Subtalar Dislocation: Difference between revisions
Pieter Piron (talk | contribs) (Created page with " Subtalar dislocation<br> Search strategy<br>Search engines:<br>• Pubmed<br>• Web of knowledge (RCT’s)<br>• PEDro Key words: <br>Subtalar<br>dislocation<br>talar di...") |
Kim Jackson (talk | contribs) m (Kim Jackson moved page Subtalar dislocation to Subtalar Dislocation: Corrected Title) |
||
| (24 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Pieter Piron|Pieter Piron]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
=Definition/Description= | |||
[[File:Subtalar dislocation.jpg|thumb|Medial Subtalar Dislocation ]] | |||
Subtalar dislocation occurs through the disruption of 2 separate bony articulations: the talonavicular and talocalcaneal joints.<ref>Horning J, DiPreta J. Subtalar dislocation. Orthopedics. 2009 Dec 1;32(12).</ref> | |||
Subtalar dislocations are a rare ankle injury accounting for about 1%-2% of all joint dislocations. This injury occurs due to high-energy trauma, including falls, motor vehicle crashes, and sports injuries<ref>Bryant J, Levis JT. [https://escholarship.org/content/qt69r5p7g6/qt69r5p7g6.pdf?t=mprzjp Images in Emergency Medicine: Subtalar Dislocation]. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health. 2009;10(2).</ref>. The tightness of the joint capsule around the ankle and the strong connection of ligaments connecting the talus and the calcaneus explain the rarity of this injury<ref name=":4">Giannoulis D, Papadopoulos DV, Lykissas MG, Koulouvaris P, Gkiatas I, Mavrodontidis A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4390901/ Subtalar dislocation without associated fractures: Case report and review of literature.] World Journal of Orthopedics. 2015 Apr 18;6(3):374.</ref>. | |||
There are four types of subtalar dislocation according to Malaigne and Burger: medial, lateral, anterior, and posterior dislocations. This classification depends on the direction of the foot in relation to the talus at the time of injury. Medial subtalar dislocations predominate, accounting for approximately 80% of reported dislocations, and are known as acquired club foot, it happens when the foot is in plantarflexion and the lateral collateral ligaments are under stress when there is forceful inversion applied at the forefoot. Less common are lateral dislocations or acquired flat foot (15%-35%)<ref>Inokuchi S, Hashimoto T, Usami N. [https://pubmed.ncbi.nlm.nih.gov/9042888/ Posterior subtalar dislocation]. Journal of Trauma and Acute Care Surgery. 1997 Feb 1;42(2):310-3.</ref>, posterior dislocations (from 0.8% to 2.5%)<ref>Krishnan KM, Sinha AK. [https://pubmed.ncbi.nlm.nih.gov/14688779/ True posterior dislocation of subtalar joint: a case report.] The Journal of foot and ankle surgery. 2003 Nov 1;42(6):363-5..</ref>, and anterior dislocations (1%).<ref>Kanda T, Sakai H, Koseki K, Tamai K, Takeyama N, Saotome K. [https://journals.sagepub.com/doi/abs/10.1177/107110070102200715 Anterior dislocation of the subtalar joint: a case report.] Foot & Ankle International. 2001 Jul;22(7):609-11.</ref> | |||
It is common to be associated with [[Fracture|fractures]] of the malleoli, the talus, the calcaneus, or the fifth metatarsal<ref>Perugia D, Basile A, Massoni C, Gumina S, Rossi F, Ferretti A. [https://pubmed.ncbi.nlm.nih.gov/11954852/ Conservative treatment of subtalar dislocations]. International orthopaedics. 2002 Feb;26(1):56-60.</ref> and it is rare to find patients with an isolated subtalar dislocation<ref name=":4" />. Subtalar dislocation may result in a substantial deformity of the foot shape. | |||
=Clinically Relevant Anatomy= | |||
The [[Subtalar Joint|subtalar joint]] is a synovial joint between the [[talus]] and [[calcaneus]]. The facets of the talus and calcaneus alternate concave and convex. They are surrounded by strong ligaments that make this joint relatively stable.<ref name=":0">Jastifer JR, Gustafson PA. [https://pubmed.ncbi.nlm.nih.gov/25175840/ The subtalar joint: biomechanics and functional representations in the literature.] The foot. 2014 Dec 1;24(4):203-9.</ref> | |||
[[File:SubtalarJoint.PNG|thumb|Subtalar Joint]] | |||
Subtalar joint motion is complex because the axis of rotation is at an angle. Subtalar joint motion in open chain combines dorsiflexion/abduction/eversion and plantarflexion/adduction/inversion. In closed chain, these motions are referred to as pronation and supination.<ref name=":0" /> | |||
The most important ligament of the subtalar joint is the interosseus talocalcaneal ligament. There are four other weaker connections between the talus and calcaneus which are: the anterior talocalcaneal ligament, the posterior talocalcaneal ligament, lateral talocalcaneal ligament and the medial talocalcaneal ligament <ref>Drake R L, Vogl W, Mitchell A W M. Gray's anatomy for student. Philadelphia, USA: Elsevier Inc; 2005. p565-567</ref>. | |||
=Epidemiology/Etiology= | |||
Subtalar dislocations are usually seen when a person suffers a high-energy trauma such as falling from a height (20%) or road traffic accident (48%)<ref name=":1">Bibbo C, Anderson RB, Davis WH. [https://pubmed.ncbi.nlm.nih.gov/12627624/ Injury characteristics and the clinical outcome of subtalar dislocations: a clinical and radiographic analysis of 25 cases.] Foot & ankle international. 2003 Feb;24(2):158-63.</ref>. | |||
A dislocation of the subtalar joint usually occurs during plantar flexion and the injury is usually a closed injury<ref name=":2">Fotiadis E, Lyrtzis C, Svarnas T, Koimtzis M, Akritopoulou K, Chalidis B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2769472/ Closed subtalar dislocation with non-displaced fractures of talus and navicular: a case report and review of the literature]. Cases Journal. 2009 Dec;2(1):1-6.</ref>. If the foot lands on the ground while in inversion or eversion, this respectively results in a medial (80%) or a lateral (17%) subtalar dislocation. Anterior (1%) and posterior (2.5%) dislocations have also been examined and described but they are extremely rare<ref name=":1" />. | |||
== Risk Factors == | |||
* Bony or soft tissue dysplasia. | |||
* Impaired function of the [[Ankle Joint|ankle joint]]. | |||
* Aplasia of the [[Ankle Sprain|ankle ligaments]] or the calcaneus facets. | |||
* Hypoplasia of the malleoli. | |||
* Posttraumatic ligamentous insufficiency because of recurrent ankle sprain. | |||
* Atrophy of the peroneal muscles that predispose to this specific injury pattern. | |||
== Mechanism of Injury == | |||
'''Medial subtalar dislocations -''' result from forced inversion applied to a plantarflexed foot. | |||
During this position the neck of the talus will hinge and rotate around the sustentaculum tali as a pivot and this will cause a rupture of the lateral talonavicular joint capsule and ligaments, followed by the subtalar ligaments<ref name=":5">Sharma S, Patel S, Dhillon MS. [https://journals.lww.com/jaaosglobal/Fulltext/2021/12000/Subtalar_Dislocations.14.aspx Subtalar Dislocations.] JAAOS Global Research & Reviews. 2021 Dec;5(12).</ref>. Fracture of the posterior process of the talus is common to occur with medial dislocations. | |||
'''Lateral subtalar dislocations -''' result from forced eversion of a dorsiflexed foot during high-energy trauma. | |||
5. | During this position the head of the talus rotates around the anterior process of the calcaneus, this will result in rupture of talonavicular and subtalar ligaments and joint capsules<ref name=":5" />. Partial or complete rupture of the deltoid ligament may be presented with this injury because of the high-energy trauma. | ||
'''Posterior subtalar dislocations''' - result from forced plantar flexion of the foot. | |||
< | '''Anterior subtalar dislocations -''' result from anterior traction to the foot when the leg is in a fixed position. It is rare to find obvious foot deformity with posterior or anterior subtalar dislocations. | ||
{{#ev:youtube|LyGxuXLkxSA}}<ref>nabil ebraheim. Subtalar Dislocation - Everything You Need To Know - Dr. Nabil Ebraheim | |||
. Available from: http://www.youtube.com/watch?v=LyGxuXLkxSA [last accessed 21/4/2022]</ref> | |||
=Diagnostic Procedures= | |||
[[File:Lateral subtalar dislocation.jpeg|thumb|350x350px|Lateral subtalar dislocation+ lat malleoli fracture]] | |||
Patients with a subtalar dislocation present with increased of pain and inability to fully weight bear on the affected foot. | |||
A clear deformity of the ankle can be seen. The talar head can stick out prominently and the talonavicular and medial subtalar joints are very tender and painful to palpate. | |||
A CT scan is usually performed to determine the type of injury<ref name=":2" />. In 88% of all patients, an associated foot and ankle injury also occurs. [[Ankle Joint|Ankle]], talar, [[Calcaneal Fractures|calcaneal]] and [[navicular]] bones run the highest risk of being fractured. The [[cuneiforms]], [[cuboid]], and [[metatarsals]] may also be injured. All parts of the foot that could be damaged due to a subtalar dislocation have to be examined radiographically<ref name=":1" />. | |||
=Medical Management= | |||
Subtalar dislocations require reduction under general anaesthesia by manual pressure and traction. Talus relocation is performed with the knee flexed to reduce the tension of the [[soleus]] and [[gastrocnemius]] muscles. | |||
Subsequently, the subtalar instability is evaluated by the use of [[Medical Imaging|fluoroscopy]]. | |||
Pure dislocations (those without concomitant fractures) usually have a more favourable prognosis<ref name=":2" />. There is not consensus on how or how long the ankle should be immobilized after dislocation. Studies show a range of immobilization times from 3 to 8 weeks depending on concomitant injuries<ref name=":2" />. | |||
=Physical Therapy Implications= | |||
Due to the rate of occurrence, most studies of subtalar dislocations include patients with a medial dislocation. | |||
Some studies have shown early mobilisation after uncomplicated medial subtalar dislocation assists patients in returning to daily function in 2 months<ref name=":3">Lasanianos NG, Lyras DN, Mouzopoulos G, Tsutseos N, Garnavos C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3052431/ Early mobilization after uncomplicated medial subtalar dislocation provides successful functional results.] Journal of Orthopaedics and Traumatology. 2011 Mar;12(1):37-43.</ref>. | |||
Physical therapy can be started when early mobilisation is allowed after the immobilisation period is complete approximately, 2-3 weeks after reduction. The purpose of physical therapy at this time is to reduce swelling, increase range of motion and prevent muscle shortening<ref name=":3" />. | |||
According to this study, in week 3 after injury active range of motion exercises for the ankle, foot, and muscle-strengthening exercises were started. After the third week, patients started with partial-weight-bearing exercises and progressed to full weight-bearing at week five. The exercises for full weight-bearing were performed using a below the knee functional ankle brace. This brace allowed plantar- and dorsiflexion but inhibited inversion and eversion movements. | |||
This study concluded that all patients regained a normal ankle ROM (evaluated by a [[goniometer]]). The mean percentage of ankle ROM between the injured and healthy lower limb was 92.5% which was considered very satisfactory by both physiotherapists and patients. The mean AOFAS ankle-hindfoot scale (American Orthopaedic Foot and Ankle Society) score was 90.75 points (range: 82-97). AOFAS ankle-hindfoot scale scores pain, function, and alignment. 3 years post-reductive, no radiographic evidence of arthritis or avascular necrosis of the talus was detected. Two patients complained of mild pain in the hindfoot.<ref name=":3" /> | |||
It should be noted that this study may not be applicable to all medial subtalar dislocations and that surgical consultant protocol may vary between consultants. | |||
= References: = | |||
<references /> | |||
[[Category:Ankle]] | |||
[[Category:Foot]] | |||
[[Category:Conditions]] [[Category:Ankle - Conditions]] | |||
[[Category:Foot - Conditions]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
Latest revision as of 12:10, 23 September 2022
Definition/Description[edit | edit source]
Subtalar dislocation occurs through the disruption of 2 separate bony articulations: the talonavicular and talocalcaneal joints.[1]
Subtalar dislocations are a rare ankle injury accounting for about 1%-2% of all joint dislocations. This injury occurs due to high-energy trauma, including falls, motor vehicle crashes, and sports injuries[2]. The tightness of the joint capsule around the ankle and the strong connection of ligaments connecting the talus and the calcaneus explain the rarity of this injury[3].
There are four types of subtalar dislocation according to Malaigne and Burger: medial, lateral, anterior, and posterior dislocations. This classification depends on the direction of the foot in relation to the talus at the time of injury. Medial subtalar dislocations predominate, accounting for approximately 80% of reported dislocations, and are known as acquired club foot, it happens when the foot is in plantarflexion and the lateral collateral ligaments are under stress when there is forceful inversion applied at the forefoot. Less common are lateral dislocations or acquired flat foot (15%-35%)[4], posterior dislocations (from 0.8% to 2.5%)[5], and anterior dislocations (1%).[6]
It is common to be associated with fractures of the malleoli, the talus, the calcaneus, or the fifth metatarsal[7] and it is rare to find patients with an isolated subtalar dislocation[3]. Subtalar dislocation may result in a substantial deformity of the foot shape.
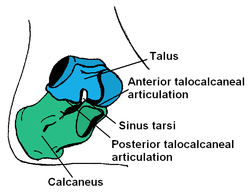
Clinically Relevant Anatomy[edit | edit source]
The subtalar joint is a synovial joint between the talus and calcaneus. The facets of the talus and calcaneus alternate concave and convex. They are surrounded by strong ligaments that make this joint relatively stable.[8]
Subtalar joint motion is complex because the axis of rotation is at an angle. Subtalar joint motion in open chain combines dorsiflexion/abduction/eversion and plantarflexion/adduction/inversion. In closed chain, these motions are referred to as pronation and supination.[8]
The most important ligament of the subtalar joint is the interosseus talocalcaneal ligament. There are four other weaker connections between the talus and calcaneus which are: the anterior talocalcaneal ligament, the posterior talocalcaneal ligament, lateral talocalcaneal ligament and the medial talocalcaneal ligament [9].
Epidemiology/Etiology[edit | edit source]
Subtalar dislocations are usually seen when a person suffers a high-energy trauma such as falling from a height (20%) or road traffic accident (48%)[10].
A dislocation of the subtalar joint usually occurs during plantar flexion and the injury is usually a closed injury[11]. If the foot lands on the ground while in inversion or eversion, this respectively results in a medial (80%) or a lateral (17%) subtalar dislocation. Anterior (1%) and posterior (2.5%) dislocations have also been examined and described but they are extremely rare[10].
Risk Factors[edit | edit source]
- Bony or soft tissue dysplasia.
- Impaired function of the ankle joint.
- Aplasia of the ankle ligaments or the calcaneus facets.
- Hypoplasia of the malleoli.
- Posttraumatic ligamentous insufficiency because of recurrent ankle sprain.
- Atrophy of the peroneal muscles that predispose to this specific injury pattern.
Mechanism of Injury[edit | edit source]
Medial subtalar dislocations - result from forced inversion applied to a plantarflexed foot.
During this position the neck of the talus will hinge and rotate around the sustentaculum tali as a pivot and this will cause a rupture of the lateral talonavicular joint capsule and ligaments, followed by the subtalar ligaments[12]. Fracture of the posterior process of the talus is common to occur with medial dislocations.
Lateral subtalar dislocations - result from forced eversion of a dorsiflexed foot during high-energy trauma.
During this position the head of the talus rotates around the anterior process of the calcaneus, this will result in rupture of talonavicular and subtalar ligaments and joint capsules[12]. Partial or complete rupture of the deltoid ligament may be presented with this injury because of the high-energy trauma.
Posterior subtalar dislocations - result from forced plantar flexion of the foot.
Anterior subtalar dislocations - result from anterior traction to the foot when the leg is in a fixed position. It is rare to find obvious foot deformity with posterior or anterior subtalar dislocations.
Diagnostic Procedures[edit | edit source]
Patients with a subtalar dislocation present with increased of pain and inability to fully weight bear on the affected foot.
A clear deformity of the ankle can be seen. The talar head can stick out prominently and the talonavicular and medial subtalar joints are very tender and painful to palpate.
A CT scan is usually performed to determine the type of injury[11]. In 88% of all patients, an associated foot and ankle injury also occurs. Ankle, talar, calcaneal and navicular bones run the highest risk of being fractured. The cuneiforms, cuboid, and metatarsals may also be injured. All parts of the foot that could be damaged due to a subtalar dislocation have to be examined radiographically[10].
Medical Management[edit | edit source]
Subtalar dislocations require reduction under general anaesthesia by manual pressure and traction. Talus relocation is performed with the knee flexed to reduce the tension of the soleus and gastrocnemius muscles.
Subsequently, the subtalar instability is evaluated by the use of fluoroscopy.
Pure dislocations (those without concomitant fractures) usually have a more favourable prognosis[11]. There is not consensus on how or how long the ankle should be immobilized after dislocation. Studies show a range of immobilization times from 3 to 8 weeks depending on concomitant injuries[11].
Physical Therapy Implications[edit | edit source]
Due to the rate of occurrence, most studies of subtalar dislocations include patients with a medial dislocation.
Some studies have shown early mobilisation after uncomplicated medial subtalar dislocation assists patients in returning to daily function in 2 months[14].
Physical therapy can be started when early mobilisation is allowed after the immobilisation period is complete approximately, 2-3 weeks after reduction. The purpose of physical therapy at this time is to reduce swelling, increase range of motion and prevent muscle shortening[14].
According to this study, in week 3 after injury active range of motion exercises for the ankle, foot, and muscle-strengthening exercises were started. After the third week, patients started with partial-weight-bearing exercises and progressed to full weight-bearing at week five. The exercises for full weight-bearing were performed using a below the knee functional ankle brace. This brace allowed plantar- and dorsiflexion but inhibited inversion and eversion movements.
This study concluded that all patients regained a normal ankle ROM (evaluated by a goniometer). The mean percentage of ankle ROM between the injured and healthy lower limb was 92.5% which was considered very satisfactory by both physiotherapists and patients. The mean AOFAS ankle-hindfoot scale (American Orthopaedic Foot and Ankle Society) score was 90.75 points (range: 82-97). AOFAS ankle-hindfoot scale scores pain, function, and alignment. 3 years post-reductive, no radiographic evidence of arthritis or avascular necrosis of the talus was detected. Two patients complained of mild pain in the hindfoot.[14]
It should be noted that this study may not be applicable to all medial subtalar dislocations and that surgical consultant protocol may vary between consultants.
References:[edit | edit source]
- ↑ Horning J, DiPreta J. Subtalar dislocation. Orthopedics. 2009 Dec 1;32(12).
- ↑ Bryant J, Levis JT. Images in Emergency Medicine: Subtalar Dislocation. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health. 2009;10(2).
- ↑ 3.0 3.1 Giannoulis D, Papadopoulos DV, Lykissas MG, Koulouvaris P, Gkiatas I, Mavrodontidis A. Subtalar dislocation without associated fractures: Case report and review of literature. World Journal of Orthopedics. 2015 Apr 18;6(3):374.
- ↑ Inokuchi S, Hashimoto T, Usami N. Posterior subtalar dislocation. Journal of Trauma and Acute Care Surgery. 1997 Feb 1;42(2):310-3.
- ↑ Krishnan KM, Sinha AK. True posterior dislocation of subtalar joint: a case report. The Journal of foot and ankle surgery. 2003 Nov 1;42(6):363-5..
- ↑ Kanda T, Sakai H, Koseki K, Tamai K, Takeyama N, Saotome K. Anterior dislocation of the subtalar joint: a case report. Foot & Ankle International. 2001 Jul;22(7):609-11.
- ↑ Perugia D, Basile A, Massoni C, Gumina S, Rossi F, Ferretti A. Conservative treatment of subtalar dislocations. International orthopaedics. 2002 Feb;26(1):56-60.
- ↑ 8.0 8.1 Jastifer JR, Gustafson PA. The subtalar joint: biomechanics and functional representations in the literature. The foot. 2014 Dec 1;24(4):203-9.
- ↑ Drake R L, Vogl W, Mitchell A W M. Gray's anatomy for student. Philadelphia, USA: Elsevier Inc; 2005. p565-567
- ↑ 10.0 10.1 10.2 Bibbo C, Anderson RB, Davis WH. Injury characteristics and the clinical outcome of subtalar dislocations: a clinical and radiographic analysis of 25 cases. Foot & ankle international. 2003 Feb;24(2):158-63.
- ↑ 11.0 11.1 11.2 11.3 Fotiadis E, Lyrtzis C, Svarnas T, Koimtzis M, Akritopoulou K, Chalidis B. Closed subtalar dislocation with non-displaced fractures of talus and navicular: a case report and review of the literature. Cases Journal. 2009 Dec;2(1):1-6.
- ↑ 12.0 12.1 Sharma S, Patel S, Dhillon MS. Subtalar Dislocations. JAAOS Global Research & Reviews. 2021 Dec;5(12).
- ↑ nabil ebraheim. Subtalar Dislocation - Everything You Need To Know - Dr. Nabil Ebraheim . Available from: http://www.youtube.com/watch?v=LyGxuXLkxSA [last accessed 21/4/2022]
- ↑ 14.0 14.1 14.2 Lasanianos NG, Lyras DN, Mouzopoulos G, Tsutseos N, Garnavos C. Early mobilization after uncomplicated medial subtalar dislocation provides successful functional results. Journal of Orthopaedics and Traumatology. 2011 Mar;12(1):37-43.