Respiratory Management in Spinal Cord Injury: Difference between revisions
No edit summary |
No edit summary |
||
| Line 242: | Line 242: | ||
* Breath stacking (or air-stacking): three to six inspiratory breaths before exhalation. This technique can be conducted by the individual [[Active Cycle of Breathing Technique|actively]] performing [[Breath Stacking|breath stacking]] (respiratory sniff or inspiratory hold techniques) as well as through using a resuscitation bag with a mouthpiece or facemask.<ref name=":2" /><ref name=":4" /> | * Breath stacking (or air-stacking): three to six inspiratory breaths before exhalation. This technique can be conducted by the individual [[Active Cycle of Breathing Technique|actively]] performing [[Breath Stacking|breath stacking]] (respiratory sniff or inspiratory hold techniques) as well as through using a resuscitation bag with a mouthpiece or facemask.<ref name=":2" /><ref name=":4" /> | ||
* Active Cycle of Breathing (ACBT): allows sputum clearance from the lungs. Consists of 3 phases: gentle relaxed breathing, deep breathing, and huffing (small-long and big-short)<ref>Association of Chartered Physiotherapists in Respiratory Care.The Active Cycle of Breathing Techniques. Available at https://www.acprc.org.uk/Data/Publication_Downloads/GL-05ACBT.pdf (last accessed 14.02.2022)</ref> | * Active Cycle of Breathing (ACBT): allows sputum clearance from the lungs. Consists of 3 phases: gentle relaxed breathing, deep breathing, and huffing (small-long and big-short)<ref>Association of Chartered Physiotherapists in Respiratory Care.The Active Cycle of Breathing Techniques. Available at https://www.acprc.org.uk/Data/Publication_Downloads/GL-05ACBT.pdf (last accessed 14.02.2022)</ref> | ||
* Autogenic Drainage: breathing at low, mid and high lung volume to mobilise, collect and evacuate mucus, followed by forced expiratory techniques<ref name=":5">Massery, M. "If You Can't Breathe, You Can't Function" continuing education class 20 hrs. Feb 21-23, 2008. Rehabilitation Institute of Chicago, Chicago, IL. | * Autogenic Drainage: breathing at low, mid and high lung volume to mobilise, collect and evacuate mucus, followed by forced expiratory techniques<ref name=":5">Massery, M. "If You Can't Breathe, You Can't Function" continuing education class 20 hrs. Feb 21-23, 2008. Rehabilitation Institute of Chicago, Chicago, IL. </ref> | ||
{{#ev:youtube|v=a3n0l7vQTag}}<ref>Cork University Hospital. Breath Stacking Techniques. 2019. Available from: https://www.youtube.com/watch?v=a3n0l7vQTag [last accessed 15/02/2022]</ref> | {{#ev:youtube|v=a3n0l7vQTag}}<ref>Cork University Hospital. Breath Stacking Techniques. 2019. Available from: https://www.youtube.com/watch?v=a3n0l7vQTag [last accessed 15/02/2022]</ref> | ||
Revision as of 11:38, 18 February 2022
Original Editor - Eugenie Lamprecht
Top Contributors - Ewa Jaraczewska, Eugenie Lamprecht, Lucinda hampton, Jess Bell, Kim Jackson, Naomi O'Reilly, Vidya Acharya, Chelsea Mclene and Kirenga Bamurange Liliane
Introduction[edit | edit source]
Respiratory dysfunction is one of the most common medical complications, as well as the leading cause of reduced Quality of Life (QoL) and mortality among individuals with Spinal Cord Injuries.[1][2][3] Literature indicates that 67% of individuals with a spinal cord injury present with respiratory complications in the acute stage. [4] A retrospective review (Dec 2020) of the patients with acute traumatic spinal cord injuries at C5–T5 level during 2010–2015 shows a higher prevalence of respiratory complications during the initial hospitalisation just after the injury and suggests the presence of previous respiratory disease, complete motor impairment (AIS A–B) and coexistent thoracic trauma are a predictor of respiratory complications. Cervical and higher thoracic spinal cord injury are more prevalent to develop respiratory complications, primary due to diaphragm impairment. [1] The diaphragm is accountable for 65% of forced vital capacity and therefore plays a large role in ventilation.[3] In addition to muscular, other systems supporting ventilation include: skeletal, neurological and integumentary.
Early identification of patients with a spinal cord injury (SCI) who are at risk of respiratory complications might help clinicians to implement preventive strategies to reduce complications. [5]
Normal Respiration[edit | edit source]
In order to understand how respiratory functioning is affected among individuals with a spinal cord injury, it is important to understand how normal respiration occurs. The sequence of normal respiration includes the rise of the upper abdomen first, followed by lateral expansion of the lower chest, finished by a gentle rise of the upper chest in two planes: superior and anterior. Normal ventilation is possible due to the coordinated effort of many systems involved.
Primary systems involved in normal respiration:
- Musculoskeletal
- Neuromuscular
- Integumentary
- Other (Internal organs)
Musculoskeletal[edit | edit source]
Skeletal support for ventilation include :
- Anteriorly: ribs and sternum
- Posteriorly: thoracic spine and posterior ribs
During respiration upper ribs move primary anterior and superior, middle ribs move in all three planes of movement (anterior, superior and lateral), lower ribs move primarily lateral and superior. The greatest mobility of the rib cage occurs along the xiphoid process and the inferior borders of the anterior and lateral ribs. The thoracic spine allows mechanical alignment support for the rib cage.
Primary muscles of ventilation:
C3,4,5 keeps us alive!
- Diaphragm: innervated by the phrenic nerve C3-C5. In her role, the diaphragm provides up to 75% of tidal volume effort. It moves in all three planes and its function depends on the function of the intercostal and abdominal muscles, vocal cords and pelvic floor muscles. During quiet and forceful inhalation the diaphragm contracts concentrically. Controlled exhalation requires eccentric contraction of the diaphragm.
- Intercostals: innervated from T1-T2 levels. In their primary role, intercostals stabilise the rib cage during inhalation. During quiet and forceful inhalation and forceful exhalation, intercostals contract concentrically when controlled exhalation demands eccentric contraction. Note: patient with a spinal cord injury who has a tracheostomy tube, but is not able to tolerate a speaking valve cannot rely on this eccentric contraction to improve ventilation, because the tracheostomy tube allows the air to escape at will.[6]
- Abdominals: innervated from T6 to L1 levels. The primary role of the internal obliques is a downward pull on the inferior border of the rib cage. External obliques stabilises the inferior border of the rib cage. Transversus abdominis assists the diaphragm with maintaining positive pressure support.
Accessory muscles of ventilation
- Paraspinals: T1-S3 innervation, provide posterior stabilisation of the thorax allowing anterior chest expansion.
- Pectoralis Muscles: C5-T1 innervation, provide upper chest movement in 2 planes: anterior and lateral, act like rib stabilisers when intercostal muscles are paralysed.
- Serratus Anterior: C5-C7 innervation, with fixed upper extremity-assist with rib cage posterior expansion. The only inspiratory muscles that pair its function with trunk flexion.
- Scalenes: C3-C8 innervation, allows for superior and anterior movement of the upper chest
- Sternocleidomastoid: C2-C3 innervation and accessory cranial nerve, allows for superior and anterior movement of the upper chest
- Trapezius: C2-C4 innervation, allows for superior movement of the upper chest, must lift the weight of the upper extremity to assist with ventilation, highly inefficient muscle
Neuromuscular[edit | edit source]
The neurorespiratory system includes the cortex of the brain which is responsible for controlling voluntary breathing and the brainstem which controls automatic breathing. The spinal cord and motor neurons are also the elements of this system and are responsible for transmitting nerve impulses to the respiratory muscles closing the loop of the action of respiration. There is also a system of receptors and nerves regulating the process of ventilation.[8]
This video discusses the neuromuscular control of the respiration.
Integumentary (Skin)[edit | edit source]
Loss of elastic skin quality can cause deeper dysfunction affecting the spine and rib cage mobility. Scars and adhesions form as a result of inflammatory disease, burn, trauma or surgical incision can affect the quality of the tissue and its flexibility. The adhesions between the epidermis, dermis and fascia do not only stop at their level. Due to the continuity of the connective tissue throughout the body, the superficial restrictions can extend deeper restricting the mobility of the entire musculoskeletal system including fascia, tendons, muscles and joints. Study shows, that limited abdominal wall mobility, as well as mobility in the upper and lower chest, correlates with lower lung function.[10]
Spinal Cord Injury and Respiration[edit | edit source]
Traumatic and non-traumatic (tumour, vascular accident, abscess, transverse myelitis) spinal injuries can affect respiration due to impaired motor control of the respiratory muscles. Long term ventilation may be required with high cervical (C3 and above) spinal cord injury. Injuries below C3 level may or may not require ventilatory support, while patients with injuries below C5 may be able to breathe independently of continuous ventilator support. [8]
The following table illustrates the level of neurological injury relevant to impairment;[1][2]
| Neurological level | Impairment |
|---|---|
| C1-3 | Full Ventilator Dependent |
| C3-4 | Periods of Unassisted Ventilation
Diaphragm Impaired - ↓ Tidal Volume & Vital Capacity |
| C5 | Independent Ventilation
Initial Ventilatory Support Diaphragm Intact Intercostals and Abdominal Muscles Impaired - ↓ Lung Volumes and Forced Expiration for effective secretion clearance |
| C6-8 | Independent Ventilation
Diaphragm Intact Intercostals and Abdominal Muscles Impaired - ↓ Lung Volumes and Forced Expiration for effective secretion clearance Uses Accessory Muscles to generate an effective cough |
| T1-4 | Independent Ventilation
Diaphragm Intact Intercostals Intact - Normal Lung Volumes Abdominal Muscles Impaired - ↓ Forced Expiration for effective secretion clearance |
| T5-12 | Ventilation near equal or equal to individuals without spinal cord injury |
Respiratory Complications[edit | edit source]
The type and the extent of the respiratory complications depend on the level of injury and the degree of impairment. It can affect 80% of patients with a spinal cord injury during acute hospitalisation and continues through the post-acute and chronic phases of the spinal cord injury rehabilitation.[11]Possible complications include:
- Hypoventilation
- Reduced Surfactant Production
- Respiratory Failure[11]
- Mucus Plugging
- Atelectasis
- Pneumonia[11][12]
- Pulmonary Oedema
- Pulmonary Embolism
- Sleep-Disordered Breathing and Sleep Apnoea Syndrome [1][2]
Problem with ventilation and the above listed respiratory complications in individuals with a spinal cord injury can be related to:
- difficulties with productive cough and clearance of secretions
- excessive mucus production
- spastic contraction of the abdominal muscles
- restricted position and mobility limitation due to wearing the orthosis
Cough and Secretions[edit | edit source]
Patients' difficulties with cough and clearance of secretions can be observed with cervical, thoracic and high lumbar spinal injuries. These two functions depend on intercostal and abdominal muscles engagement which are innervated at T1-L1 levels.
Mucus Production[edit | edit source]
Another common complication that occurs among patients with quadriplegia is excessive bronchial mucus production. The cause of this is still uncertain but is thought to be due to reduced vagal nerve activity, which leads to a parasympathetic imbalance that causes:
- Bronchial Spasm
- Increased Vascular Congestion, and
- Decreased Mucociliary Activity (related to mechanical ventilation)[1]
Spastic Contraction of Abdominal Muscles[edit | edit source]
After the spinal shock phase, abnormal spinal reflexes may lead to spastic contraction of abdominal muscles. This increases difficulties with ability to breathe and may lead to dyspnea.[1]
Position and Orthosis[edit | edit source]
Erect positions can negatively affect ventilation due to a flattened diaphragm and the forward movement of abdominal content due to weak abdominal muscles. Wearing an abdominal binder can assist with breathing in upright positions.[1]
Acute Respiratory Management[edit | edit source]
The role of the members of the medical team varies in many aspects of the respiratory management of patients with a spinal cord injury. It often depends on the policies and procedures established by each country professional organisations.
Monitoring[edit | edit source]
During the acute phase of the spinal cord injury, the entire hospital multidisciplinary team can be responsible for monitoring the following:
- Diaphragmatic Function
- Pulse Oximetry
- Arterial gasometry
These markers indicate the need for patient's intubation:
- VC below 15mL/kg
- Maximum Inspiratory Pressure below -20cmH2O
- Increased pCO2[2]
Ventilation, Weaning and Extubation[edit | edit source]
The medical team including the neurologist, anesthesiologist, respiratory therapist, nurse and physiotherapist decides on the ventilation settings to meet the specific respiratory needs of every individual with a spinal cord injury. Chest physiotherapy performed by the respiratory therapist, nurse and/or physiotherapist is a key element in the post-extubation procedure.
Tracheostomy and Decannulation[edit | edit source]
Individuals with a spinal cord injury who develop respiratory complications or have a high level of complete spinal cord injury are likely to receive a tracheostomy. When decannulation is considered it is important for the entire multidisciplinary team to assess the airway patency, cough and swallowing effectiveness as well as oxygen requirements, medical stability, patient co-operation, oxygen dependence and infection markers[1][2].
Physiotherapy Management of Respiration[edit | edit source]
Patient Assessment[6][edit | edit source]
- Observation and Palpation
- observe and palpate breathing patterns by looking at the chest from the anterior and posterior view (upper, middle and lower chest expansion)
- observe and palpate trunk muscles alignment including neck and shoulder, intercostals, pectoralis, abdominals, quadratus, and posterior trunk muscles. Watch for tightness, function during inspiration and expiration, function while the patient lifts the head or attempts to get out of bed.
- observe ribs spacing and function: side-bending, rib separation, symmetry in static and dynamic situations.
- Objective measurement
- chest wall excursion using a tape measure
- Listening
- Auscultation of breaths sounds
- Quality of phonation, including syllabus per breath and changes in voice
- Cough effectiveness in each of four phases of cough: inspiration phase, hold phase, force phase, and expulsion phase.
- Finding the problem and choosing the action plan: the problem may be with secretions mobilisation (from the lungs up), secretions expectoration (from the lower airway up), or secretion management (movement away from the trachea to avoid aspiration).
Positioning[edit | edit source]
For individuals with compromised respiratory systems, proper positioning is a key to influencing breathing patterns and improving ventilation. A person with a spinal cord injury may need to rely on accessory muscles to breathe, including recruitment of trunk muscles for inspiration and expiration. When trunk muscles are too weak to support upright sitting, proper wheelchair seating and positioning is needed to optimise respiration and facilitate the use of accessory muscles. [13]
- Crytzer et al. (2018) suggested back support with air cells inside over rigid back. Air cells allow for trunk and rib cage expansion. [13]
- Back support should fit each person to optimise posture and function.[14]
- Footrest adjustment can facilitate upper chest or diaphragm breathing: lower foot support promotes anterior pelvis tilt promoting upper chest breathing and higher foot support promotes posterior pelvis tilt promoting diaphragm breathing. [6]
- Armrests, arm trough vs. lab tray: first one position upper extremities in the abduction and external rotation (upper chest respiration) and the latter position them in adduction and internal rotation (diaphragm respiration)
- Towel roll placed horizontally (under the ischium) or in a perpendicular direction (along the spine) opens up the anterior chest wall and facilitate upper chest breathing
- Soft or rigid supports assist with head, trunk and pelvis alignment and can include: abdominal binder, lateral trunk support, head support.[6]
Techniques[edit | edit source]
Secretion Mobilisation[edit | edit source]
A person with a spinal cord injury have difficulties with secretion mobilisation due to expiratory muscle weakness: external oblique, internal oblique, rectus and transverse. Adequate hydration is an important element in the effective mobilisation of secretion. Patients must receive enough fluids to meet the criteria for good hydration which is often assessed by the colour of the urine (pale green-yellow vs. dark orange when dehydrated).
Primary interventions used for secretion mobilisation include:
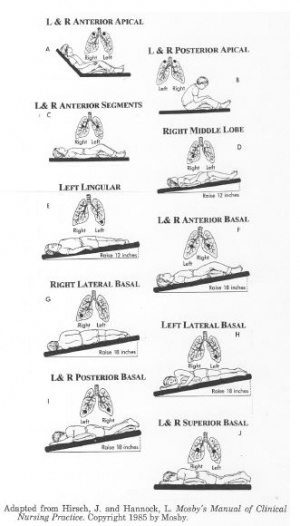
- postural drainage
- suctioning
- assisted coughing techniques
- percussions and vibrations
- mechanical insufflation and exsufflation.
Postural Drainage[edit | edit source]
Postural drainage is a gold standard of airway clearance. It can be used during daily routines of rest and sleep. Chosen positions will allow gravity to assist the movement of secretions towards the upper airway for removal via coughing or suctioning. Duration of postural drainage can vary from 5 to 10 minutes. [1]
Suctioning[edit | edit source]
Suctioning is an invasive procedure that allows clearance of secretions only in the large airways. Despite being very effective this technique is traumatic to the soft tissue of the airways.[6]Clinical condition of the patient must be considered when secretions clearance via suctioning is chosen. [15]
You can read about the indications, preparation, and technique needed to perform suctioning procedure here.
Assisted Coughing Techniques[edit | edit source]
- Manual cough assist: a person assisting the individual with a spinal cord injury presses the lower portion of the ribcage on both sides or under the diaphragm while the patient tries to cough. This is a synchronized inward and upward manual force to create intra-abdominal pressure for an effective forceful cough. This manual force will facilitate the intercostal and abdominal muscles to increase the intra-abdominal pressure necessary for an effective cough.[1][2]
- «Frog-breathing» technique (glossopharyngeal breathing): after 6 – 9 cycles of breathing out or coughing the patient uses gulping swallowing movements to push small volumes of air down into the lungs.
Percussions and Vibrations[edit | edit source]
Percussions and vibrations are manual techniques used to loosen secretions by causing vibrations in the chest wall. Important precautions and contraindications need to be taken into account prior to execution.
Contraindications include;
- Cardiovascular Instability
- Tension pneumothorax
- Active Pulmonary Tuberculosis (TB)
- Pulmonary Embolism (PE)
- Severe Pleural Effusion
- Unstable Spinal and / or Cranial Fractures
- Fractured Ribs
- Chest Wounds
- Acute Haemoptysis
- Increased Intracranial Pressure (ICP)[1]
Mechanical Insufflation and Exsufflation[edit | edit source]
This technique uses a cough assist device via a face mask or a tracheostomy tube to push the air into the lungs and then the secretion is suctioned out.
Specialised Breathing Techniques[edit | edit source]
- Breath stacking (or air-stacking): three to six inspiratory breaths before exhalation. This technique can be conducted by the individual actively performing breath stacking (respiratory sniff or inspiratory hold techniques) as well as through using a resuscitation bag with a mouthpiece or facemask.[2][11]
- Active Cycle of Breathing (ACBT): allows sputum clearance from the lungs. Consists of 3 phases: gentle relaxed breathing, deep breathing, and huffing (small-long and big-short)[20]
- Autogenic Drainage: breathing at low, mid and high lung volume to mobilise, collect and evacuate mucus, followed by forced expiratory techniques[6]
Stretching Techniques[edit | edit source]
In supine or side-lying:
- Passive stretch of the rib cage in side-lying or supine over the pillow under the rib cage or the towel roll along the spine
- Active stretch using upper extremity passive movements in abduction with external rotation paired with inspiration and adduction with internal rotation paired with expiration.
In sitting or supine:
- shoulder pinches with inhalation
- eyes and head move up with passive or active trunk extension paired with inspiration
- eyes and head move down with passive or active trunk flexion paired with expiration
- passive or active trunk rotation with head movement. The physiotherapist instructs the patient to look over the shoulder and inhale as the clinician passively or actively move the patient's arm(s) up and back. On the way back, the arm(s) is moved down towards the opposite knee while the patient exhales. The goal is to activate intercostals and oblique muscles.[6]
Soft tissue release[edit | edit source]
Myofascial release for intercostals, quadratus lumborum, abdominals, pectoralis
Respiratory Muscle Training[edit | edit source]
Respiratory Muscle Training involves one-way valves to target either inspiratory or expiratory muscles.[24][25]. The ventilatory muscle trainers (VMTs) are divided into:
- inspiratory trainers (P-flex, Threshold IMT, The Breather), and
- expiratory trainers (Resistex, Threshold PEP, The Breather)
Non-Invasive Ventilatory (NIV) Support[edit | edit source]
This technique applies positive pressure in the airways and is known as positive-pressure support. Examples of positive-pressure support devices are; CPAP, BPAP and IPPB. Individuals should be cooperative and the preferred technique should be conducted during day time via a mouthpiece and at night time, via a nosepiece. NIV support is also known to be used for initial ventilatory support or weaning and as night support.
Early Mobilisation[edit | edit source]
This is an effective technique in secretion clearance and improving ventilation.[25] Physiotherapists can assist individuals with a spinal cord injury to sit up in a chair once the spinal fractures are surgically stabilised. The early mobilisation has proven to accelerate recovery and reduce hospital stay. It is however extremely important for physiotherapists to consider using abdominal binders and slow progressive elevation during the spinal shock phase, as an individual with spinal cord injury may struggle with hypotension and increased work of breathing in the upright position. Antihypotensive medication can also be administered by the medical team if indicated.[2]
Long-Term Ventilation[edit | edit source]
Individuals with a spinal cord injury of C4 and higher often require long-term ventilatory support. Caregiver education and extensive training must be conducted by the entire multidisciplinary team. Frequent medical and physiotherapy assessments are advised in order to monitor the individual's condition.[27]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Galeiras Vázquez R, Rascado Sedes P, Mourelo Fariña M, Montoto Marqués A, Ferreiro Velasco ME. Respiratory management in the patient with spinal cord injury. BioMed research international. 2013;2013.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe. 2016 Dec 1;12(4):328-40.
- ↑ 3.0 3.1 Zakrasek EC, Nielson JL, Kosarchuk JJ, Crew JD, Ferguson AR, McKenna SL. Pulmonary outcomes following specialized respiratory management for acute cervical spinal cord injury: a retrospective analysis. Spinal cord. 2017 Jun;55(6):559-65.
- ↑ Hagen EM. Acute complications of spinal cord injuries. World journal of orthopedics. 2015 Jan 18;6(1):17.
- ↑ Sampol J, González-Viejo MÁ, Gómez A, Martí S, Pallero M, Rodríguez E, Launois P, Sampol G, Ferrer J. Predictors of respiratory complications in patients with C5–T5 spinal cord injuries. Spinal Cord. 2020 Dec;58(12):1249-54.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Massery, M. "If You Can't Breathe, You Can't Function" continuing education class 20 hrs. Feb 21-23, 2008. Rehabilitation Institute of Chicago, Chicago, IL.
- ↑ Scott Null. Normal Respiratory Cycle. 2009. Available from: https://www.youtube.com/watch?v=5L3dM3hinuo[last accessed 5/2/2022]
- ↑ 8.0 8.1 Benditt JO. The Neuromuscular Respiratory System: Physiology, Pathophysiology, and a Respiratory Care Approach to Patients. Respiratory Care Aug 2006, 51 (8) 829-839;
- ↑ Dr. Matt&Dr. Mike. Neural Control of Breathing | Respiratory System. 2019. Available from: https://www.youtube.com/watch?v=GqkMzds77f8[last accessed 7/2/2022]
- ↑ Kaneko H, Shiranita S, Horie J, Hayashi S. Reduced Chest and Abdominal Wall Mobility and Their Relationship to Lung Function, Respiratory Muscle Strength, and Exercise Tolerance in Subjects With COPD. Respir Care. 2016 Nov;61(11):1472-1480.
- ↑ 11.0 11.1 11.2 11.3 Tollefsen E, Fondenes O. Respiratory complications associated with spinal cord injury. Tidsskr Nor Laegeforen. 2012 May 15;132(9):1111-4.
- ↑ Raab AM, Mueller G, Elsig S, Gandevia SC, Zwahlen M, Hopman MT, Hilfiker R. Systematic Review of Incidence Studies of Pneumonia in Persons with Spinal Cord Injury. Journal of clinical medicine. 2022 Jan;11(1):211.
- ↑ 13.0 13.1 Crytzer TM, Hong EK, Dicianno BE, Pearlman J, Schmeler M, Cooper RA. Identifying characteristic back shapes from anatomical scans of wheelchair users to improve seating design. Med Eng Phys. 2016 Sep;38(9):999-1007.
- ↑ Halkiotis E, Mogul-Rotman B. B2: BACK IT UP! Back Supports’ Impact on Body Systems and Scapular Function. SYLLABUS. 2020 Mar 4:73.
- ↑ Pasrija D, Hall CA. Airway Suctioning. [Updated 2021 Sep 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557386/
- ↑ SpinalHub. How to assist cough a person with spinal cord injury. Available from: https://www.youtube.com/watch?v=lp-LBgD5Y5M [last accessed 3/10/2020]
- ↑ CANVent Ottawa. Glossopharyngeal Breathing. 2015. https://www.youtube.com/watch?v=9OswSaTG71I [last accessed 15/2/2022]
- ↑ Jack Thompson. Percussion, vibration and shaking for clearing secretions. Available from: https://www.youtube.com/watch?v=qr-FJ3RdGuQ [last accessed 3/10/2020]
- ↑ CANVentOttawa. Mechanical Insufflation-Exsufflation with a Tracheostomy. 2017. Available from: https://www.youtube.com/watch?v=mlc7Hk652UM [last accessed 15/02/2022]
- ↑ Association of Chartered Physiotherapists in Respiratory Care.The Active Cycle of Breathing Techniques. Available at https://www.acprc.org.uk/Data/Publication_Downloads/GL-05ACBT.pdf (last accessed 14.02.2022)
- ↑ Cork University Hospital. Breath Stacking Techniques. 2019. Available from: https://www.youtube.com/watch?v=a3n0l7vQTag [last accessed 15/02/2022]
- ↑ AdvancedTrainings. Intercostal Technique (Rib Bucket Handles) - Advanced Myofascial Techniques DVD Series. 2011. Available from: https://www.youtube.com/watch?v=I9LvnpTqWAI[last accessed 16/02/2022]
- ↑ John Gibbons. Myofascial release treatment for the Pectorals and Subscapularis using Soft Tissue Release (STR). 2014. https://www.youtube.com/watch?v=0EfmqYgl7zM [last accessed 15/2/2022]
- ↑ Tamplin J, Berlowitz DJ. A systematic review and meta-analysis of the effects of respiratory muscle training on pulmonary function in tetraplegia. Spinal Cord. 2014 Mar;52(3):175-80.
- ↑ 25.0 25.1 Wang HC, Lin YT, Huang CC, Lin MC, Liaw MY, Lu CH. Effects of respiratory muscle training on baroreflex sensitivity, respiratory function, and serum oxidative stress in acute cervical spinal cord injury. Journal of Personalized Medicine. 2021 May;11(5):377.
- ↑ NIck Smith.CPAP and Non-Invasive Ventilation in 5 minutes. 2015. Available from: https://www.youtube.com/watch?v=OHQK5PUTQ_0 [last accessed 16/02/2022]
- ↑ Schreiber AF, Garlasco J, Vieira F, Lau YH, Stavi D, Lightfoot D, Rigamonti A, Burns K, Friedrich JO, Singh JM, Brochard LJ. Separation from mechanical ventilation and survival after spinal cord injury: a systematic review and meta-analysis. Ann Intensive Care. 2021 Oct 24;11(1):149.