name="p1" /><ref name="p2" /> | |||
Manual lymph drainage therapy and connective tissue massage have also been studied in women with fibromyalgia. Researchers used the [[Fibromyalgia Impact Questionnaire (FIQ)]] and the [[Nottingham Health Profile]] to measure the impact of the treatment. Their research suggests that both manual lymph drainage therapy and connective tissue massage show improvements in both the FIQ and the Nottingham Health Profile. However, there were significantly greater improvements in the group that received manual lymph drainage therapy, suggesting that manual lymphatic drainage therapy may be preferred over connective tissue massage. | |||
==== Aquatic Therapy & Balneotherapy ==== | |||
Recent research has proven that [[Hydrotherapy|aquatic therapy]] is a more tolerable workout for people with FMS pain. The water’s buoyancy allows the patient to maintain active movement without exerting excessive energy and/or increasing pressure on their joints. Furthermore, evidence has shown that aquatic therapy and hydrotherapy help in improving the [[Quality of Life|quality of life]] of those with chronic FMS.<ref name="p4">Wolfe F, Rasker J. The Symptom Intensity Scale, Fibromyalgia, and the Meaning of Fibromyalgia-like Symptoms. Journal Of Rheumatology [serial online]. November 2006;33(11):2291-2299. Available from: CINAHL, Ipswich, MA. Accessed April 2, 2017.</ref><ref name="p3">Wolfe F, Clauw D, Yunus M, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care & Research [serial online]. May 2010;62(5):600-610. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017.</ref> The underlying symptom(s) of fibromyalgia, central hypersensitivity and pain, may be alleviated by the hydrostatic pressure and the effects of soothing temperature on the nerve endings, along with general muscle relaxation.<br>Ideal pool temperature for aquatic therapy sessions are between 84<sup>o</sup> F and 90<sup>o</sup> F | |||
*82<sup>o</sup> F and 84<sup>o</sup> F for the general population | |||
*90<sup>o</sup> F and 94<sup>o</sup> F for people with [[Arthritis|arthritic]] conditions<br> | |||
An exercise-education program showed a small significant improvement in health status in patients with fibromyalgia and chronic widespread pain, compared with education only. Patients with milder symptoms improved most with this treatment. Moreover, it has been shown that thermal mud baths (and other balneotherapy methods) increase plasma levels of beta-endorphins, thus explaining their analgesic and anti-spastic effects, which is particularly important in patients with FMS. <ref name="p3" /><ref name="p4" /><ref name="p2" /><ref name="p1" /><ref name="p9" /> | |||
=== Other Types of Management === | |||
==== Occupational Therapy ==== | |||
Treatment focuses on activity modification principles, such as working at a moderate pace, frequent positional/postural changes, and resting before fatigue sets in. Patients are encouraged to incorporate regulating principles into all areas of life including self-care, work, and leisure. Proper body mechanics and posture related to home management and work activities are evaluated and adjusted per individual.<ref name="p5">Bennett R, Friend R, Jones K, Ward R, Han B, Ross R. The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties. Arthritis Research & Therapy [serial online]. 2009;11(4):R120. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017.</ref> | |||
== | ==== Cognitive Behavioral Therapy ==== | ||
Research performed by Moseley supports the relationship between pain association and beliefs with physical performance. There is evidence that supports the consideration of [[Cognitive Behavioural Therapy|cognitive behavioral therapy (CBT)]] to be implemented in the assessment and plan of care of patients with [[Chronic Pain and the Brain|chronic pain]]. Growing evidence continues to demonstrate that CBT shows improvement in reports of pain, reduces hyperalgesia, and chronic pain-related brain response in FMS.<br>Another study found that behavioral insomnia therapy for patients with FMS may have a promising impact. The study incorporated patient education on sleeping habits and proper sleeping schedules to reduce the bouts of insomnia experienced by those with fibromyalgia. The researchers concluded that patients who received the behavioral therapy experienced improvement in how long they slept and in their general condition compared to other groups. <ref name="p6">Korszun A. Sleep and circadian rhythm disorders in fibromyalgia. Current Rheumatology Reports [serial online]. April 2000;2(2):124-130. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017.</ref><ref name="p7">Moseley GL. Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 2005;51:49–52.</ref><ref name="p8">Meeus M,Nijs J,VanOosterwijck J,etal.Painphysiologyeducation improvespainbeliefsinpatientswithchronicfatiguesyndromecompared topacingandself-managementeducation:adouble-blindrandomised controlledtrial.ArchPhys MedRehabil.2010;91:1153–1159.</ref> | |||
==== Emotional Awareness and Expression Therapy (EAET) ==== | |||
[https://www.physio-pedia.com/index.php?title=Physiopedia:Emotional_Awareness_and_Expression_Therapy&utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal EAET] is a group intervention focusing of emotional awareness and expression of emotions was found to be more effective than cognitive behavioral therapy in reducing pain for up to 6 months.<ref>Lumley MA, Schubiner H, Lockhart NA, Kidwell KM, Harte SE, Clauw DJ, Williams DA. [https://insights.ovid.com/pubmed?pmid=28796118 Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: a cluster-randomized controlled trial.] Pain. 2017 Dec 1;158(12):2354-63.</ref> | |||
==== Chiropractic care & Massage ==== | |||
There is no evidence to support chiropractic care nor therapeutic massage are effective in pain management. <ref name="p9" /> | |||
== | ==== Acupuncture ==== | ||
While many patients explore this option for relief of pain and fatigue, [[Acupuncture|acupuncture techniques]] have weak evidence to support their effectiveness in current literature. <ref name="p0" /> | |||
==== Alternative/Holistic Management ==== | |||
There is no evidence to support [[Alternative Therapies for Pain Conditions|alternative]]/holistic management. | |||
< | == <b>Differential Diagnosis </b> == | ||
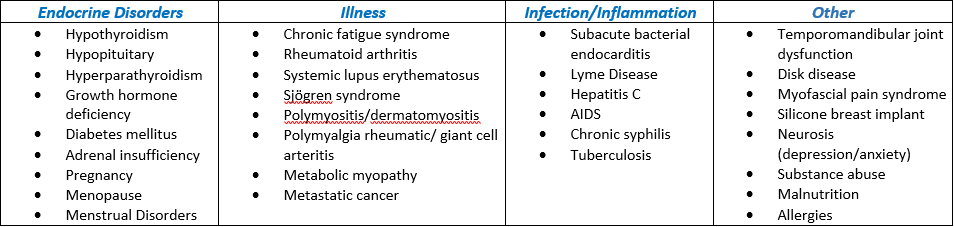
The following are all differential diagnoses for FMS. It is possible for several to be present concurrently. Moreover, it is important to determine the presence of all potential facets and diagnoses in order to successfully treat a patient with suspected fibromyalgia.<ref name="p1" /> | |||
[[Image:FMS Differential.png|center]] | |||
== <b>Case Reports</b> == | |||
[[Fibromyalgia Case Study|Fibromyalgia Case Study]] | |||
A case-control study examining the role of physical trauma in the onset of fibromyalgia syndrome (Full Text [http://rheumatology.oxfordjournals.org/cgi/content/full/41/4/450 Here]) | |||
Tailored cognitive-behavioral therapy for fibromyalgia: Two case studies. (Abstract [http://www.pec-journal.com/article/S0738-3991(07)00484-3/abstract Here]) | |||
Insular hypometabolism in a patient with Fibromyalgia: A case study. (Abstract [http://www.prohealth.com/fibromyalgia/library/showarticle.cfm?libid=13573 Here]) | |||
== | == Link between Fibromyalgia and Neuroinflammation == | ||
Here is a video explaining the link between Fibromyalgia and Neuroinflammation: <ref>Dr. Andrea Furlan. Understanding the link between Fibromyalgia and Neuroinflammation. Available from: https://www.youtube.com/watch?v=fEVrAFZV2Eo&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023). </ref> | |||
{{#ev:youtube|fEVrAFZV2Eo}} | |||
== <b>Resources</b> == | |||
[https://www.cdc.gov/arthritis/basics/fibromyalgia.htm Centers for Disease Control and Prevention] - Fibromyalgia as it relates of Arthritis from the | |||
[http://afsafund.org/fibromyalgia.html National Fibromyalgia Association] | |||
[http://www.fibrocenter.com/ FibroCenter.org] | |||
[http://www.apta.org/PTinMotion/News/2016/8/3/FibromyalgiaCPG/ APTA Conservative PT Management for Fibromyalgia] | |||
[http://www.prevention.com/fitness/fitness-tips/best-workouts-chronic-pain-and-fibromyalgia/ APTA Recommendation for "Best Workout Options" for Chronic Pain] | |||
[https://www.youtube.com/watch?v=gwd-wLdIHjs&app=desktop/ Ted Talk] - A short lecture discussing the perception of pain can pose as an example of how to approach educating patients with chronic and/or catastrophizing pain symptoms, like Patient with FMS. | |||
== References == | |||
1. Goodman, Catherine and Fuller Kendra. Pathology: Implications for the Physical Therapist. Philadelphia, WB Saunders. 4th edition (Goodman & Fuller), 2014. (pp. 310-317) (LoE: 5) | |||
2. Solano C, Martinez A, Martinez-Lavin M, et al. Autonomic dysfunction in fibromyalgia assessed by the Composite Autonomic Symptoms Scale (COMPASS). Journal Of Clinical Rheumatology: Practical Reports On Rheumatic & Musculoskeletal Diseases [serial online]. June 2009;15(4):172-176. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017. (LoE: 3b) | |||
3. Wolfe F, Clauw D, Yunus M, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care & Research [serial online]. May 2010;62(5):600-610. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017. (LoE: 1b) | |||
4. Wolfe F, Rasker J. The Symptom Intensity Scale, Fibromyalgia, and the Meaning of Fibromyalgia-like Symptoms. Journal Of Rheumatology [serial online]. November 2006;33(11):2291-2299. Available from: CINAHL, Ipswich, MA. Accessed April 2, 2017. (LoE: 4) | |||
5. Bennett R, Friend R, Jones K, Ward R, Han B, Ross R. The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties. Arthritis Research & Therapy [serial online]. 2009;11(4):R120. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017. (LoE: 1b) | |||
6. Korszun A. Sleep and circadian rhythm disorders in fibromyalgia. Current Rheumatology Reports [serial online]. April 2000;2(2):124-130. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017. (LoE: 3a) | |||
7. Moseley GL. Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 2005;51:49–52. (LoE: 4) | |||
8. Meeus M,Nijs J,VanOosterwijck J,etal.Painphysiologyeducation improvespainbeliefsinpatientswithchronicfatiguesyndromecompared topacingandself-managementeducation:adouble-blindrandomised controlledtrial.ArchPhys MedRehabil.2010;91:1153–1159. (LoE: 1b) | |||
9. Brosseau L, Wells G, Veilleux L, et al. Ottawa Panel evidence-based clinical practice guidelines for aerobic fitness exercises in the management of fibromyalgia: part 1. Physical Therapy [serial online]. July 2008;88(7):857-871. Available from: CINAHL, Ipswich, MA. Accessed April 4, 2017. (LoE: 1a) | |||
10. Skyba DA, Radhakrishnan R, Rohlwing JJ, et al. Joint manipulation reduces hyperalgesia by activation of monoamine receptors but not opioid or GABA receptors in the spinal cord. Pain. 2003;106:159–168. (LoE: 1b) | |||
11. Lofgren M, Norrbrink C. Pain relief in women with fibromyalgia: a cross-over study of superficial warmth stimulation and transcutaneous electrical nerve stimulation. J Rehabil Med.2009;41:557–562. | |||
& | 12. Ekici G, Bakar Y, Akbayrak T, Yuksel I. Comparison of manual lymph drainage therapy and connective tissue massage in women with fibromyalgia: a randomized controlled trial. Journal Of Manipulative & Physiological Therapeutics [serial online]. February 2009;32(2S):127-133. Available from: CINAHL, Ipswich, MA. Accessed April 5, 2017. | ||
13. Mannerkorpi K, Nordeman L, Ericsson A, et al. Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analyses. J Rehabil Med. 2009;41:751–760. | |||
14. Bazzichi L, Da Valle Y, Lucacchini A, et al. A multidisciplinary approach to study the effects of balneotherapy and mud-bath therapy treatments on fibromyalgia. Clinical And Experimental Rheumatology [serial online]. November 2013;31(6 Suppl 79):S111-S120. Available from: MEDLINE, Ipswich, MA. Accessed April 4, 2017. | |||
15. Poole J, Siegel P. Effectiveness of Occupational Therapy Interventions for Adults With Fibromyalgia: A Systematic Review. American Journal Of Occupational Therapy [serial online]. January 2017;71(1):1-10. Available from: CINAHL, Ipswich, MA. Accessed April 4, 2017. | |||
16. Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. 2004;8:39–45. | |||
17. Lazaridou A, Jieun K, Kim J, et al. Effects of Cognitive-Behavioral Therapy (CBT) on Brain Connectivity Supporting Catastrophizing in Fibromyalgia. Clinical Journal Of Pain [serial online]. March 2017;33(3):215-221. Available from: CINAHL, Ipswich, MA. Accessed April 5, 2017. | |||
18. Martínez M, Miró E, Buela-Casal G, et al. Cognitive-behavioral therapy for insomnia and sleep hygiene in fibromyalgia: a randomized controlled trial. Journal Of Behavioral Medicine [serial online]. August 2014;37(4):683-697. Available from: CINAHL, Ipswich, MA. Accessed | |||
19. Wise P, Walsh M. Chiropractic treatment of fibromyalgia: two case studies. Chiropractic Journal Of Australia [serial online]. June 2001;31(2):42-46. Available from: CINAHL, Ipswich, MA. Accessed April 5, 2017. | |||
20. Carville SF, Arendt-Nielsen S, Bliddal H, et al. EULAR evidence-based recommendations for the management of fibromyalgia syndrome. Ann Rheum Dis. 2008;67:536–541. | |||
[[Category:Rheumatology]] [[Category: | 21. Carey, W. D., & Cleveland Clinic Foundation. (2010). Current clinical medicine (2nd ed.). Philadelphia: Saunders Elsevier. | ||
<references /> | |||
[[Category:Autoimmune Disorders]] | |||
[[Category:Non Communicable Diseases]] | |||
[[Category:Conditions]] | |||
[[Category:Rheumatology]] | |||
[[Category:Pain]] | |||
[[Category:Bellarmine Student Project]] | |||
Latest revision as of 01:56, 7 February 2024
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Amanda Collard, Jaclyn Crush, Elaine Lonnemann, Kapil Narale, Sweta Christian, Admin, Vidya Acharya, Rachael Lowe, Gayatri Jadav Upadhyay, Lucinda hampton, Kim Jackson, Wajeeha Hassan, Jo Etherton, Ward dirk Merckx, Samuel Adedigba, Aimee Tow, Kalyani Yajnanarayan, Mila Andreew, Ahmed M Diab, Sehriban Ozmen, WikiSysop and 127.0.0.1
Definition/Description[edit | edit source]
Fibromyalgia Syndrome (FMS) is a disease characterized by chronic pain, stiffness, and tenderness of muscles, tendons, and joints, without detectable inflammation. Fibromyalgia does not cause body damage or deformity. Fatigue affects 90 percent of patients, and sleep disorders are common. Fibromyalgia can be associated with other rheumatic conditions, and irritable bowel syndrome (IBS). There is no definitive medical test for the diagnosis of fibromyalgia. Fibromyalgia symptoms can occur and disappear over time. Diagnosis is made by eliminating other possible causes of the symptoms. It can take time to identify which symptoms are caused by which problems [1]. FMS is NOT just one condition; it's a complex syndrome involving many different factors that can severely impact and disrupt a person’s daily life.
FMS is considered a systemic problem involving biochemical, neuroendocrine, and physiologic abnormalities, leading to a disorder of pain processing and perception (i.e. allodynia, hyperalgesia). The symptoms associated with FMS may originate from primary or secondary/reactive causes. [2] As fibromyalgia encompasses persistent pain in various areas, without any evidence of tissue damage, it is classified as nociplastic pain. [3]
The most effective treatment is a combination of education, stress reduction, exercise, and medication.
Here is a thorough video from Dr. Andrea Furlan, with an explanation of Fibromyalgia: [4]
Prevalence[edit | edit source]
FMS occurs in more than 6 million Americans, or 4% of the population, causing it to be the most common musculoskeletal disorder in the U.S. It mainly effects women (90%) more often than men. Symptoms typically present between the ages of 20-55 years, but individuals have been diagnosed as young as 6 years and as old as 85 years of age.[2]
Pathophysiology[edit | edit source]
The pathogenesis of FMS is theorised to be a malfunctioning of the central nervous system (CNS), characterized by central sensitisation, which is a heightened pain perception accompanied by ineffective pain inhibition and/or modulation. This increased response to peripheral stimuli causes hyperalgesia, allodynia, and referred pain across multiple spinal segments, resulting in chronic widespread pain and decreased tolerance to sensory input of the musculoskeletal system.
FMS systemically causes a dysregulation : : neurologic; immunologic; endocrinologic; and enteric organ systems [2].
1. Autonomic Nervous System
The Autonomic Nervous System (ANS) is responsible for regulating the Sympathetic (“fight or flight”) and the Parasympathetic (“rest and digest”) responses. With FMS, patients experience a systemically heightened sympathetic (SNS) response with a diminished parasympathetic (PNS) modulation. Continuous over activation of the SNS results in increased heart rate, excessive gastric secretions and contractions, abnormalities of smooth muscle contraction throughout the digestive tract, rapid and shallow respiration, and vasoconstriction. This can lead to malnutrition due to absorption and digestion disruptions. Prolonged inhibition of PNS alters the neuroimmunoendocrine systems, directly affecting growth hormone secretion by the pituitary gland. This can result in nonrestorative sleep, pain, fatigue, and cognitive/mood symptoms. [2]
2. Immune System
The immune response to infection, inflammation, and/or trauma is a release of cytokines for local healing, which trigger the CNS to release glial cells within the brain and spinal cord for healing support and pain response. With FMS, this auto-immune response is heightened, causing an excess of glia in the body, which creates an exaggerated state of pain (chronic).[2]
Causes[edit | edit source]
There are many hypotheses of how multiple factors play a role in the development of FMS. The exact etiology of FMS is still being researched; however, there are several potential causes and risk factors, listed below, that are currently associated with, or increase one’s risk for developing this condition[2].
- Diet
- Viral
- Occupation, seasonal, environmental influences
- Adverse childhood experiences (i.e. PTSD)
- Psychological and cognitive/behavioral factors
- Other conditions: rheumatoid athritis, systemic lupus erythematosus, or ankylosing spondylitis AS
Current research remains inconclusive regarding the genetic or hereditary cause of FMS. A family history of FMS is also a risk factor.
Characteristics/Clinical Presentation[edit | edit source]
Muscle pain is characterised as the major symptom of FMS, often described by patients as “aching or burning” regardless of physical activity. Other symptoms or associated problems occur, with various reports of frequencies, that can also affect function. FMS may cause residual pain sensations at a lower intensity due to repetitive exposure to peripheral stimuli or activity, also known as the “Wind-up Response.” [5][2] Other symptoms include sleep disturbances, fatigue, and other cognitive and somatic symptoms. [6]
Symptoms are often exacerbated by:
- Stress
- Overloading physical activity
- Overstretching
- Damp or chilly weather
- Heat exposure or humidity
- Sudden change in barometric pressure
- Trauma
- Another illness
A recent study carried out by Sempere-Rubio et al found out that functional capacity, upper limb muscular strength, postural maintenance, pain threshold, and anxiety are important predictive factors of Quality of Life (QoL) in women with FMS.[7]
Associated Co-morbidities[edit | edit source]
Those with FMS are likely to present with several co-morbidities. It is important that a diagnosis of FMS is not overlooked given the presence of additional co-morbidities which would be more commonly diagnosed. Below is a list of common co-morbidities associated with FMS [2]:
- Sleep disturbances / apnea
- Depression
- Anxiety
- PTSD
- Rheumatoid arthritis
- Systemic Lupus Erythematosus
- Ankylosing Spondylitis (Axial Spondyloarthritis),
Fibromyalgia Diagnostic Criteria (2016)[edit | edit source]
There is no definitive diagnostic test currently available to determine the presence of FMS. A diagnosis of FMS is generally made based upon the results of a physical examination and ruling out other similar conditions. No special laboratory or radiologic testing is necessary for making a diagnosis; however, some recommended lab tests can be performed in order to rule out other conditions. These tests include: CBC, ESR, basic chemistry (blood urea nitrogen, creatine, hepatic enzymes, serum calcium), thyroid levels (TSH, T3, and T4), and Rheumatoid factor.
Fibromyalgia may now be diagnosed in adults when all of the following criteria are met [8]:
- Widespread pain index (WPI) ≥7 and Symptom Severity Scale (SSS) score ≥5 OR WPI 4–6 and SSS score ≥9.
- Generalised pain, defined as pain in at least 4 of 5 regions, is present.
- Symptoms have been present at a similar level for at least 3 months.
- A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses.
Here is a video from Dr. Andrea Furlan on how Doctors diagnose Fibromyalgia:
Management[edit | edit source]
Medication[edit | edit source]
Active rehabilitative approaches have primacy in management, but drugs can help to control symptoms. There is evidence to support the use of amitriptyline, duloxetine, milnacipran or pregabalin, but pure opioids should be avoided [9].
Physical Therapy Management & Exercise[edit | edit source]
Education about the pathophysiology and the neuroscience behind the condition is the most effective method in reducing catastrophising pain symptoms in patients experiencing FMS, according to current research. Simple acknowledgement and explanation of symptoms, and relaxation strategies can enhance a patient’s ability to cope with their condition.
- Explanation of disorder
- Reassurance of condition and symptoms
- Activity management - Pacing, self-monitoring, rest breaks, AVOID exacerbations, set realistic activity goals, etc.
- Relaxation Techniques - Minimize environmental stress, deep breathing, healthy & active lifestyle habits, adequate sleep, therapeutic massage, etc.
[10]
[Example of a Physical Therapist providing a patient with the educational tools to manage their condition and rehabilitation process.]
Here is a video with an explanation to exercises for patients with Fibromyalgia, since it is helpful for the condition. There are 3 other videos that follow this video, one on strengthening, low intensity aerobic exercises, and stretching exercises, which are presented in the next section: [11]
Aerobic and Resistance Exercise[edit | edit source]
According to the Ottawa Panel Evidence-Based Clinical Practice Guidelines (2008), supervised light aerobic exercise and strength/resistance training is highly recommended for the management of patients with chronic pain, such as those with FMS. It has been found to increase their capacity for activity while minimising their symptoms associated with FMS. Specifically, aerobic activity has been shown to improve psychological symptoms associated with depression, cognitive decline, and sleep disturbances. Exercise also improves patient’s cellular metabolism and respiratory capacity, increases lean muscle mass and tone, and increases oxygen uptake within the body’s system(s), which ultimately reduces their complaints of chronic pain and fatigue. [2][12]
Here is a video on strengthening exercises: [13]
Here is a video on gentle aerobic exercises for Fibromyalgia: [14]
Here is a video on stretching exercises for Fibromyalgia: [15]
Manual / Passive Therapy[edit | edit source]
Some studies support that TENS and joint mobilisations foster the reduction of pain as short-term relief in patients with FMS. Specifically, patients with chronic back pain due to FMS may benefit from spinal manipulations with limited evidence to support this modality. Moderate evidence shows that the use of passive soft tissue manipulation (STM) is helpful with pain regulation. In addition, diffuse chronic pain presentations are less likely to be reliable for medical management with TENS compared to localised pain. Passive therapy should not be the foundation of FMS medical management due to the maladaptive illness beliefs and coping strategies for patients’ pain. [16][2][5]
Manual lymph drainage therapy and connective tissue massage have also been studied in women with fibromyalgia. Researchers used the Fibromyalgia Impact Questionnaire (FIQ) and the Nottingham Health Profile to measure the impact of the treatment. Their research suggests that both manual lymph drainage therapy and connective tissue massage show improvements in both the FIQ and the Nottingham Health Profile. However, there were significantly greater improvements in the group that received manual lymph drainage therapy, suggesting that manual lymphatic drainage therapy may be preferred over connective tissue massage.
Aquatic Therapy & Balneotherapy[edit | edit source]
Recent research has proven that aquatic therapy is a more tolerable workout for people with FMS pain. The water’s buoyancy allows the patient to maintain active movement without exerting excessive energy and/or increasing pressure on their joints. Furthermore, evidence has shown that aquatic therapy and hydrotherapy help in improving the quality of life of those with chronic FMS.[17][18] The underlying symptom(s) of fibromyalgia, central hypersensitivity and pain, may be alleviated by the hydrostatic pressure and the effects of soothing temperature on the nerve endings, along with general muscle relaxation.
Ideal pool temperature for aquatic therapy sessions are between 84o F and 90o F
- 82o F and 84o F for the general population
- 90o F and 94o F for people with arthritic conditions
An exercise-education program showed a small significant improvement in health status in patients with fibromyalgia and chronic widespread pain, compared with education only. Patients with milder symptoms improved most with this treatment. Moreover, it has been shown that thermal mud baths (and other balneotherapy methods) increase plasma levels of beta-endorphins, thus explaining their analgesic and anti-spastic effects, which is particularly important in patients with FMS. [18][17][5][2][12]
Other Types of Management[edit | edit source]
Occupational Therapy[edit | edit source]
Treatment focuses on activity modification principles, such as working at a moderate pace, frequent positional/postural changes, and resting before fatigue sets in. Patients are encouraged to incorporate regulating principles into all areas of life including self-care, work, and leisure. Proper body mechanics and posture related to home management and work activities are evaluated and adjusted per individual.[19]
Cognitive Behavioral Therapy[edit | edit source]
Research performed by Moseley supports the relationship between pain association and beliefs with physical performance. There is evidence that supports the consideration of cognitive behavioral therapy (CBT) to be implemented in the assessment and plan of care of patients with chronic pain. Growing evidence continues to demonstrate that CBT shows improvement in reports of pain, reduces hyperalgesia, and chronic pain-related brain response in FMS.
Another study found that behavioral insomnia therapy for patients with FMS may have a promising impact. The study incorporated patient education on sleeping habits and proper sleeping schedules to reduce the bouts of insomnia experienced by those with fibromyalgia. The researchers concluded that patients who received the behavioral therapy experienced improvement in how long they slept and in their general condition compared to other groups. [20][21][22]
Emotional Awareness and Expression Therapy (EAET)[edit | edit source]
EAET is a group intervention focusing of emotional awareness and expression of emotions was found to be more effective than cognitive behavioral therapy in reducing pain for up to 6 months.[23]
Chiropractic care & Massage[edit | edit source]
There is no evidence to support chiropractic care nor therapeutic massage are effective in pain management. [12]
Acupuncture[edit | edit source]
While many patients explore this option for relief of pain and fatigue, acupuncture techniques have weak evidence to support their effectiveness in current literature. [16]
Alternative/Holistic Management[edit | edit source]
There is no evidence to support alternative/holistic management.
Differential Diagnosis [edit | edit source]
The following are all differential diagnoses for FMS. It is possible for several to be present concurrently. Moreover, it is important to determine the presence of all potential facets and diagnoses in order to successfully treat a patient with suspected fibromyalgia.[2]
Case Reports[edit | edit source]
A case-control study examining the role of physical trauma in the onset of fibromyalgia syndrome (Full Text Here)
Tailored cognitive-behavioral therapy for fibromyalgia: Two case studies. (Abstract Here)
Insular hypometabolism in a patient with Fibromyalgia: A case study. (Abstract Here)
Link between Fibromyalgia and Neuroinflammation[edit | edit source]
Here is a video explaining the link between Fibromyalgia and Neuroinflammation: [24]
Resources[edit | edit source]
Centers for Disease Control and Prevention - Fibromyalgia as it relates of Arthritis from the
National Fibromyalgia Association
APTA Conservative PT Management for Fibromyalgia
APTA Recommendation for "Best Workout Options" for Chronic Pain
Ted Talk - A short lecture discussing the perception of pain can pose as an example of how to approach educating patients with chronic and/or catastrophizing pain symptoms, like Patient with FMS.
References[edit | edit source]
1. Goodman, Catherine and Fuller Kendra. Pathology: Implications for the Physical Therapist. Philadelphia, WB Saunders. 4th edition (Goodman & Fuller), 2014. (pp. 310-317) (LoE: 5)
2. Solano C, Martinez A, Martinez-Lavin M, et al. Autonomic dysfunction in fibromyalgia assessed by the Composite Autonomic Symptoms Scale (COMPASS). Journal Of Clinical Rheumatology: Practical Reports On Rheumatic & Musculoskeletal Diseases [serial online]. June 2009;15(4):172-176. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017. (LoE: 3b)
3. Wolfe F, Clauw D, Yunus M, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care & Research [serial online]. May 2010;62(5):600-610. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017. (LoE: 1b)
4. Wolfe F, Rasker J. The Symptom Intensity Scale, Fibromyalgia, and the Meaning of Fibromyalgia-like Symptoms. Journal Of Rheumatology [serial online]. November 2006;33(11):2291-2299. Available from: CINAHL, Ipswich, MA. Accessed April 2, 2017. (LoE: 4)
5. Bennett R, Friend R, Jones K, Ward R, Han B, Ross R. The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties. Arthritis Research & Therapy [serial online]. 2009;11(4):R120. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017. (LoE: 1b)
6. Korszun A. Sleep and circadian rhythm disorders in fibromyalgia. Current Rheumatology Reports [serial online]. April 2000;2(2):124-130. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017. (LoE: 3a)
7. Moseley GL. Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 2005;51:49–52. (LoE: 4)
8. Meeus M,Nijs J,VanOosterwijck J,etal.Painphysiologyeducation improvespainbeliefsinpatientswithchronicfatiguesyndromecompared topacingandself-managementeducation:adouble-blindrandomised controlledtrial.ArchPhys MedRehabil.2010;91:1153–1159. (LoE: 1b)
9. Brosseau L, Wells G, Veilleux L, et al. Ottawa Panel evidence-based clinical practice guidelines for aerobic fitness exercises in the management of fibromyalgia: part 1. Physical Therapy [serial online]. July 2008;88(7):857-871. Available from: CINAHL, Ipswich, MA. Accessed April 4, 2017. (LoE: 1a)
10. Skyba DA, Radhakrishnan R, Rohlwing JJ, et al. Joint manipulation reduces hyperalgesia by activation of monoamine receptors but not opioid or GABA receptors in the spinal cord. Pain. 2003;106:159–168. (LoE: 1b)
11. Lofgren M, Norrbrink C. Pain relief in women with fibromyalgia: a cross-over study of superficial warmth stimulation and transcutaneous electrical nerve stimulation. J Rehabil Med.2009;41:557–562.
12. Ekici G, Bakar Y, Akbayrak T, Yuksel I. Comparison of manual lymph drainage therapy and connective tissue massage in women with fibromyalgia: a randomized controlled trial. Journal Of Manipulative & Physiological Therapeutics [serial online]. February 2009;32(2S):127-133. Available from: CINAHL, Ipswich, MA. Accessed April 5, 2017.
13. Mannerkorpi K, Nordeman L, Ericsson A, et al. Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analyses. J Rehabil Med. 2009;41:751–760.
14. Bazzichi L, Da Valle Y, Lucacchini A, et al. A multidisciplinary approach to study the effects of balneotherapy and mud-bath therapy treatments on fibromyalgia. Clinical And Experimental Rheumatology [serial online]. November 2013;31(6 Suppl 79):S111-S120. Available from: MEDLINE, Ipswich, MA. Accessed April 4, 2017.
15. Poole J, Siegel P. Effectiveness of Occupational Therapy Interventions for Adults With Fibromyalgia: A Systematic Review. American Journal Of Occupational Therapy [serial online]. January 2017;71(1):1-10. Available from: CINAHL, Ipswich, MA. Accessed April 4, 2017.
16. Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. 2004;8:39–45.
17. Lazaridou A, Jieun K, Kim J, et al. Effects of Cognitive-Behavioral Therapy (CBT) on Brain Connectivity Supporting Catastrophizing in Fibromyalgia. Clinical Journal Of Pain [serial online]. March 2017;33(3):215-221. Available from: CINAHL, Ipswich, MA. Accessed April 5, 2017.
18. Martínez M, Miró E, Buela-Casal G, et al. Cognitive-behavioral therapy for insomnia and sleep hygiene in fibromyalgia: a randomized controlled trial. Journal Of Behavioral Medicine [serial online]. August 2014;37(4):683-697. Available from: CINAHL, Ipswich, MA. Accessed
19. Wise P, Walsh M. Chiropractic treatment of fibromyalgia: two case studies. Chiropractic Journal Of Australia [serial online]. June 2001;31(2):42-46. Available from: CINAHL, Ipswich, MA. Accessed April 5, 2017.
20. Carville SF, Arendt-Nielsen S, Bliddal H, et al. EULAR evidence-based recommendations for the management of fibromyalgia syndrome. Ann Rheum Dis. 2008;67:536–541.
21. Carey, W. D., & Cleveland Clinic Foundation. (2010). Current clinical medicine (2nd ed.). Philadelphia: Saunders Elsevier.
- ↑ Medicine net. Medical definition of fibromyalgia Available from: https://www.medicinenet.com/script/main/art.asp?articlekey=3453 (last accessed 6.10.19)
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Goodman, Catherine and Fuller Kendra. Pathology: Implications for the Physical Therapist. Philadelphia, WB Saunders. 4th edition (Goodman & Fuller), 2014. (pp. 310-317)
- ↑ International Association for the Study of Pain - What's in a Name for Chronic Pain? “Nociplastic pain” was officially adopted by IASP as the third mechanistic descriptor of chronic pain. Available from: https://www.iasp-pain.org/publications/pain-research-forum/prf-news/92059-whats-name-chronic-pain/ (accessed 11 August 2023).
- ↑ Dr. Andrea Furlan. Fibromyalgia by Dr. Andrea Furlan MD, PhD. Available from: https://www.youtube.com/watch?v=_1B8U-eEkE0&t=53s&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023).
- ↑ 5.0 5.1 5.2 Solano C, Martinez A, Martinez-Lavin M, et al. Autonomic dysfunction in fibromyalgia assessed by the Composite Autonomic Symptoms Scale (COMPASS). Journal Of Clinical Rheumatology: Practical Reports On Rheumatic & Musculoskeletal Diseases [serial online]. June 2009;15(4):172-176. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017.
- ↑ Bair MJ, Krebs EE. Fibromyalgia. Annals of internal medicine. 2020 Mar 3;172(5):ITC33-48. https://sci-hub.hkvisa.net/10.7326/AITC202003030
- ↑ Sempere-Rubio N, Aguilar-Rodríguez M, Inglés M, Izquierdo-Alventosa R, Serra-Añó P. Physical Condition Factors that Predict a Better Quality of Life in Women with Fibromyalgia. International journal of environmental research and public health. 2019 Jan;16(17):3173.
- ↑ Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, Mease PJ, Russell AS, Russell IJ, Walitt B. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. InSeminars in arthritis and rheumatism 2016 Dec 1 (Vol. 46, No. 3, pp. 319-329). WB Saunders. Available from: https://acrabstracts.org/abstract/2016-revisions-to-the-20102011-fibromyalgia-diagnostic-criteria/ (last accessed 6.9.2019)
- ↑ Kwiatek R. Treatment of fibromyalgia. Australian prescriber. 2017 Oct;40(5):179. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5662432/ (last accessed 6.10.19)
- ↑ Jackie Crush Basic Educational Tool for Fibromyalgia Syndrome. Available from https://www.youtube.com/watch?time_continue=6&v=RYZ2BtFjZAg&feature=emb_logo
- ↑ Dr. Andrea Furlan. #094 Fibromyalgia: A beginner's guide to start exercising. Available from: https://www.youtube.com/watch?v=eOK_I-5cMHQ&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023).
- ↑ 12.0 12.1 12.2 Brosseau L, Wells G, Veilleux L, et al. Ottawa Panel evidence-based clinical practice guidelines for aerobic fitness exercises in the management of fibromyalgia: part 1. Physical Therapy [serial online]. July 2008;88(7):857-871. Available from: CINAHL, Ipswich, MA. Accessed April 4, 2017.
- ↑ Dr. Andrea Furlan. #095 Fibromyalgia: Resistance (weight training) exercises to gain power and strength. Available from: https://www.youtube.com/watch?v=XlyUQK-RplI&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023).
- ↑ Dr. Andrea Furlan. #096 Fibromyalgia: A 20-minute low-intensity (cardio) exercise routine. Available from: https://www.youtube.com/watch?v=Gd1fdRA-ZjA&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023).
- ↑ Dr. Andrea Furlan. #097 Fibromyalgia: A 15-miute gentle stretching routine. Available from: https://www.youtube.com/watch?v=YMFES0QpwA8&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023).
- ↑ 16.0 16.1 Skyba DA, Radhakrishnan R, Rohlwing JJ, et al. Joint manipulation reduces hyperalgesia by activation of monoamine receptors but not opioid or GABA receptors in the spinal cord. Pain. 2003;106:159–168.
- ↑ 17.0 17.1 Wolfe F, Rasker J. The Symptom Intensity Scale, Fibromyalgia, and the Meaning of Fibromyalgia-like Symptoms. Journal Of Rheumatology [serial online]. November 2006;33(11):2291-2299. Available from: CINAHL, Ipswich, MA. Accessed April 2, 2017.
- ↑ 18.0 18.1 Wolfe F, Clauw D, Yunus M, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care & Research [serial online]. May 2010;62(5):600-610. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017.
- ↑ Bennett R, Friend R, Jones K, Ward R, Han B, Ross R. The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties. Arthritis Research & Therapy [serial online]. 2009;11(4):R120. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017.
- ↑ Korszun A. Sleep and circadian rhythm disorders in fibromyalgia. Current Rheumatology Reports [serial online]. April 2000;2(2):124-130. Available from: MEDLINE, Ipswich, MA. Accessed April 2, 2017.
- ↑ Moseley GL. Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 2005;51:49–52.
- ↑ Meeus M,Nijs J,VanOosterwijck J,etal.Painphysiologyeducation improvespainbeliefsinpatientswithchronicfatiguesyndromecompared topacingandself-managementeducation:adouble-blindrandomised controlledtrial.ArchPhys MedRehabil.2010;91:1153–1159.
- ↑ Lumley MA, Schubiner H, Lockhart NA, Kidwell KM, Harte SE, Clauw DJ, Williams DA. Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: a cluster-randomized controlled trial. Pain. 2017 Dec 1;158(12):2354-63.
- ↑ Dr. Andrea Furlan. Understanding the link between Fibromyalgia and Neuroinflammation. Available from: https://www.youtube.com/watch?v=fEVrAFZV2Eo&ab_channel=Dr.AndreaFurlan (accessed 16 September 2023).