Ruptured Spleen: Difference between revisions
mNo edit summary |
Kim Jackson (talk | contribs) mNo edit summary |
||
| (46 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- Nick Hansen & Ren Peterson [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''- [[User:Nick Hansen|Nick Hansen]] & [[User:Ren Peterson|Ren Peterson]] [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Illu spleen.jpg|right|frameless|389x389px]] | |||
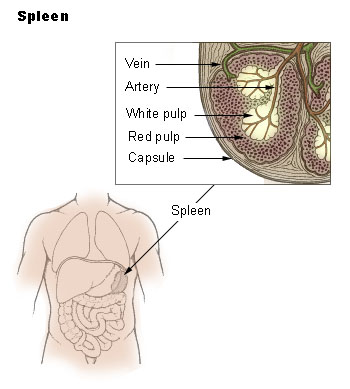
The spleen is a significant organ of the hematologic and reticuloendothelial systems<ref name=":0" />. | |||
* An intraperitoneal organ located anatomically behind the 9 and 11 ribs on the left side of the body, under the [[Ribs|rib]] cage and [[Muscles of Respiration|diaphragm]] (left upper quadrant). | |||
* An organ of the [[Lymphatic System|lymphatic system]] | |||
* About the size of a fist | |||
* Primary roles are filtering the body’s [[blood]], helps to fight [[Infectious Disease|infection]] and serves a role in storing and releasing certain types of [[Immune System|immune]] cells that mediate tissue inflammation. | |||
Rupture of the spleen can lead to life-threatening bleeding into the abdominal cavity, which will lead to low blood pressure and decreased oxygen supply to the [[Anatomy of the Human Heart|heart]] and [[Brain Anatomy|brain]]. It is a medical emergency and should be referred to the emergency room immediately | |||
This great 90 second video (by physiotherapists) gives a great summary of the condition.{{#ev:youtube|https://www.youtube.com/watch?v=gip3fDb5O3E}}<ref name=":1">Mike Flores Physical therapy management - ruptured spleen Available from https://www.youtube.com/watch?v=gip3fDb5O3E</ref>. | |||
== Function of the Spleen == | |||
In utero, the spleen is partially responsible for hemoglobin synthesis from the 10th through the 25th week of pregnancy. | |||
After birth, the primary function of the spleen shifts to the following major roles: | |||
# Filtration of erythrocytes and platelets. Young, flexible red blood cells pass through the epithelial cells of the splenic cords and continue through [[blood]] flow. On the other hand, older, larger, and deformed red blood cells are trapped by the splenic cords and phagocytosed by macrophages waiting on the reticulum and sinus endothelium. | |||
# Iron metabolism. Splenic macrophages recycle iron from the breakdown of senescent and damaged red blood cells (either store ingested iron in their cytoplasm or export it via ferritin into the bloodstream). | |||
# Prevention of infection. Occurs by two major mechanisms: Phagocytic filtration of the bloodstream (macrophages supervise the flow of red blood cells, platelets, as well as microorganisms through the splenic cords); Production of opsonizing antibodies ie the process at which opsonins bind to the surface of the antigen so that the antigen will be readily identified and engulfed by phagocytes for destruction. After opsonization, macrophages, dendritic cells, and neutrophils phagocytose the antigen. Opsonization is essential to clear particular microorganisms like encapsulated bacteria and intra-erythrocytic parasites. The spleen is the largest secondary lymphoid organ in an adult human | |||
# Red blood cell and platelet storage: As a reservoir for blood, the spleen weights about 100 g. It can respond to sympathetic stimulation by contracting its fibroelastic capsule and trabeculae to increase systemic blood supply (this vital function takes place during hemorrhage). About 25% to 30% of red blood cells (RBCs) are stored in the spleen, along with about 25% of platelets normally sequestered in the spleen<ref name=":0">Kapila V, Tuma F. Physiology, [https://www.ncbi.nlm.nih.gov/books/NBK537307/ Spleen]. InStatPearls [Internet] 2020 Mar 26. StatPearls Publishing.Available from;https://www.ncbi.nlm.nih.gov/books/NBK537307/ (accessed 1.12.2020)</ref>. | |||
== Etiology == | |||
[[File:Atraumatic_Schematic.png|right|frameless|600x600px]] | |||
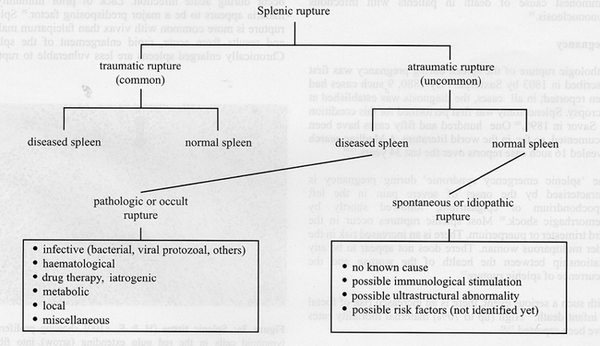
Splenic rupture: divided into two major categories: traumatic and non-traumatic rupture. | |||
# Traumatic: most prevalent major mechanism in traumatic injury (50% to 75%) is the result of motor vehicle injury. Direct abdominal blows and falls are the remaining major causes of traumatic rupture. Can present immediately after an injury or may present in a delayed fashion. | |||
# Non-traumatic splenic rupture: is very uncommon, though can be related to underlying pathologic conditions or may be idiopathic. However, non-traumatic rupture, when it does happen, carries a mortality of around 12%. One often cited example of spontaneous splenic rupture, which occurs in only 0.1 percent of patients with this condition, is related to infection with [[Epstein-Barr Virus|Infectious Mononucleosis also known as Epstein-Barr Virus]](Incidence of trauma in the presence of a diagnosis of infectious mononucleosis places one with an increased risk of a ruptured spleen<ref name=":0" /><ref name="p0">About Infectious Mononucleosis. Centers for Disease Control and Prevention. https://www.cdc.gov/epstein-barr/about-mono.html. Published September 14, 2016. Accessed April 5, 2017</ref>) | |||
3 minute Video demonstrating traumatic force required to rupture a spleen and its relevance to some sporting codes:{{#ev:youtube|uQp9iwVzN5Q|300}}<ref>How Much Force to Rupture a Spleen: Sport Science. Available from: http://www.youtube.com/watch?v=uQp9iwVzN5Q [last accessed 30 November 2020]</ref> | |||
== Epidemiology == | |||
The prevalence of splenic ruptures is not widely reported in the literature. | |||
* The mechanism of the majority of traumatic ruptures continues to be motor vehicle injury, followed by direct abdominal blows. Sports such as football, hockey, and bicycling increase the risk of [[Abdominal Muscles|abdominal]], and, therefore, splenic injury and rupture. One study suggests that traumatic splenic ruptures are more likely to occur in males (2:1 male to female) in ages ranging from 18 to 34 years. | |||
The | * The following are six major causes of non-traumatic rupture: [[Oncology|Neoplasm]], 30%; [[Infectious Disease|Infectious]], 30%; [[Autoimmune Disorders|Inflammatory disease]], 15%; Medication and medical treatment, 10%; Mechanical causes, 7%; Idiopathic, 7%<ref name=":0" /> | ||
Of Note: [[Pancreatitis]] may lead to atraumatic splenic rupture; Domestic violence should be among the considerations in evaluating patients with splenic rupture; [[Malaria]] also remains a risk factor for splenic rupture in countries where this disease is prevalent<ref name=":0" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Signs and symptoms of a ruptured spleen include: <ref name="Mayo Clinic">Mayo Clinic<br>http://www.mayoclinic.com/health/ruptured-spleen/DS00872 </ref> | |||
* Pain (usually severe but not always) in the upper left portion of the stomach (abdomen) or under rib cage. | |||
* Tenderness when you touch the upper left portion of the stomach (abdomen). | |||
* Left shoulder pain ([[Kehr’s Sign]]) - Pain in the left shoulder caused by irritation of the undersurface of the diaphragm by blood leaking from a ruptured spleen. The pain impulses are referred along the phrenic nerve supplying the diaphragm C3-C5 nerve distribution. <ref name="Dictionary of Nursing">A Dictionary of Nursing. 2008. Kehr’s Sign. 29 Mar. 2012 Available at: http://www.encyclopedia.com/doc/1O62-Kehrssign.html.</ref> | |||
*Video of Kehr’s Sign: | *Video of Kehr’s Sign: | ||
{{#ev:youtube|UkXghZn2WJ8}} | {{#ev:youtube|UkXghZn2WJ8}}<ref>Med School Made Easy Kehr Sign - Spleen Exam Available from https://www.youtube.com/watch?v=UkXghZn2WJ8</ref> | ||
* Internal Bleeding occurs secondary to a ruptured spleen and can cause [[Blood Pressure|blood pressure]] to drop ([[hypotension]]). This can lead to: <ref name="WebMD">WebMD. 2005-2012. Ruptured Spleen. [Internet] [reviewed 2009 Aug 19; cited 2012 Mar 30]. Available from: http://www.webmd.com/digestive-disorders/ruptured-spleen</ref> | |||
** Blurred vision | |||
** confusion | |||
** Light-headedness | |||
*Blurred vision | ** Fainting and signs of shock (cold clammy skin, pallor, nausea, vomiting, and weak and/or rapid pulse) | ||
* | |||
*Light-headedness | |||
*Fainting | |||
< | * Splenic Inflammation '''-''' This can be identified by performing the '''[[Castell’s Percussion Test]]''': Patient is positioned in supine lying. The clinician palpates the left costal margin near the anterior axillary line and then instructs the patient to breathe normally while applying percussion at both full inspiration as well as at rest. | ||
** Findings: Positive test if the dull sound is present upon full inspiration and expiration. (Indicates spleen descending). Normal it is only dull at full inspiration and should be tympanic at rest. Important: If the spleen is found to be inflamed, DO NOT continue to palpate as it can lead to a rupture. <ref name="p8">Examination of the Spleen. Examination of the Spleen | Stanford Medicine 25 | Stanford Medicine. http://stanfordmedicine25.stanford.edu/the25/spleen.html. Accessed April 4, 2017.</ref> | |||
'''Clinical Pearl:''' It is strongly advised to seek immediate medical care if an injury is sustained coupled with pain in the left upper stomach (abdomen) region along with any of the above-listed signs and symptoms. If severe injuries are untreated a ruptured spleen can be fatal. | |||
== Treatment/Management == | |||
Treatment is dependent on the severity and etiology of rupture, as well as the hemodynamic stability of the patient. | |||
* Non-operative treatment is attempted in 60% to 90% of patients with blunt traumatic splenic injuries out of a desire to preserve splenic function. Non-operative management is the main management option, particularly in the pediatric population. Current success rates of 90% are reported in pediatric populations. | |||
* Interventional radiology may be available at some institutions as a means to perform arterial embolization for large or small vessel injuries with bleeding in stable trauma patients. This is also an option in patients who fail conservative management. | |||
* Exploratory laparotomy indicated if continuing hemodynamic instability or if the patient has required more than 4 units of blood during a 48-hour period. The initial choice in surgical management is to repair any capsular lacerations (splenorrhaphy). If extensive injury or uncontrolled hemorrhage is present, splenectomy is warranted. | |||
* Post-splenectomy [[Vaccines|vaccinations]] are intended to address encapsulated organisms ( Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitides.). Children who have a splenectomy are generally recommended to take phenoxymethylpenicillin (Pen VK) until they are 5 years old, though the recommended duration of this prophylaxis varies. This is based on a prior study of [[Sickle Cell Anemia|sickle cell]] patients.<ref name=":0" /> | |||
Non- | |||
* | |||
* | |||
* | |||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
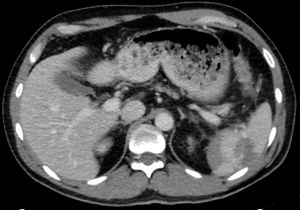
[[File:Spleen Rupture.jpg|alt=CT Ruptured spleen|CT Ruptured spleen|right|frameless]]A splenic injury may not always be clinically apparent, and spontaneous splenic rupture or pathologic splenic rupture can occur after negligible trauma or insignificant events. | |||
* [[Ultrasound Scans|Ultrasound]]: helpful and highly accurate in the diagnosis of significant splenic injury but is limited in detecting active bleeding, pseudoaneurysm, or early in the evaluation when blood loss is minimal. Ultrasound at the bedside in the emergency department has been able to visualize as little as 100 mL of free fluid in the abdomen with 90% sensitivity. | |||
* [[CT Scans|CT]] has become the mainstay of stable patient evaluation since it can provide splenic injury severity and assessment of other abdominal organs. An intraparenchymal or subcapsular hematoma is also easier to identify and may be associated with delayed splenic rupture. | |||
Splenic injury is classified based on CT findings according to the American Association for the Surgery of Trauma (AAST) Organ Injury Scale. It helps categorizes splenic injuries but does not predict the need for surgical intervention<ref name=":0" />. | |||
== Physical Therapy Management == | |||
The physical therapist must be able to recognize the signs and symptoms of spleen rupture. In [[Sport Injury Classification|sport]]<nowiki/>s, splenic rupture is the most common cause of death due to abdominal trauma, it is vital that clinicians perform a thorough examination of the patient.<ref name="Shultz">Shultz SJ, Houglum PA, Perrin DH. Examination of Musculoskeletal Injuries, 2nd ed. Champaign, IL, 2005. p. 570-571</ref> | |||
* '''Palpation:''' The spleen is located in the left upper quadrant and covered by the 9th - 11th ribs. Clinicians should check this area for pain and tenderness. Abdominal palpation should also be performed in the hook-lying position checking for tenderness, distension, guarding, and rebound tenderness. "To palpate the spleen, lift the left flank with your non-dominant hand; keeping your other hand flat, depress the palpating digits just below and anterior to the 11th and 12 ribs and ask the patient to take a deep breath. A normal healthy spleen should not be palpable." <ref name="Shultz" /> | |||
* '''Patient Education:''' Most splenic ruptures can be rapidly progressing, while others can delay haemorrhage for hours, days, or even weeks after injury until a sufficient enough force causes a rupture. It is vital that we educate patients about the signs and symptoms so they can seek medical care immediately. | |||
* '''Post-operation:''' Encourage ROM, ambulation, and coughing techniques (splinted coughing). Most traumatic splenic ruptures will not be seen in physical therapy. | |||
[[ | |||
< | |||
'''Palpation:''' The spleen is located in the left upper quadrant and covered by the 9th - 11th ribs. Clinicians should check this area for pain and tenderness. Abdominal palpation should also be performed in the hook-lying position checking for tenderness, distension, guarding, and rebound tenderness. "To palpate the spleen, lift the left flank with your non-dominant hand; keeping your other hand flat, depress the palpating digits just below and anterior to the 11th and 12 ribs and ask the patient to take a deep breath. A normal healthy spleen should not be palpable." <ref name="Shultz" /> | |||
'''Patient Education:''' Most splenic ruptures can be rapidly progressing, while others can delay | |||
'''Post-operation''' | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* Left kidney trauma/pathology | |||
* [[Rib Fracture|Rib fracture]] | |||
* Intestinal pathology | |||
* Musculoskeletal Involvement | |||
* [[Non-Hodgkin's Lymphoma]] | |||
*[[Epstein-Barr Virus|Infectious Mononucleosis aka Epstein-Barr Virus]] | |||
== Case Report/ Case Study == | |||
[http://www.ncbi.nlm.nih.gov/pubmed/7572867 Spontaneous rupture of the spleen – a fatal complication of pregnancy] | |||
== Case | |||
http://www.ncbi.nlm.nih.gov/pubmed/7572867 | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] [[Category:Medical]] [[Category:Sports_Injuries]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Medical]] | |||
[[Category:Sports_Injuries]] | |||
[[Category:Primary Contact]] | |||
[[Category:Conditions]] | |||
Latest revision as of 17:25, 2 January 2021
Original Editors - Nick Hansen & Ren Peterson from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Nicholaus Hansen, Taylor Hutchison, Vidya Acharya, Kim Jackson, Michael Flores, Lucinda hampton, Admin, Elaine Lonnemann, Claire Knott, 127.0.0.1, WikiSysop, Wendy Walker and Naomi O'Reilly
Introduction[edit | edit source]
The spleen is a significant organ of the hematologic and reticuloendothelial systems[1].
- An intraperitoneal organ located anatomically behind the 9 and 11 ribs on the left side of the body, under the rib cage and diaphragm (left upper quadrant).
- An organ of the lymphatic system
- About the size of a fist
- Primary roles are filtering the body’s blood, helps to fight infection and serves a role in storing and releasing certain types of immune cells that mediate tissue inflammation.
Rupture of the spleen can lead to life-threatening bleeding into the abdominal cavity, which will lead to low blood pressure and decreased oxygen supply to the heart and brain. It is a medical emergency and should be referred to the emergency room immediately
This great 90 second video (by physiotherapists) gives a great summary of the condition.
[2].
Function of the Spleen[edit | edit source]
In utero, the spleen is partially responsible for hemoglobin synthesis from the 10th through the 25th week of pregnancy.
After birth, the primary function of the spleen shifts to the following major roles:
- Filtration of erythrocytes and platelets. Young, flexible red blood cells pass through the epithelial cells of the splenic cords and continue through blood flow. On the other hand, older, larger, and deformed red blood cells are trapped by the splenic cords and phagocytosed by macrophages waiting on the reticulum and sinus endothelium.
- Iron metabolism. Splenic macrophages recycle iron from the breakdown of senescent and damaged red blood cells (either store ingested iron in their cytoplasm or export it via ferritin into the bloodstream).
- Prevention of infection. Occurs by two major mechanisms: Phagocytic filtration of the bloodstream (macrophages supervise the flow of red blood cells, platelets, as well as microorganisms through the splenic cords); Production of opsonizing antibodies ie the process at which opsonins bind to the surface of the antigen so that the antigen will be readily identified and engulfed by phagocytes for destruction. After opsonization, macrophages, dendritic cells, and neutrophils phagocytose the antigen. Opsonization is essential to clear particular microorganisms like encapsulated bacteria and intra-erythrocytic parasites. The spleen is the largest secondary lymphoid organ in an adult human
- Red blood cell and platelet storage: As a reservoir for blood, the spleen weights about 100 g. It can respond to sympathetic stimulation by contracting its fibroelastic capsule and trabeculae to increase systemic blood supply (this vital function takes place during hemorrhage). About 25% to 30% of red blood cells (RBCs) are stored in the spleen, along with about 25% of platelets normally sequestered in the spleen[1].
Etiology[edit | edit source]
Splenic rupture: divided into two major categories: traumatic and non-traumatic rupture.
- Traumatic: most prevalent major mechanism in traumatic injury (50% to 75%) is the result of motor vehicle injury. Direct abdominal blows and falls are the remaining major causes of traumatic rupture. Can present immediately after an injury or may present in a delayed fashion.
- Non-traumatic splenic rupture: is very uncommon, though can be related to underlying pathologic conditions or may be idiopathic. However, non-traumatic rupture, when it does happen, carries a mortality of around 12%. One often cited example of spontaneous splenic rupture, which occurs in only 0.1 percent of patients with this condition, is related to infection with Infectious Mononucleosis also known as Epstein-Barr Virus(Incidence of trauma in the presence of a diagnosis of infectious mononucleosis places one with an increased risk of a ruptured spleen[1][3])
3 minute Video demonstrating traumatic force required to rupture a spleen and its relevance to some sporting codes:
Epidemiology[edit | edit source]
The prevalence of splenic ruptures is not widely reported in the literature.
- The mechanism of the majority of traumatic ruptures continues to be motor vehicle injury, followed by direct abdominal blows. Sports such as football, hockey, and bicycling increase the risk of abdominal, and, therefore, splenic injury and rupture. One study suggests that traumatic splenic ruptures are more likely to occur in males (2:1 male to female) in ages ranging from 18 to 34 years.
- The following are six major causes of non-traumatic rupture: Neoplasm, 30%; Infectious, 30%; Inflammatory disease, 15%; Medication and medical treatment, 10%; Mechanical causes, 7%; Idiopathic, 7%[1]
Of Note: Pancreatitis may lead to atraumatic splenic rupture; Domestic violence should be among the considerations in evaluating patients with splenic rupture; Malaria also remains a risk factor for splenic rupture in countries where this disease is prevalent[1]
Characteristics/Clinical Presentation[edit | edit source]
Signs and symptoms of a ruptured spleen include: [5]
- Pain (usually severe but not always) in the upper left portion of the stomach (abdomen) or under rib cage.
- Tenderness when you touch the upper left portion of the stomach (abdomen).
- Left shoulder pain (Kehr’s Sign) - Pain in the left shoulder caused by irritation of the undersurface of the diaphragm by blood leaking from a ruptured spleen. The pain impulses are referred along the phrenic nerve supplying the diaphragm C3-C5 nerve distribution. [6]
- Video of Kehr’s Sign:
- Internal Bleeding occurs secondary to a ruptured spleen and can cause blood pressure to drop (hypotension). This can lead to: [8]
- Blurred vision
- confusion
- Light-headedness
- Fainting and signs of shock (cold clammy skin, pallor, nausea, vomiting, and weak and/or rapid pulse)
- Splenic Inflammation - This can be identified by performing the Castell’s Percussion Test: Patient is positioned in supine lying. The clinician palpates the left costal margin near the anterior axillary line and then instructs the patient to breathe normally while applying percussion at both full inspiration as well as at rest.
- Findings: Positive test if the dull sound is present upon full inspiration and expiration. (Indicates spleen descending). Normal it is only dull at full inspiration and should be tympanic at rest. Important: If the spleen is found to be inflamed, DO NOT continue to palpate as it can lead to a rupture. [9]
Clinical Pearl: It is strongly advised to seek immediate medical care if an injury is sustained coupled with pain in the left upper stomach (abdomen) region along with any of the above-listed signs and symptoms. If severe injuries are untreated a ruptured spleen can be fatal.
Treatment/Management[edit | edit source]
Treatment is dependent on the severity and etiology of rupture, as well as the hemodynamic stability of the patient.
- Non-operative treatment is attempted in 60% to 90% of patients with blunt traumatic splenic injuries out of a desire to preserve splenic function. Non-operative management is the main management option, particularly in the pediatric population. Current success rates of 90% are reported in pediatric populations.
- Interventional radiology may be available at some institutions as a means to perform arterial embolization for large or small vessel injuries with bleeding in stable trauma patients. This is also an option in patients who fail conservative management.
- Exploratory laparotomy indicated if continuing hemodynamic instability or if the patient has required more than 4 units of blood during a 48-hour period. The initial choice in surgical management is to repair any capsular lacerations (splenorrhaphy). If extensive injury or uncontrolled hemorrhage is present, splenectomy is warranted.
- Post-splenectomy vaccinations are intended to address encapsulated organisms ( Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitides.). Children who have a splenectomy are generally recommended to take phenoxymethylpenicillin (Pen VK) until they are 5 years old, though the recommended duration of this prophylaxis varies. This is based on a prior study of sickle cell patients.[1]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
A splenic injury may not always be clinically apparent, and spontaneous splenic rupture or pathologic splenic rupture can occur after negligible trauma or insignificant events.
- Ultrasound: helpful and highly accurate in the diagnosis of significant splenic injury but is limited in detecting active bleeding, pseudoaneurysm, or early in the evaluation when blood loss is minimal. Ultrasound at the bedside in the emergency department has been able to visualize as little as 100 mL of free fluid in the abdomen with 90% sensitivity.
- CT has become the mainstay of stable patient evaluation since it can provide splenic injury severity and assessment of other abdominal organs. An intraparenchymal or subcapsular hematoma is also easier to identify and may be associated with delayed splenic rupture.
Splenic injury is classified based on CT findings according to the American Association for the Surgery of Trauma (AAST) Organ Injury Scale. It helps categorizes splenic injuries but does not predict the need for surgical intervention[1].
Physical Therapy Management[edit | edit source]
The physical therapist must be able to recognize the signs and symptoms of spleen rupture. In sports, splenic rupture is the most common cause of death due to abdominal trauma, it is vital that clinicians perform a thorough examination of the patient.[10]
- Palpation: The spleen is located in the left upper quadrant and covered by the 9th - 11th ribs. Clinicians should check this area for pain and tenderness. Abdominal palpation should also be performed in the hook-lying position checking for tenderness, distension, guarding, and rebound tenderness. "To palpate the spleen, lift the left flank with your non-dominant hand; keeping your other hand flat, depress the palpating digits just below and anterior to the 11th and 12 ribs and ask the patient to take a deep breath. A normal healthy spleen should not be palpable." [10]
- Patient Education: Most splenic ruptures can be rapidly progressing, while others can delay haemorrhage for hours, days, or even weeks after injury until a sufficient enough force causes a rupture. It is vital that we educate patients about the signs and symptoms so they can seek medical care immediately.
- Post-operation: Encourage ROM, ambulation, and coughing techniques (splinted coughing). Most traumatic splenic ruptures will not be seen in physical therapy.
Differential Diagnosis[edit | edit source]
- Left kidney trauma/pathology
- Rib fracture
- Intestinal pathology
- Musculoskeletal Involvement
- Non-Hodgkin's Lymphoma
- Infectious Mononucleosis aka Epstein-Barr Virus
Case Report/ Case Study[edit | edit source]
Spontaneous rupture of the spleen – a fatal complication of pregnancy
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Kapila V, Tuma F. Physiology, Spleen. InStatPearls [Internet] 2020 Mar 26. StatPearls Publishing.Available from;https://www.ncbi.nlm.nih.gov/books/NBK537307/ (accessed 1.12.2020)
- ↑ Mike Flores Physical therapy management - ruptured spleen Available from https://www.youtube.com/watch?v=gip3fDb5O3E
- ↑ About Infectious Mononucleosis. Centers for Disease Control and Prevention. https://www.cdc.gov/epstein-barr/about-mono.html. Published September 14, 2016. Accessed April 5, 2017
- ↑ How Much Force to Rupture a Spleen: Sport Science. Available from: http://www.youtube.com/watch?v=uQp9iwVzN5Q [last accessed 30 November 2020]
- ↑ Mayo Clinic
http://www.mayoclinic.com/health/ruptured-spleen/DS00872 - ↑ A Dictionary of Nursing. 2008. Kehr’s Sign. 29 Mar. 2012 Available at: http://www.encyclopedia.com/doc/1O62-Kehrssign.html.
- ↑ Med School Made Easy Kehr Sign - Spleen Exam Available from https://www.youtube.com/watch?v=UkXghZn2WJ8
- ↑ WebMD. 2005-2012. Ruptured Spleen. [Internet] [reviewed 2009 Aug 19; cited 2012 Mar 30]. Available from: http://www.webmd.com/digestive-disorders/ruptured-spleen
- ↑ Examination of the Spleen. Examination of the Spleen | Stanford Medicine 25 | Stanford Medicine. http://stanfordmedicine25.stanford.edu/the25/spleen.html. Accessed April 4, 2017.
- ↑ 10.0 10.1 Shultz SJ, Houglum PA, Perrin DH. Examination of Musculoskeletal Injuries, 2nd ed. Champaign, IL, 2005. p. 570-571