Types of Rheumatic Disease
Original Editor - User Name
Top Contributors - Khloud Shreif, Lucinda hampton and Vidya Acharya
Introduction[edit | edit source]
Historically, "rheumatism" was a term used to describe a range of painful conditions affecting muscles, tendons, joints, and bones. Nowadays, we prefer the more precise term "rheumatic disease." Rheumatic disease RD is a comprehensive term encompassing arthritis and various other conditions, it encompasses over 200 different conditions, musculoskeletal system be the most affected system it is sometimes named musculoskeletal diseases, some of it's condition involving the immune system when mistakenly attacking the body's own tissues, which can lead to autoimmunity.
It is divided into:
- Autoimmune disease.
- Autoinflammatory disease.
- Degenerative/ metabolic disorders.
General Classification Criteria of Rheumatic Diseases[edit | edit source]
There is still no accurate solo diagnostic procedures to diagnose or confirm Rheumatic Diseases, the Classification criteria will help to distinguish between similar diseases and confirm or exclude a specific disease based on specific factors. These criteria are guidelines, not the only way to diagnose. Diagnosis of rheumatic disease can be challenging, it relies on clinical assessment, gathering a complete patient history and carefully evaluating the musculoskeletal system is very important, hence match the findings during clinical examination with lab, X-ray, and sometimes tissue samples to confirm the diagnosis[1].
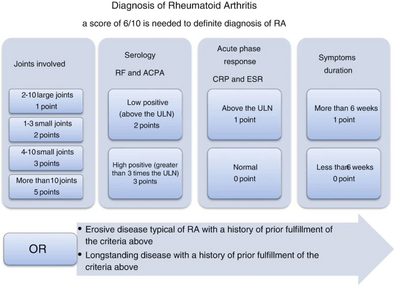
Rheumatoid arthritis In 1987, the American College of Rheumatology (ACR) introduced the initial classification criteria for RA, which required meeting 4 out of 7 criteria for over 6 weeks. Subsequently, a new classification criteria set was developed jointly by ACR/ EULAR in 2010. This updated criteria take in consideration the prognostic markers while maintaining high specificity and sensitivity. This allows for early patient identification and timely treatment with disease-modifying antirheumatic drugs DMARDs or inclusion in clinical trials for new therapies, enhancing care for those with early arthritis and enabling personalized treatment strategies[2].
Systemic Lupus Erythematosus Classification Criteria
In 2012, International Collaborating Clinics (SLICC) improved the 1997 criteria for categorizing lupus patients. These criteria help in research but aren't perfect for diagnosing patients. The new criteria are more sensitive (better at finding lupus cases) but less specific (may include some false positives). To be classified with lupus, a person must meet at least 4 out of 17 criteria, including one clinical and one immunologic sign. If a biopsy confirms lupus in the kidneys and there are positive autoantibodies, that's enough for classification[3].
Spondyloarthritis
Spondyloarthritis (SpA) includes diseases like ankylosing spondylitis (AS), psoriatic arthritis (PsA), reactive arthritis, enteropathic-related spondylitis. There are different criteria for diagnosing SpA, mainly used in research, but the latest from Assessment of SpondyloArthritis international Society suggests MRI is better for detecting early disease in the spine and sacroiliac area. They also defined inflammatory back pain and criteria for diagnosing axial and peripheral spondyloarthritis in early phases. ASAS introduced non-radiographic axial spondyloarthritis, which is similar to the radiographic form but lacks findings on plain X-rays and shows less ossification and inflammation on MRIs.
- Axial spondyloarthritis.jpg
Axial spondyloarthritis
- Peripheral spondyloarthritis.jpg
Peripheral spondyloarthritis
| Autoimmune | Autoinflammatory | Degenerative/ metabolic disorders |
|---|---|---|
|
|
Vitamin D deficiency/osteomalacia
|
Rheumatoid Arthritis and Osteoarthritis[edit | edit source]
| Rheumatoid Arthritis | Osteoarthritis |
|---|---|
|
|
References[edit | edit source]
- ↑ Hassan R, Faruqui H, Alquraa R, Eissa A, Alshaiki F, Cheikh M. Classification criteria and clinical practice guidelines for rheumatic diseases. Skills in Rheumatology. 2021:521.
- ↑ Britsemmer K, Ursum J, Gerritsen M, van Tuyl L, van Schaardenburg D. Validation of the 2010 ACR/EULAR classification criteria for rheumatoid arthritis: slight improvement over the 1987 ACR criteria. Annals of the rheumatic diseases. 2011 Aug 1;70(8):1468-70.
- ↑ Petri M, Orbai AM, Alarcon GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg DA, Wallace DJ, Nived O, Sturfelt GK. Derivation and validation of systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. In2011 ACR/ARHP Annual Meeting 2011 Nov 4 (pp. S669-S670). WILEY-BLACKWELL.