Posterior Interosseous Nerve Syndrome
Original Editors - Lyn Bruyndonckx
Top Contributors - David Adamson, Thomas Longbottom, Admin, Kim Jackson, Alan Jit Ho Mak, Anas Mohamed, Evan Thomas, WikiSysop, Wanda van Niekerk and 127.0.0.1
Definition/Description[edit | edit source]
Posterior interosseous nerve syndrome is a neuropathic compression of the posterior interosseous nerve where it passes through the radial tunnel.[1] This may result in paresis or paralysis of the digital and thumb extensor muscles, resulting in an inability to extend the thumb and fingers at their metacarpophalangeal joints.[2] Wrist extension is preserved due to the action of the extensor carpi radialis longus innervated by the radial nerve.[3]
Clinically Relevant Anatomy[edit | edit source]
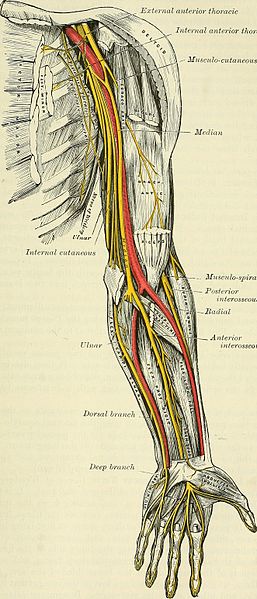
The posterior interosseous nerve is located close to shaft of the humerus and the elbow. This nerve is the deep motor branch of the radial nerve. Proximal to the supinator arch, the radial nerve is divided into a superficial branch and posterior interosseous branch. The radial nerve supplies the majority of the forearm and hand extensors. Damage to this branch of the radial nerve results in posterior interosseous nerve syndrome.
The radial tunnel is a space that extends 5cm from the radial head to the distal margin of the supinator. This tunnel is attached laterally to the brachioradialis, extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) and medially to the biceps tendon and brachialis. The floor is formed by the deep head of the supinator and the capsule of the radiocapitellar joint, while the roof is formed by the superficial head of the supinator and the radial recurrent vessels.[4]
At the level of the lateral epicondyle, between the brachioradialis and brachialis muscles, the radial nerve, which has its origin in the brachial plexus, divides into its 2 terminal branches: the superficial radial nerve and the posterior interosseous nerve.[5] The superficial radial nerve ends proximal to the radial tunnel. The posterior interosseous nerve is much longer and enters the radial tunnel underneath a musculotendinous arch, the arcade of Frohse. The arcade of Frohse, which is the most common point of compression, is a connection between the deep and superficial heads of the supinator and is fibrotendinous in 30% to more than 80% of the population.[6] The posterior interosseous nerve continues in the radial tunnel through the supinator, as it goes from the anterior to the posterior surface of the forearm.
The posterior interosseous nerve is a motor nerve and sequentially innervates supinator, extensor carpi radialis brevis, extensor digitorum communis, extensor digiti minimi, extensor carpi ulnaris, abductor pollicis, extensor pollicis brevis, extensor pollicis longus, and extensor indicis.[4][7]
Epidemiology/Etiology[edit | edit source]
Posterior interosseous nerve syndrome is more common in males, manual labourers and bodybuilders, with an incidence of 3 per 100 000.[8] With a humeral shaft fracture, there is a 12% chance of associated with radial nerve paralysis.[9]Proximal forearm fractures can also result in posterior interosseous nerve palsy.[10]
Posterior interosseous nerve syndrome can be caused by a traumatic injury, tumors, inflammation and an anatomic injury. With repeated pronation and supination a dynamic compression of the nerve in the proximal part of the forearm can be created.[11]
Posterior interosseous nerve syndrome usually develops spontaneously[1] and is caused by compression injuries to the upper extremity, mostly in the arcade of Frohse[12]. It is the area where the nerve enters the supinator muscle[13] and is the most common place for a compression of the nerve. However, it can also occur following trauma, such as a blow to the proximal dorsal region of the forearm. Impingement of the radial nerve results in posterior interosseous nerve syndrome.[9] Compression of the posterior interosseous nerve is associated with repetitive activities that involve gripping, wrist supination and pronation, with a component of wrist extension.[14]This diagnosis may be associated with lateral epicondylitis.[15]
Posterior interosseous nerve syndrome can be iatrogenic following reduction of radial fracture, transposition of the ulnar nerve or release of the extensor origin for lateral epicondylitis.[1] Although less common, it can also follow surgical reinsertion of a ruptured distal biceps brachii tendon.[16] The causes of posterior interosseous nerve syndrome include intrinsic nerve abnormalities and extrinsic compression.[17]
Characteristics/Clinical Presentation[edit | edit source]
A patient who presents with this diagnosis of posterior interosseous syndrome may have a history of vague proximal posterior forearm pain with no weakness in more mild cases. In more severe cases, the patient may present with weakness in the wrist and finger extensors. Because the extensor carpi radialis longus and in some cases the extensor carpi radialis brevis are innervated before the radial nerve passes into the supinator, there is usually some sparing of wrist extension. Also, because of the lack of extensor carpi ulnaris, there maybe some radial deviation of the wrist with extension with the remaining innervated ECRL and ECRB.[18][19]
Most nerve entrapments occurs due to an osseoligamentous tunnel narrowing. In the case of a posterior interosseous nerve entrapment, the compression occurs within the musculotendinous radial tunnel. In 69.4%, the nerve is compressed by the fibrous arcade of Frohse.[20]
There is a very slow development of the symptoms. The duration of symptoms averaged 2-3 years before a definitive diagnosis could be made.[11] Symptoms of nerve entrapment syndromes are generally involving pain, sensory and motor changes, sensations of popping, paresthesias, and paresis. There will be no sensory loss as this nerve carries motor fibers only.
Posterior interosseous nerve syndrome is characterized by motor deficits in the distribution of the posterior interosseous nerve.[20] While the posterior interosseous nerve does have afferent fibres that transmit pain signals from the wrist, it does not carry any cutaneous sensory information that can help distinguish a posterior interosseous nerve palsy from cervical radiculopathy. The clinical presentation of posterior interosseous nerve syndrome is characterized by the loss of function due to variable degrees of weakness involving ulnar deviation.
Differential Diagnosis[edit | edit source]
Posterior interosseous nerve syndrome is one of the pathologies that can cause lateral elbow pain (lateral epicondylitis). In early stages, both diagnosis may present with similar presentations with dorsal forearm pain and pain with resisted wrist extension. The patient who presents with posterior interosseous syndrome may have subtle finger extension and thumb extension weakness. The use of a lidocaine injection may aid in the diagnosis of lateral epicondylitis as it should significantly decrease pain in this diagnosis for a temporary period of time. Compression or injury of the radial nerve may occur along its course on the posterior side of the humerus in the radial groove from humeral shaft fractures or as it winds to the anterior side of the lateral epicondyle from epicondylar fractures.[21][22]
The other pathologies that are associated with lateral elbow pain are:
- Pigmented villonodular synovitis[1]
- Lateral epicondylitis[5]
- Radial nerve injury/palsy[5]
- Cervical radiculopathy[5]
- Extensor carpi radialis brevis tendinosis[7]
- Cervical spine C5-C7[7]
- Extensor tendon rupture[23]
- Trigger finger
- Sagittal band ruptures
- Inflammatory involvement of the metacarpophalangeal joints
- Anconeus muscle tendonitis[24]
- Supinator syndrome[24]
- Brachialis neuritis[24]
- Arthritis/arthrosis of the radiohumeral joint
- Meniscus of the radiohumeral joint
- Olecranon bursitis
- Neuralgic amyotrophy
- Rupture of the intermetacarpal space[23]
- Wartenberg's disease (sensory only)
Diagnostic Procedures[edit | edit source]
Careful clinical and electrophysiological examination is important and essential for a reliable diagnosis.[13]
Physical examination[edit | edit source]
- History
- Functional limitations or deficits
- Palpation: Abnormal tenderness is expected over the arcade of Frohse and eventually over the lateral epicondyle
- Neural tension test
- Muscle testing (with resistance):[4][25] There is partial or complete paralysis of the wrist extensors:
- The patient is unable to extend the thumb and other fingers of the affected side at the metacarpophalangeal joints
- Wrist extension is possible, typically in a radially deviated direction, due to the preservation of the extensor carpi radialis longus and the weakened extensor carpi ulnaris
- Resisted supination and pronation of the forearm can produce pain, as well as resisted extension of the middle finger
- The brachioradialis and the extensor carpi radialis longus are innervated by more proximal branches of the radial nerve, so may be spared
Special investigations[edit | edit source]
The following special investigations are used to assist in making the diagnosis.[1] It further aids to establish the topography of the lesion and the severity of the muscular denervation.[13]
- Electromyography: Identify level of compression
- Nerve conduction velocity
- MRI: Not commonly used:
- To determine specific area of compression
- Assist in surgical planning
Outcome Measures[edit | edit source]
Medical Management[edit | edit source]
There are several medical ways to treat the posterior interosseous nerve syndrome.
Conservative management[edit | edit source]
- Reduction of local inflammation and swelling around the nerve:[26]
- Wrist and/or elbow splints
- The arm can be put in an above-elbow cast for ten days with the elbow flexed at 90°, the forearm supinated and the wrist in neutral position[27]
- In cases with more significant weakness, extension assist outrigger component maybe added to aid in passive finger extension for improved hand function.
- NSAID’s
- Activity modification to reduce local inflammation and swelling around the nerve
- Wrist and/or elbow splints
- Corticosteroid injections[27]
- Therapeutic ultrasound[27]
- Physiotherapy[27]
- Reduction of synovitis:[28]
- Heat
- Rest
- Mild range of motion
Surgery[edit | edit source]
- Indication:
- No improvement with conservative management after 3-6 months
- Pain present after 12 weeks
- Surgical decompression may be indicated to prevent further nerve damage.
- Aim: To obtain full recovery
- Recovery and outcomes: Will depend on the extent of nerve damage with the vast majority of neuropraxic problems resolving. Treatment of a patient after they have a decompression includes a gradual return to activities over a 6 weeks period.
- Surgery: Depends on how and where impingement is present[28][29]
- Arcade of Frohse release
- Resection of lesions
- Posterior interosseous nerve release
- Release of superficial radial nerve
- Lengthening of supinator
- Synovectomy
Physiotherapy Management[edit | edit source]
Conservative management[edit | edit source]
3-6 months of physiotherapy with regular re-assessment of signs and symptoms is recommended. If there is no response to therapy, evidence of denervation, or persistent paralysis, surgical decompression should be considered.[20]
Physiotherapy should include a multimodal approach. The following can be considered based on the patient presentation:
- Cryotherapy: Increase extensibility and reduce tone of local muscles
- Ultrasound
- TENS
- Deep tissue massage and stretching exercises: Improve extensibility of the muscles who surround the brachial plexus and radial nerve
- Focus on:[30]
- Thoracic outlet
- Pectoralis minor
- Triceps
- Brachioradialis
- Supinator
- Extensor carpi radialis longus and brevis
- Focus on:[30]
- Dry needling: Increase extensibility and reduce tone of local muscles
- Neural mobilizations:[30]
- Reduce mechanical extra- and intra-neural adhesion
- Assist the neuromodulation of symptoms
- Manual therapy[9]: Regain elbow mobility
- Strengthening[20] and range of motion exercises
- Stretching exercises:
- Focus on supinator
- Passive wrist extensions stretches:
- Place hand on table and move upper body over wrist
- Prayer stretch
Post-surgical rehabilitation[edit | edit source]
- Commence active range of motion from day 3-5
- Incorporate stretching of extensors
- Commence strengthening from week 3-4
Patients can return to light duty work between week 2 and 3 post-operatively, while return to baseline function can take between 6 and 12 weeks.[31]
Clinical Bottom Line[edit | edit source]
The posterior interosseous nerve is the deep branch stemming from the radial nerve. Compression can be caused by trauma, repetitive strain and inflammation. This is then known as posterior interosseous nerve syndrome, which may result in paresis or paralysis of the digital and thumb extensor muscles, resulting in an inability to extend the thumb and fingers at their metacarpophalangeal joints. Conservative management includes splinting, NSAID's and physiotherapy, and symptoms normally resolve within 3-6 months. Failed conservative management is an indication for surgery, where nerve releases are the most common surgical intervention. Physiotherapy also plays a big part in the post-operative management, and rehabilitation generally lasts between 6 and 12 weeks.
Key Evidence[edit | edit source]
- Interventions for treating the posterior interosseus nerve syndrome: a systematic review of observational studies.
- Ultrasonographic evaluation of the iatrogenic peripheral nerve injuries in upper extremity.
- Median and radial nerve compression about the elbow. A unified approach to radial tunnel syndrome and lateral tendinosis.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Vrieling C, Robinson PH, Geertzen JH. Posterior interosseous nerve syndrome: literature review and report of 14 cases. European journal of plastic surgery 1998;21(4):196-202.
- ↑ Chien AJ, Jamadar DA, Jacobson JA, Hayes CW, Louis DS. Sonography and MR imaging of posterior interosseous nerve syndrome with surgical correlation. American Journal of Roentgenology 2003;181(1):219-21.
- ↑ Wheeler R, DeCastro A. Posterior interosseous nerve syndrome [Internet]. National Center for Biotechnology Information. U.S. National Library of Medicine; 2021 [cited 2021Oct30]. Available from: https://pubmed.ncbi.nlm.nih.gov/31082090/
- ↑ 4.0 4.1 4.2 Cha J, York B, Tawfik J. Posterior interosseous nerve compression. Eplasty 2014;14.
- ↑ 5.0 5.1 5.2 5.3 Bevelaqua AC, Hayter CL, Feinberg JH, Rodeo SA. Posterior interosseous neuropathy: electrodiagnostic evaluation. HSS Journal 2012;8(2):184-9.
- ↑ Ozturk A, Kutlu C, Taskara N, Kale AC, Bayraktar B, Cecen A. Anatomic and morphometric study of the arcade of Frohse in cadavers. Surgical and Radiologic Anatomy. 2005 Aug 1;27(3):171-5.
- ↑ 7.0 7.1 7.2 Ekstrom RA, Holden K. Examination of and intervention for a patient with chronic lateral elbow pain with signs of nerve entrapment. Physical therapy 2002;82(11):1077-86.
- ↑ Ortho Bullets. PIN Compression Syndrome. Available from: https://www.orthobullets.com/hand/6023/pin-compression-syndrome (accessed 30/01/2019).
- ↑ 9.0 9.1 9.2 Quignon R, Marteau E, Penaud A, Corcia P, Laulan J. Posterior interosseous nerve palsy. A series of 18 cases and literature review. Chirurgie de la Main 2012;31(1):18-23.
- ↑ Bulstra LF, Schep NWL, Van Der Vlies CH. Posterior interosseous nerve palsy after closed proximal forearm fractures. Trauma Case Reports [Internet] 2019;23:100240. Available from: https://dx.doi.org/10.1016/j.tcr.2019.100240
- ↑ 11.0 11.1 Molina AP, Bour C, Oberlin C, Nzeusseu A, Vanwijck R. The posterior interosseous nerve and the radial tunnel syndrome: an anatomical study. International orthopaedics 1998;22(2):102-6.
- ↑ Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D. Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics 2006;26(5):1267-87.
- ↑ 13.0 13.1 13.2 Huisstede BM, Miedema HS, Van Opstal T, De Ronde MT, Kuiper JI, Verhaar JA, Koes BW. Interventions for treating the posterior interosseus nerve syndrome: a systematic review of observational studies. Journal of the Peripheral Nervous System 2006;11(2):101-10.
- ↑ Rosenbaum R. Disputed radial tunnel syndrome. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine 1999;22(7):960-7.
- ↑ Pecina M. Krmpotic-Nemanic J. Markiewitz A. Tunnel Syndromes Peripheral Nerve Compression Syndromes.New York.CRC Press.196
- ↑ Reichert P, Królikowska A, Witkowski J, Szuba Ł, Czamara A. Surgical management of distal biceps tendon anatomical reinsertion complications: Iatrogenic posterior interosseous nerve palsy. Medical science monitor: international medical journal of experimental and clinical research. 2018;24:782.
- ↑ Chien AJ, Jamadar DA, Jacobson JA, Hayes CW, Louis DS. Sonography and MR imaging of posterior interosseous nerve syndrome with surgical correlation. American Journal of Roentgenology 2003;181(1):219-21.
- ↑ Brotzman S, Wilk K, editors. Clinical Orthopedic Rehabilitation. 2nd edition. Philadelphia: Mosby, 2003
- ↑ Magee D. Orthopedic Physical Assessment. 3rd edition. Philadelphia.WB Saunders Company,1997
- ↑ 20.0 20.1 20.2 20.3 Saratsiotis J, Myriokefalitakis E. Diagnosis and treatment of posterior interosseous nerve syndrome using soft tissue manipulation therapy: A case study. Journal of bodywork and movement therapies 2010;14(4):397-402.
- ↑ Robson AJ, See MS, Ellis H. Applied anatomy of the superficial branch of the radial nerve. Clin Anat. Jan 2008;21(1):38-45.
- ↑ Thomsen NO, Dahlin LB. Injury to the radial nerve caused by fracture of the humeral shaft: timing and neurobiological aspects related to treatment and diagnosis. Scand J Plast Reconstr Surg Hand Surg. 2007;41(4):153-7.
- ↑ 23.0 23.1 Millender LH, Nalebuff EA, Holdsworth DE. Posterior interosseous-nerve syndrome secondary to rheumatoid synovitis. JBJS 1973;55(4):753-7.
- ↑ 24.0 24.1 24.2 Kaswan S, Deigni O, Tadisina KK, Totten M, Kraemer BA. Radial tunnel syndrome complicated by lateral epicondylitis in a middle-aged female. Eplasty 2014;14.
- ↑ Singh VA, Michael RE, Dinh DB, Bloom S, Cooper M. Posterior interosseous nerve syndrome from thermal injury. Case reports in surgery 2014;2014.
- ↑ Mansuripur PK, Deren ME, Kamal RO. Nerve compression syndromes of the upper extremity: diagnosis, treatment, and rehabilitation. Rhode Island Medical Journal 2013;96(5):37-9.
- ↑ 27.0 27.1 27.2 27.3 Maffulli N, Maffulli F. Transient entrapment neuropathy of the posterior interosseous nerve in violin players. Journal of Neurology, Neurosurgery & Psychiatry 1991;54(1):65-7.
- ↑ 28.0 28.1 Chang LW, Gowans JD, Granger CV, Millender LH. Entrapment neuropathy of the posterior interosseous nerve. A complication of rheumatoid arthritis. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology 1972;15(4):350-2.
- ↑ Hashizume H, Nishida K, Nanba Y, Shigeyama Y, Inoue H, Morito Y. Non-traumatic paralysis of the posterior interosseous nerve. The Journal of bone and joint surgery. British volume 1996;78(5):771-6.
- ↑ 30.0 30.1 Molloy J, Neville V, Woods I, Speedy D. Posterior interosseous nerve entrapment. RTS 2006;1(8):20-5.
- ↑ The Student Physical Therapist. Posterior interosseous nerve syndrome. Available from: https://www.thestudentphysicaltherapist.com/research-articles/posterior-interosseous-nerve-syndrome (accessed 30/01/2019).