Introduction to Foot Neuropathy
Top Contributors - Stacy Schiurring, Jess Bell and Matt Huey
Introduction[edit | edit source]
Diabetes is a global epidemic, affecting more than 537 million adults worldwide.[1] Of those, 40 to 60 million people have diabetic-related foot and lower extremity complications. Diabetes accounts for 9% of total adult health care costs.[2]
Peripheral neuropathy is a common consequence of diabetes, with a prevalence of anywhere from 10 to 85%.[2] The outcomes of peripheral neuropathy can be devastating and include (1) foot ulcers, (2) major amputation, (3) falls, (4) intracranial injuries, and (5) decreased quality of life.[1] Approximately one in four people with diabetes will develop a diabetic foot ulcer:
- individuals with a diabetic foot ulcer have a 2.5 times greater mortality risk than people with diabetes who do not develop a foot ulcer
- their mortality rate increases to 42% within five years of developing a diabetic foot ulcer
- after one year, 20% of diabetic foot ulcers remain unhealed
- the recurrence rate for healed diabetic foot ulcers within one year is 40%, and within five years is 65%[2]
This page introduces the causes and types of peripheral neuropathy, exploring aetiology beyond diabetes.
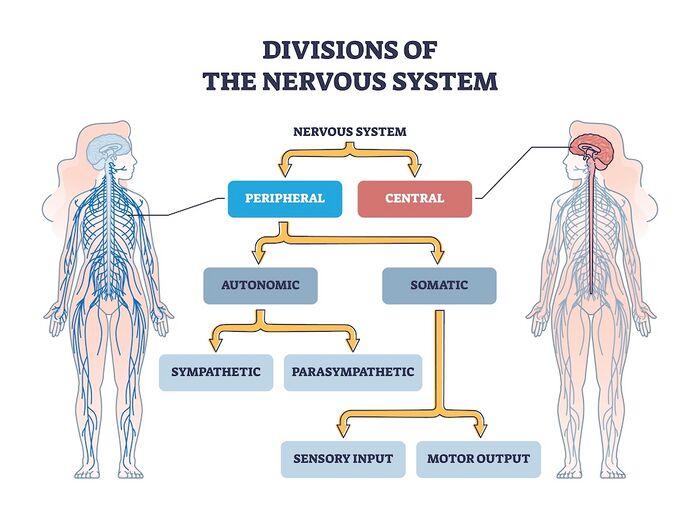
Neuroanatomy Review[edit | edit source]
- Central Nervous System: includes the brain and spinal cord. The central nervous system (CNS) is the body's processing centre. In general terms, the three functions of the CNS are to (1) take in sensory information, (2) process that information, and (3) send out motor signals. Through these mechanisms, the CNS controls most of the body's functions, including movement, sensation through our five senses, and higher-level functions such as cognition, awareness, and speech. The spinal cord is an extension of the brain and serves as a neural pathway for information exchange with the rest of the body.
- Peripheral Nervous System: a complex network of nerves which convey sensory information in from the body to the CNS via the spinal cord and transmit information out from the CNS via the spinal cord to the body. Examples of outgoing signals transmitted along the peripheral nervous system (PNS) include (1) motor information for muscle activity and (2) autonomic functioning (heart rate, blood pressure, respiration, digestion, sexual arousal).[3]
- Motor Nerves: relay information to skeletal muscles and somatic tissue, which creates voluntary movement
- Sensory Nerves: conveys sensory information about the environment in from sensory receptors in the body to the CNS
- Autonomic Nervous System: relays motor information to the visceral organs to innervate smooth muscle, cardiac muscle, and glands and functions to maintain the body's homeostasis. The autonomic nervous system has two parts: the sympathetic and parasympathetic divisions, which innervate visceral organs. The sympathetic nervous system stimulates ("fight or flight") while the parasympathetic nervous system inhibits ("rest and digest") the functions of these organs.
Peripheral Neuropathy[edit | edit source]
The term peripheral neuropathy (PN) describes many conditions which involve damage to the peripheral nervous system. Initially, this damage presents as nerve malfunction due to cellular and chemical changes. However, over time, this nerve malfunction becomes true nerve or structural damage, resulting in atrophy and demyelination.[2] There are more than 100 known types of PN, each with unique symptoms and prognosis. PN symptoms are dependent on the category of nerves involved: motor, sensory, or autonomic.[3]
The exact pathophysiology of PN depends on the underlying disease processes. However, the mechanisms of peripheral nerve injury exhibit similar patterns. These reactions include (1) segmental demyelination, (2) Wallerian degeneration, and (3) axonal degeneration.[4]
Classification methods for PN include:
- Categorisation based on the number of nerves affected - mono-neuropathies, multifocal neuropathies, poly-neuropathies[5][4]
- Can be further divided into smaller groups, such as the cause of the condition (e.g. compressive vs non-compressive) or type of neuropathy (e.g. axonal or demyelinating), etc.[6][4]
Common symptoms of PN include:
If you would like to learn more about neuropathy, please read this optional article.
Aetiology of Peripheral Neuropathies[edit | edit source]
The National Institute of Health (NIH) states that the aetiology of PN can have many causes, including metabolic, systemic, and toxic causes[4]:
- Diabetes mellitus[2][4] (most common cause of PN)
- Chronic alcoholism[2][4]
- Nutritional deficiencies (e.g., B1, B6, B12, and vitamin E)[2][4]
- Inflammatory conditions (e.g., vasculitis)[4]
- Hypothyroidism[2][4]
- Autoimmune disorders (e.g., Sjogren's syndrome[2], lupus, rheumatoid arthritis)[4]
- Infections (e.g., Lyme disease[2], Epstein-Barr virus, hepatitis C, shingles, leprosy, HIV,[4] and long COVID[7])
- Guillain-Barre syndrome[4]
- Toxins (heavy metals, chemicals such as mercury, lead, and arsenic)[4]
- Chemotherapy agents[2][4]
- Medications (antibiotics, cardiovascular medications)[4]
- Tumours (secondary to compression or associated paraneoplastic syndromes)[4]
- Inherited conditions (e.g., Charcot-Marie-Tooth disease, amyloidosis)[4]
- Trauma/injury (e.g., carpel tunnel syndrome)[4]
- Multiple myeloma and its treatments[4]
- Monoclonal gammopathy of undetermined significance (MGUS)[4][8]
- Idiopathic, when no direct cause can be identified[2]
Types of Peripheral Neuropathies[edit | edit source]
Below is an overview of the three types of PN. Recall that classification of PN is dependent on the types of nerves involved and that more than one type of PN can be present at the same time. Most people with PN experience polyneuropathy. Understanding the common symptoms and clinical presentation of each type of PN is a useful skill for the rehabilitation professional as it aids in care plan creation and guides referrals to medical colleagues.
For a more in-depth discussion of clinical diagnosis and management of peripheral neuropathy injuries, including a clinical decision-making tree, please read this optional additional research article from 2022.
Sensory Neuropathy[edit | edit source]
"Sensory neuropathies refer to a host of diseases that result in loss of sensation throughout the body ... [sensory neuropathy conditions] may further sub-divide into small fiber (pain-dominant) and large fiber (ataxia-predominant) pathologies."[9]
To classify a sensory neuropathy, it is important to identify the size of the nerve fibre and the degree of myelination. Some diseases, such as diabetes, can involve sensory polyneuropathy.[9]
- Small fibre neuropathies (Aδ and small unmyelinated C fibres)
- Large fibre neuropathies (Aβ fibres)
Special Topic: Loss of Protective Sensation[edit | edit source]
Loss of Protective Sensation (LOPS) is a complication common to patients with diabetic neuropathy. PN related to diabetes is an "anatomically diffuse process" which affects sensory and autonomic nerve fibres and, in more advanced cases, distal motor fibres. Symptoms tend to develop distally in the toes, then advance by moving proximally. This disease process leads to LOPS, meaning the person is unable to sense minor trauma and injury from mechanical, thermal, or chemical causes.[11]
LOPS is an important symptom used in the classification of diabetic foot wounds[12] because the foot is more vulnerable to physical and thermal trauma and predisposes it to deformity.[13]
Common mechanisms of injury related to LOPS:
- Exposure to constant, prolonged pressure, such as wearing shoes that are too tight
- Exposure to moderate to high repetitive pressure, which causes the development of a callus, which in turn acts as a source of pressure
- Exposure to brief high pressure, such as stepping on a sharp object which causes a wound or other injury[2]
For more information on testing for LOPS, please read this article.
All photos provided by and used with kind permission from Diane Merwarth PT.
Motor Neuropathy[edit | edit source]
Motor neuropathy is the result of damage to the motor nerves.[2]
Signs of motor neuropathy include:
- Foot deformities resulting from muscle imbalances within the foot[2] and the non-enzymatic glycation of proteins.[14]
- Common deformities include (1) hammer toe, (2) claw toe, and (3) pes equinus[2]
- Changes in gait pattern due to tendon shortening
- Tendons commonly affected include (1) Achilles tendon and the (2) flexor hallucis tendons[2]
- Loss of deep tendon reflexes (DTRs)[2]
- Other symptoms can include:
- muscle twitching and cramps
- muscle weakness or paralysis
- muscle wasting[15]
All photos provided by and used with kind permission from Diane Merwarth PT.
Autonomic Neuropathy[edit | edit source]
"Autonomic neuropathies are a collection of syndromes and diseases affecting the autonomic neurons, either parasympathetic or sympathetic, or both. Autonomic neuropathies can be hereditary or acquired in nature."[16]
Signs and symptoms of autonomic neuropathy can present across a wide variety of body systems. Many of these impairments can affect a patient's gait pattern, putting them at greater risk for foot dysfunction and wound formation. Other impairments can increase an individual's fall risk (e.g. increased urinary frequency and urgency or a decreased ability to effectively scan the environment).
- Cardiovascular system:
- Digestive system. Digestive difficulties can include:[17]
- feelings of bloating, fullness, and nausea
- vomiting
- constipation
- diarrhoea
- faecal incontinence
- gastroparesis
- swallowing impairments
- Urogenital system:
- bladder impairments:[17]
- impaired ability to sense the need to void
- urinary incontinence
- bladder infections stemming from urinary retention
- bladder impairments:[17]
- Integumentary system:
- non-enzymatic glycation of protein:[2][14]
- causes thickened, taut, inflexible skin on the foot. These skin changes cause additional pressures against bony prominences, which can put the patient at risk of developing an ischaemic ulcer over those areas.[2]
- predisposes skin for formation of skin fissures[2] [14]
- causes contracture of the fascial structures, which can lead to joint deformity of the foot[14]
- impaired wound healing[14]
- sweat glands:
- non-enzymatic glycation of protein:[2][14]
- Eyes:
- can experience difficulty with pupil adaptation to changes in light and night blindness when driving[17]
- Can develop hypoglycemia unawareness[17]
Resources[edit | edit source]
Additional Optional Reading[edit | edit source]
- International Wound Infection Institute (IWII) Wound Infection in Clinical Practice. Wounds International. 2022.
Clinical Resources[edit | edit source]
- Neuropathy Overview (patient education handout) from the Neuropathy Action Foundation
- Please view this optional 8-minute video for an overview of the types of peripheral neuropathy. Please note this video discusses information beyond the scope of neuropathy of the feet.
References[edit | edit source]
- ↑ 1.0 1.1 Hicks CW, Wang D, Windham BG, Matsushita K, Selvin E. Prevalence of peripheral neuropathy defined by monofilament insensitivity in middle-aged and older adults in two US cohorts. Scientific reports. 2021 Sep 27;11(1):19159.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 Merwarth, D. Understanding the Foot Programme. Introduction to Foot Neuropathy. Physioplus. 2023.
- ↑ 3.0 3.1 National Institute of Health. Peripheral Neuropathy. Available from: https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy#toc-what-is-peripheral-neuropathy- (accessed 3/August/2023).
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 Hammi C, Yeung B. Neuropathy. 2022 Available from;https://www.ncbi.nlm.nih.gov/books/NBK542220/(last accessed 5/August/2023)
- ↑ Martyn CN, Hughes R. Epidemiology of peripheral neuropathy. Journal of neurology, neurosurgery, and psychiatry. 1997 Apr;62(4):310.
- ↑ Hanewinckel R, Ikram MA, Van Doorn PA. Peripheral neuropathies. Handb Clin Neurol. 2016;138:263-82.
- ↑ Oaklander AL, Mills AJ, Kelley M, Toran LS, Smith B, Dalakas MC, Nath A. Peripheral neuropathy evaluations of patients with prolonged long COVID. Neurology-Neuroimmunology Neuroinflammation. 2022 May 1;9(3).
- ↑ Rögnvaldsson S, Steingrímsson V, Turesson I, Björkholm M, Landgren O, Kristinsson SY. Peripheral neuropathy and monoclonal gammopathy of undetermined significance: a population-based study including 15,351 cases and 58,619 matched controls. haematologica. 2020 Nov 11;105(11):2679.
- ↑ 9.0 9.1 9.2 9.3 National Institute of Health. Sensory Neuropathy. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559020/ (accessed 6/August/2023).
- ↑ 10.0 10.1 Misra UK, Kalita J, Nair PP. Diagnostic approach to peripheral neuropathy. Annals of Indian Academy of Neurology. 2008 Apr;11(2):89.
- ↑ Centers for Medicare & Medicaid Services. Diabetic Peripheral Neuropathy with Loss of Protective Sensation (LOPS). Available from: https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=N&NCAId=22&%3Bfromdb=true#:~:text=Long%20nerves%20are%20affected%20first,%2C%20thermal%2C%20or%20chemical%20sources. (accessed 6/August/2023).
- ↑ Swanson T, Ousey K, Haesler E, Bjarnsholt T, Carville K, Idensohn P, Kalan L, Keast DH, Larsen D, Percival S, Schultz G. IWII Wound Infection in Clinical Practice consensus document: 2022 update. Journal of wound care. 2022 Dec 1;31(Sup12):S10-21.
- ↑ Adams OP, Herbert JR, Howitt C, Unwin N. The prevalence of peripheral neuropathy severe enough to cause a loss of protective sensation in a population‐based sample of people with known and newly detected diabetes in Barbados: a cross‐sectional study. Diabetic Medicine. 2019 Dec;36(12):1629-36.
- ↑ 14.0 14.1 14.2 14.3 14.4 Mooney J. Illustrated Dictionary of Podiatry and Foot Science E-Book. Elsevier Health Sciences; 2009 Jul 30.
- ↑ NHS. Peripheral neuropathy symptoms. Available from: https://www.nhs.uk/conditions/peripheral-neuropathy/symptoms/ (accessed 6/August/2023).
- ↑ Medscape. Autonomic Neuropathy. Available from: https://emedicine.medscape.com/article/1173756-overview?form=fpf (accessed 6/August/2023).
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 National Institute of Health. Autonomic Neuropathy. Available from: https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/autonomic-neuropathy (accessed 15/August/2023).
- ↑ YouTube. Types of Peripheral Neuropathy: How to Identify the Type of Neuropathy You Have. Available from: https://www.youtube.com/watch?v=YTsu-HN8nw4 [last accessed 16/August/2023]