Neuropathies: Difference between revisions
Candace Goh (talk | contribs) mNo edit summary |
Candace Goh (talk | contribs) mNo edit summary |
||
| Line 51: | Line 51: | ||
* [[Timed Up and Go Test (TUG)|TUG]]; [[10 Metre Walk Test|10 metre walk test]]; [[Grip Strength]]; [[Fatigue Severity Scale|Fatigue Severity Scale;]] [[Patient Specific Functional Scale]]; [[Muscle Strength|Oxford Muscle Strength Scale]]; [[Romberg Test|Romberg Test]]. | * [[Timed Up and Go Test (TUG)|TUG]]; [[10 Metre Walk Test|10 metre walk test]]; [[Grip Strength]]; [[Fatigue Severity Scale|Fatigue Severity Scale;]] [[Patient Specific Functional Scale]]; [[Muscle Strength|Oxford Muscle Strength Scale]]; [[Romberg Test|Romberg Test]]. | ||
== Management / Interventions == | == Management / Interventions == | ||
Besides [[Pain Medications|medications]] used to treat conditions associated with peripheral neuropathy, medications used to relieve peripheral neuropathy signs and symptoms include:<ref name=":1" /> | [[File:Pill banner.png|right|frameless]]Besides [[Pain Medications|medications]] used to treat conditions associated with peripheral neuropathy, medications used to relieve peripheral neuropathy signs and symptoms include:<ref name=":1" /> | ||
'''Anticonvulsants:''' Gabapentin; Pregabalin; Valproate | '''Anticonvulsants:''' Gabapentin; Pregabalin; Valproate | ||
Revision as of 05:47, 27 July 2020
Top Contributors - Lucinda hampton, Kim Jackson, Candace Goh, Melissa Coetsee, Uchechukwu Chukwuemeka, Manisha Shrestha, Merinda Rodseth, Ahmed M Diab and Sehriban Ozmen
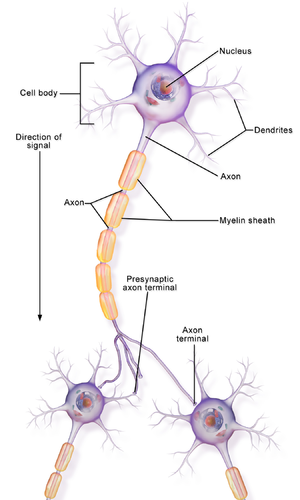
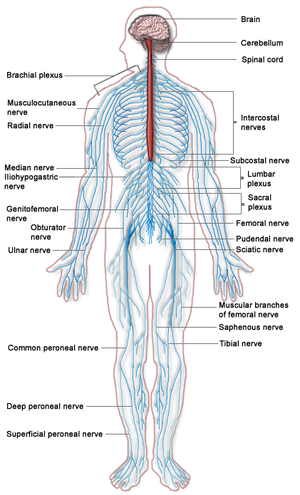
Clinically Relevant Anatomy[edit | edit source]
Neuropathy is a dysfunction of one or more peripheral nerves or peripheral nervous system.
Neuropathy can involve damage of only one nerve (called mononeuropathy); two or more nerves in different areas, called mononeuropathy multiplex; or most commonly, many nerves are affected (called polyneuropathy)[1].
Mechanism of Injury / Pathological Process[edit | edit source]
The causes of neuropathies are manyfold and include:
- Physical injury e.g. pressure from disc herniation, pressure from a cast, trauma, arthritis.
- Diabetes
- Autoimmune diseases e.g. Guillain-Barre Syndrome, Sjogren's Syndrome, Lupus, Rheumatoid Arthritis (RA)
- Toxins e.g. from toxic amounts of substances in the blood associated with kidney and liver disorders, alcoholism, chemotherapy drugs
- Infections e.g. chicken pox, Varicella zoster virus (shingles), White Nile virus, AIDS, Lyme disease (carried by ticks), Epstein-Barr virus, hepatitis C[2]
Neuropathies may primarily affect sensory nerves, motor nerves, autonomic nerves, or multiple types. Anything that damages nerves can interfere with their ability to transmit accurate signals, which can lead to a number of signs and symptoms.
Clinical Presentation[edit | edit source]
Neuropathies may primarily affect sensory nerves, motor nerves, autonomic nerves, or multiple types. Anything that damages nerves can interfere with their ability to transmit accurate signals, which can lead to a number of signs and symptoms.
Dependent on the type of nerves affected
- Motor nerve damage will cause muscle weakness, painful cramps, fasciculations (uncontrolled muscle twitching visible under the skin) and muscle atrophy.
- Sensory nerve damage causes various symptoms because sensory nerves have a broad range of functions. Damage to large sensory fibers affects the ability to feel vibrations and touch. The client may feel as if she/he is wearing gloves and stockings. This damage may contribute to the loss of reflexes (along with motor nerve damage). Loss of position sense presenting with e.g. balance problems. The damage of “small fibers” (without myelin sheaths) affects the transmission of pain and temperature sensations which interferes with the ability to feel pain or changes in temperature. This causes neuropathic pain, which can erode a person's quality of life.
- Autonomic nerve damage affects the axons in small-fiber neuropathies. Common symptoms include, excess sweating, heat intolerance, inability to expand and contract the small blood vessels that regulate blood pressure, and gastrointestinal symptoms.[2]
Diagnostic Procedures[edit | edit source]
A full Medical History (including client symptoms, lifestyle, exposure to toxins, drinking habits and a family history of nervous system (neurological) diseases).
Neurological examination
Other tests ordered include
- Blood tests, checking for e.g. toxins, vitamin deficiencies, diabetes
- Imaging test e.g. CT scans, MRI scans
- Nerve function tests, checking nerve conduction.
- Nerve biopsy, looking for abnormalities
- Skin biopsy, looking for reduction in nerve endings[3]
Outcome Measures[edit | edit source]
The many different presentations of neuropathies lead to a need to client specific outcome measures. Usually related to muscle strength, pain, QOL, and activity limitations. They include:
- The SF-36 is a measure of health status and an abbreviated variant of it, the SF-6D, is commonly used in health economics as a variable in the quality-adjusted life year calculation to determine the cost-effectiveness of a health treatment.[4]
- INCAT (inflammatory cause and treatment) score is a measure of activity limitation
- TUG; 10 metre walk test; Grip Strength; Fatigue Severity Scale; Patient Specific Functional Scale; Oxford Muscle Strength Scale; Romberg Test.
Management / Interventions[edit | edit source]
Besides medications used to treat conditions associated with peripheral neuropathy, medications used to relieve peripheral neuropathy signs and symptoms include:[3]
Anticonvulsants: Gabapentin; Pregabalin; Valproate
Antidepressants:Amitriptyline; Duloxetine; Venlafaxine
Opioids: Dextromethorphan; Morphine sustained release; Oxycodene; Tapentadol; Tramadol.
Others: Topical nitrate sprays; Capsaicin cream
Physiotherapy[edit | edit source]
The main role of Physiotherapy is to
- Restore, or maintain muscle strength, and prevent muscle shortening and deformity
- Balance, coordination and functional training.
- Pain relief e.g. provision of TENS, massage
- Splints as needed, prevent deformity and contractures
- Education, re-managing conditions, preventing damage and emotional support.
For a comprehensive guide see individual neuropathies below
- AIDS
- Anterior Interosseous Nerve Syndrome
- Axillary Nerve Injury
- Brachial Plexus Injury
- Benediction Hand
- Carpal Tunnel Syndrome
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
- Cubital Tunnel Syndrome
- Cyclist's Palsy
- Diabetic Neuropathy
- Double Crush Syndrome
- Lumbar Radioculopathy
- Multifocal Motor Neuropathy
- Nerve Entrapment
- Posterior Interosseous Nerve Syndrome
- Sciatic Nerve Injury
- Thoracic Radiculopathy
- Ulnar Nerve Entrapment
References[edit | edit source]
- ↑ Manipal hospitals. Types of neuropathies. Available from: https://www.youtube.com/watch?v=hYVtd3hB2_w (last accessed 18.4.2019)
- ↑ 2.0 2.1 NIH Peripheral neuropathy fact sheet. Available from: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet (last accessed 18 April 2019)
- ↑ 3.0 3.1 Mayo clinic. Peripheral neuropathy. Available from: https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/diagnosis-treatment/drc-20352067 (last accessed 18 April 2019)
- ↑ Wikipedia. SF-36 Available from: https://en.wikipedia.org/wiki/SF-36 (last accessed 19 April 2019)